 |
 |
| Korean J Intern Med > Volume 39(6); 2024 > Article |
|
See editorial "Impact of COVID-19 on end-stage kidney disease incidence and clinical practice" on page 872.
Abstract
Background/Aims
The corona virus disease 2019 posed a major risk for end-stage kidney disease (ESKD) cases. Our study aimed to assess changes in kidney replacement therapy (KRT) trends and healthcare access for these patients during the pandemic.
Methods
We retrospectively analyzed nationwide data from July 2017 to June 2022 to assess changes in KRT and ESKD incidence. KRT modalities included peritoneal dialysis (PD), hemodialysis (HD), and kidney transplantation (KT). We utilized the interrupted time series (ITS) method to compare changes in KRT modality before and after the incidence of the COVID-19 pandemic.
Results
ESKD incidence remained stable from 2018 to April 2022. The ITS analysis confirmed that the pandemic did not significant impact overall KRT incidence. PD cases decreased (5.7% to 1.3%), while HD cases increased (81.6% to 85%), and KT recipient remained relatively stable (12.7% to 17.3%). The hospitalization and hospital stay decreased in nursing hospital (165.01 days to 147.77 days) and general hospital (61.34 days to 55.58 days) during the pandemic, however, remained unchanged for PD and KT.
Conclusions
Our findings indicate no significant changes in ESKD incidence in South Korea during the pandemic. However, there were shifts in modality distribution, with decreased PD and increased HD cases. Notably, HD cases showed a significant reduction in hospital admissions and length of stay. The healthcare system demonstrated stability during the pandemic, with minimal disruptions in ESKD care.
The corona virus disease 2019 (COVID-19) was first recognized in December 2019 in Wuhan, China [1]. Owing to the surge in COVID-19 infections worldwide, many hospitals were forced to go into emergency mode, and this has prevented them from treating chronically ill patients and performing various procedures and surgeries in a timely manner. In this context, the significance of kidney replacement therapy (KRT) cannot be overstated. KRT is essential for sustaining life and must be provided at appropriate times. However, the COVID-19 pandemic has necessitated the adoption of changes in the methods and timing of administering KRT to patients.
Individuals with chronic kidney disease, especially those in the advanced stages, such as end-stage kidney disease (ESKD), have weakened immune systems and are at a higher risk of infection, including viral infections like COVID-19 [2]. Notably, patients undergoing KRT, including maintenance dialysis or kidney transplant (KT) cases, are particularly vulnerable to COVID-19 [3ŌĆō5]. Patients in need of KRT, particularly those undergoing hemodialysis (HD) and attending the dialysis center three times a week, face an elevated risk of contracting COVID-19 owing to their heightened exposure to healthcare facilities. Although several studies have reported on this concern [6], there is a scarcity of domestic research on this issue, necessitating an in-depth exploration.
We aimed to analyze data from the nationwide claims data in Korea to investigate the differences in ESKD incidence and changes in KRT modalities during the COVID-19 pandemic and compare these to the previous period. This study sought to determine whether COVID-19 has affected the incidence, choice of modality, and length of stay (LOS) of patients with ESKD, and whether this varied by hospital system. The acquisition of comprehensive epidemiological data on this concern would be instrumental in developing response strategies for the management of patients with ESKD in the face of future pandemics or similar infectious disease outbreaks.
This retrospective cohort study used South Korean nationwide data from July 2017 to June 2022 to analyze changes in the incidence of ESKD and the delivery of KRT during the COVID-19 pandemic. Specifically, we investigated whether there were differences in incidence rates during the COVID-19 period compared to the pre-pandemic period in 2019, utilizing the incidence rate ratio (IRR) and interrupted time series (ITS) analysis. This study was approved by the Institutional Review Board of Ajou University (IRB approval number: AJOUIRB-EX-2022-564) and all procedures were performed in accordance with the Declaration of Helsinki.
This study examined health insurance claims data from the Health Insurance Review and Assessment (HIRA) service, covering the period of July 2017 to June 2022(dataset: M20230103001). This dataset is national in scope because South Korea operates a universal coverage health insurance system with a 97% enrollment rate. This nationwide, real-world HIRA dataset comprises anonymized basic characteristics of individuals, including age and sex, as well as information on medical treatments and healthcare institutions [7]. To calculate the incidence rate per population, we obtained disease-free population data from Statistics Korea. The monthly and mid-year population values from the Statistics Korea dataset were used to determine the at-risk population [8].
The study population included incident patients with ESKD, identified from the International Classification of Diseases, Tenth Revision (ICD-10th) codes as well as procedure codes of insurance claims data. ESKD patients were categorized based on the KRT modality and age groups. Considering the KRT modality, patients were classified as undergoing HD, peritoneal dialysis (PD), or KT recipients. For HD and PD, patients who had at least one outpatient visit with ICD code ŌĆśN18ŌĆÖ and had KRT procedure codes for 3 months or more were defined as ESKD patients. For KT recipients, those with at least one outpatient visit with an ŌĆśN18ŌĆÖ code and KT procedure codes were considered ESKD patients. The procedure codes were O7020, O7021, and O9991 for HD; O7076 and O7077 for PD; and R3280 for KT [9].
Patients who underwent dialysis after KT were included in the dialysis group. For patients who received both HD and PD, the analysis was based on the most recent dialysis modality used. In terms of age, participants were grouped into five categories: under 18, 18ŌĆō44, 45ŌĆō64, 65ŌĆō74, and 75 years and above. To confirm that the ESKD cases were new, individuals with no KRT-related claims in the one-year period preceding their first KRT claim were defined as incident cases.
Since the incidence rates fluctuated from month to month, we computed the quarterly incidence rates, expressing them as both crude rates and age-standardized rates per 100,000 individuals [10]. The incidence rate was calculated by dividing the number of incident ESKD cases in a specific year by the at-risk disease-free population and then multiplying by 100,000. IRRs were calculated to compare the incidence rate in the post-COVID-19 period with that in the corresponding quarter of 2019.
To assess the changes related to hospitalization during the COVID-19 period, we analyzed the annual number of admission and LOS. In this context, the term admission encompasses hospitalizations for all medical conditions, and the number of admissions per patients was calculated by dividing the total annual number of admissions by the number of individuals admitted. LOS was calculated by dividing the total number of days a person spent in the hospital over the year by the annual number of individuals admitted to that specific type of hospital. If an individual was admitted to both a nursing and a general hospital, we calculated the number of admissions and LOS separately for each type of hospital.
Summary statistics were used to delineate the characteristics of patients with newly diagnosed ESKD. ANOVA was used to assess year-to-year changes in continuous variables, and the chi-square test was used for categorical variables. The same statistical analysis approach was applied to both categorical and continuous variables for LOS and number of admissions. Poisson regression models were used to calculate the incidence rate and its corresponding 95% confidence interval (CI), whereas autoregression was conducted to test for significant secular trends in the incidence rate for each KRT modality and age group.
We used ITS linear regression to investigate impact of COVID-19 pandemic on KRT incidence. ITS analysis is a quasi-experimental research methodology, allowing for the assessment of immediate and long-term effect following specific interventions [11]. On ITS, the dependent variable, incidence, was calculated as monthly incidence per 100,000 population. ITS analyses were conducted for different subgroups, considering KRT modality and age groups. Observations were collected from January 2018 to April 2022, comprising 52 monthly incidence data points. Both immediate level changes and trend changes in monthly incidence were observed before and after the intervention. In our analysis, March 1, 2020, was considered as the starting point of the COVID-19 pandemic, which is the intervention. Although the coronavirus initially outbreaks domestically in January 2020, the national crisis alert was raised on February 23, 2020. Considering the lag period, our analysis adjusted for the impact of the Covid-19 pandemic starting from March, 2020. The segmented regression equation for ITS analysis is as follows:
Here, yt represents the monthly incidence. T is the number of months since the beginning of observation, Xt is a categorical variable with 0 before the intervention and 1 after the intervention. TXt is an interaction term indicating the number of months after the intervention. ╬▓0 is the mean monthly incidence during the pre-pandemic period (the regression intercept). ╬▓1 represents the monthly trend change in incidence before the pandemic, and ╬▓2 is the level change in incidence immediately after the COVID-19 outbreak. ╬▓3 denotes the change in monthly incidence trend after the COVID-19 outbreak, and ╬▓1 + ╬▓3 represents the overall time trend after the COVID-19 pandemic. Z is a vector of dummy variables representing the month of the year.
All statistical analyses were performed using SAS 9.4 software (SAS Institute, Inc., Cary, NC, USA), and p values less than 0.05 were considered statistically significant.
From 2018 to April 2022, the annual incident cases of ESKD in South Korea remained stable, ranging from 15,338 to 15,833 per year, with no significant differences in the absolute numbers before or after the pandemic. However, there were significant shift in the distribution of KRT modalities among the patients with incident ESKD. The percentage of patients with PD decreased from 5.7% in 2018 to 1.3% by 2022. The proportion of HD patients undergoing HD increased from 81.6% to 85.0%, but the number of patients using catheters at the initiation of HD decreased from 63.6% to 55.4%. The proportion of KT recipients remained relatively stable, ranging from 12.7% to 17.3%. However, the preemptive KT percentage decreased from 50.8% to 44.6% (Table 1).
When examining the characteristics of incident ESKD patients, age, sex, insurance type, or other factors not significantly changed before and after the pandemic. The average age ranged from 63.3 to 64.7 years over the five-year study period, with a male predominance of over 60%. An important observation we made involved the remarkably high proportion of medical aid beneficiaries, ranging from 11.9% to 13.2%. In South Korea, medical aid beneficiaries constitute only 3% of the population [12], making this ratio notably high among patients with ESKD. Approximately 70% of the patients had diabetes, and one in three patients had conditions such as congestive heart failure or peptic ulcers. When assessing comorbid conditions within the year preceding the ESKD diagnosis, the Charlson Comorbidity Index (CCI) score [13] ranged between 5.4 and 5.8 points (Table 1).
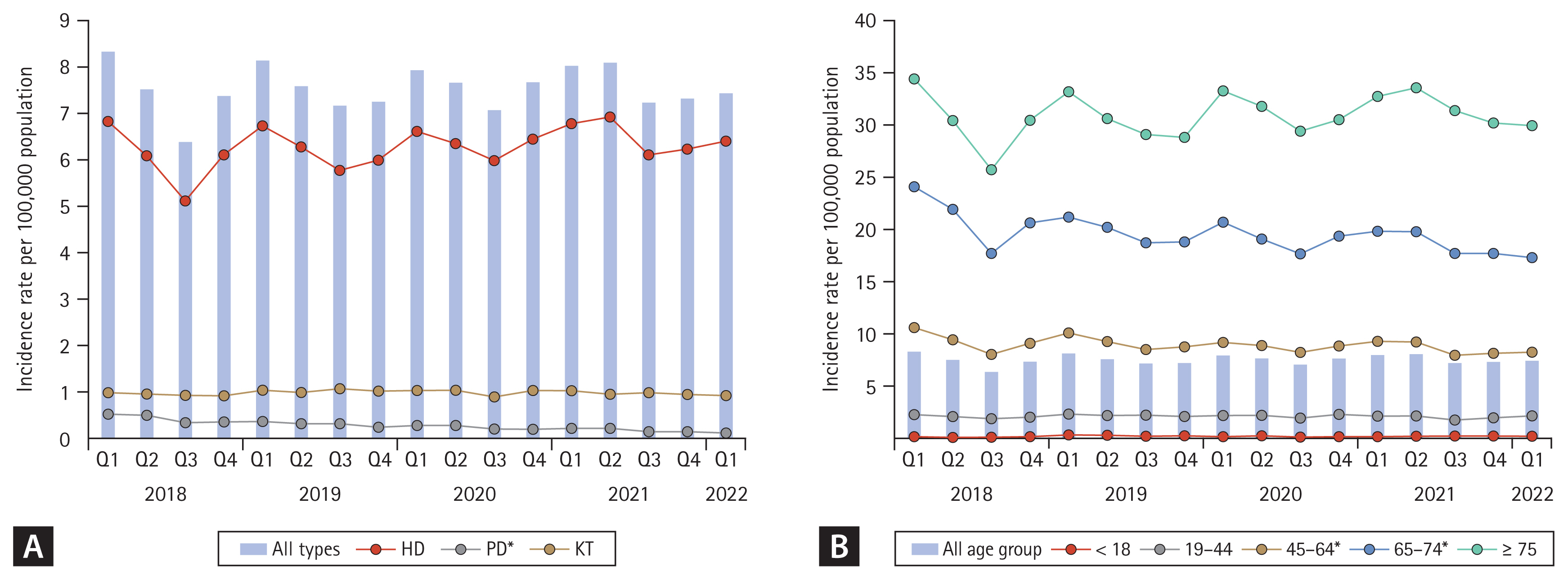
From the first quarter of 2018 to the first quarter of 2022, the incidence rate of ESKD ranged between 6.38 and 8.33 per 100,000. Annual trends showed higher incidence rates in the first and second quarters than in the third and fourth quarters; however, no secular trends were observed. Regarding KRT modality, HD had the highest quarterly incidence rate, followed by KT and PD. HD showed quarterly incidence rates ranging from 5.12 to 6.93, while KT ranged from 0.88 to 1.06. PD had quarterly incidence rates ranging from 0.11 to 0.52, with a noticeable decreasing secular trend from 2018 to 2022 (Fig. 1A).
When examining the age-standardized quarterly incidence rate by age group, the older age groups exhibited higher incidence rates. The overall age-standardized quarterly incidence rate for the entire population was 7.53 per 100,000 persons. Among those aged 45 and older, a notably higher quarterly incidence rate was observed. The age-standardized quarterly incidence rates for the age groups of 45ŌĆō64, 65ŌĆō74, and 75 and older were 8.95, 19.57, and 30.92 per 100,000 persons, respectively. Significantly decreasing secular trends were observed in the 45ŌĆō64 and 65ŌĆō74 age groups. The age-standardized quarterly incidence rates for the age groups under 18 and 19ŌĆō44 were 0.21 and 2.12 per 100,000 persons, respectively (Fig. 1B).
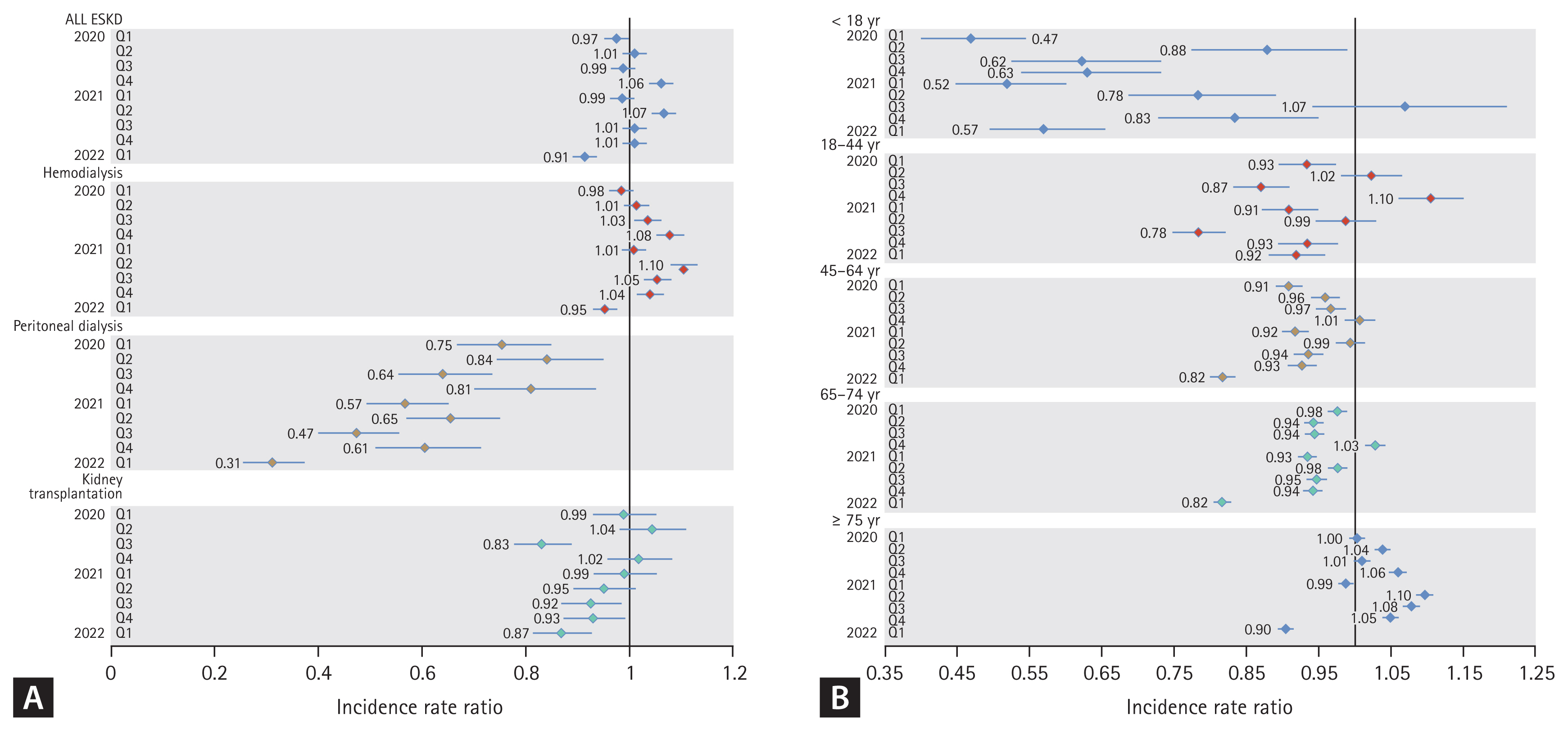
A comparison of the pre- and post-pandemic periods showed that the overall ESKD incidence did not exhibit a noticeable increase or decrease in the IRR. There were no observable quarterly trends and the overall incidence of ESKD remained unchanged. When examined by the KRT modality, PD consistently had an IRR of 1 or less in all quarters compared to 2019, whereas HD mostly had an IRR greater than 1. The incidence of KT had values of one or more in the second and fourth quarters of 2020; however, it showed a decreasing trend over time (Fig. 2A).
In terms of age-specific IRR, most age groups, excluding the 75 years and older age group, showed an IRR of 1 or less in most quarters. The 45ŌĆō74 age groups consistently exhibited values of 1 or less, except for the fourth quarter of 2020. Similarly, the 18ŌĆō44 age group had IRR values of 1 or less, except for the second and fourth quarters of 2020. The age group under 18 years, owing to its low incidence rate, showed wide CIs, but aside from the fourth quarter of 2021, it consistently exhibited IRR values of 1 or less. In contrast, the age group of 75 years or older that had the highest age-standardized incidence rate compared to other age groups, showed values of 1 or more in most quarters, excluding the first quarter of 2021 and the first quarter of 2022 (Fig. 2B).
Overall, ITS analysis provided confirmed that the COVID-19 outbreak had not statistically significant immediate or long-term effects on the overall incidence of KRT. Specifically, there were no significant month-to-month changes in the incidence of all KRT before (baseline trend: ŌłÆ0.001; p = 0.81) and after the outbreak (trend change: ŌłÆ0.001; p = 0.77). Notably, only the incidence of PD showed a significant trend change. It exhibited a decreasing trend pre-COVID (baseline trend: ŌłÆ0.004; p < 0.001), which lessened post-outbreak (trend change: 0.001; p = 0.04). The incidence of KT showed a significant decreasing trend after the COVID outbreak (trend change: 0.001; p = 0.02), while HD incidences remained stable throughout (Table 2).
When analyzed by age groups, the 45ŌĆō64 group showed a significant decrease in incidence pre-COVID (baseline trend: ŌłÆ0.001; p = 0.04), with a more pronounced decrease in the 65ŌĆō74 group (baseline trend: ŌłÆ0.042; p = 0.01). For those aged 18 and below, there was a significant increase pre-pandemic (baseline trend: 0.002; p = 0.03). Other age groups did not exhibit significant trend changes, and no age group showed significant month-to-month changes post-COVID. Furthermore, there were no immediate level change effects observed in any KRT modality or age group following the COVID outbreak (Table 2).
We examined the annual number of admission and the LOS in patients with ESKD from 2018 to 2021. Although there were no significant differences in the incidence rates of ESKD, there were significant changes in the number of admissions and LOS over time. The annual number of hospitalizations in 2018 and 2019 was 2.67 and 2.65, respectively. In contrast, it decreased slightly to 2.50 in 2020 and 2.52 in 2021. This trend was also observed in general hospitals, where the number of hospitalizations decreased from 2.84 in both 2018 and 2019 to 2.68 in both 2020 and 2021. Nursing hospitals, on the other hand, showed a lower number of admissions compared to general hospitals, but with longer hospital stays. The number of admissions to nursing hospitals decreased from 1.77 in 2018 to 1.60 in 2020, but increased to 1.76 in 2021. The LOS decreased continuously for all patients with ESKD from 2018 to 2021. In nursing hospitals, LOS decreased from 165.01 days in 2018 to 147.77 days in 2021, while in general hospitals, it decreased significantly from 61.34 days in 2018 to 55.58 days in 2021 (Table 3).
In HD patients, there was a significant reduction in the number of admissions and LOS after the COVID-19 pandemic, similar to the trends observed in the overall incidence of ESKD. As patients undergoing HD constitute the majority of the overall ESKD incidence, the parameters such as the number of admissions and LOS in HD cases were similar to those for the overall ESKD cases. Patients undergoing HD had a slightly higher number of admissions, approximately 0.05 admissions more than the overall ESKD cases, and their LOS was approximately 5 days longer. In both nursing and general hospitals, the LOS of patients undergoing HD decreased over time, and the number of admissions showed a similar pattern of increase and decrease, as was observed for ESKD cases overall (Table 3).
In contrast, patients undergoing PD did not show significant trends in annual number of admissions and LOS, and there were no significant differences. Compared to overall patients with ESKD, there was no difference in the number of admissions for PD cases, but the LOS was nearly half as long. While no distinct trends were observed for any hospital type during the COVID-19 period, nursing hospitals showed a sudden increase in both the number of admissions and LOS in 2021. KT recipients had the lowest annual number of admissions and LOS among all modality types, and no significant differences were observed across the years (Table 3).
This study aimed to investigate the incidence of ESKD, modalities of KRT, and changes in healthcare access for ESKD patients in South Korea during COVID-19 pandemic.
Initially, our findings revealed that the absolute number of annual incident cases of ESKD in South Korea remained stable from 2018 to April 2022, ranging between 15,338/ year to 15,833/year. Even when divided by quarters from 2018 onwards, there was no statistically significant change in the incidence of ESKD. The ITS analysis confirmed that the pandemic had no immediate or long-term impact on the overall KRT incidence. This stability in ESKD incidence may reflect the resilience of the healthcare system in continuing to diagnose and manage ESKD cases despite the challenges posed by the pandemic.
Potential factors that could influence the incidence of ESKD include acute kidney injury (AKI), which frequently occurs in individuals diagnosed with COVID-19, especially among those who are hospitalized, leading to a heightened incidence of AKI overall. Studies have shown an increased risk of developing CKD in COVID-19 patients, with many AKI survivors progressing to CKD within 90 days, and some potentially advancing to ESKD [14]. The occurrence of COVID-19-associated AKI or AKI on CKD during the pandemic might have impacted the incidence of ESKD. A notable decline in incident ESKD cases was observed in the United States early in the pandemic, attributed to increased mortality in patients with advanced CKD and compromised access to KRT preparations [15]. Similarly, the possibility remains that the incidence of ESKD in Korea might have been affected by COVID-19-related premature death in CKD patients.
Contrary to the stability of the ESKD incidence rate, there were notable changes in the distribution of KRT modalities among patients with incident ESKD during this period. Specifically, the percentage of patients undergoing PD decreased from 5.7% in 2018 to 1.3% by 2022. In contrast, the proportion of patients receiving HD increased from 81.6% to 85.0%. This change in the distribution of KRT modalities is speculated to be a continuation of the change in treatment trends for patients with ESKD in Korea, as reported in several previous studies [16], rather than a direct consequence of the COVID-19 pandemic. As seen in the ITS analysis, previously on a decreasing trajectory, the PD incidence rate continued to decline, but have slowed. In addition, the proportion of patients in whom HD was initiated with catheters decreased from 63.6% to 55.4%. This observation indicated that a greater number of patients started HD through established vascular access rather than through emergent catheter insertion, implying that high-quality medical care was provided even during the coronavirus pandemic.
The proportion of KT recipients remained relatively stable, ranging from 12.7% to 17.3%. However, the preemptive KT rate decreased from 50.8% to 44.6%. This decline is hypothesized to be due to the timing of transplant surgery that may have been affected by difficulties and disruptions in healthcare during the pandemic. Additionally, KT may have been performed with caution because a high dose of immunosuppressant is required in the early stages of transplantation. When considering the long-term benefits of KT over chronic dialysis [17], this highlights the need for a robust and adaptable transplant infrastructure that can navigate the complexities of infectious disease outbreaks while continuing to provide transplant procedures safely.
During the COVID-19 pandemic, significant changes in healthcare access and patient behavior were reflected in the variations in CCI scores observed among ESKD patients from 2018 to 2022. The comorbidity score of ESKD patients gradually decreased from 5.8 to 5.4. Among the 15 conditions examined, myocardial infarction, congestive heart failure, DM, DM complications, and paraplegia all decreased slightly during pandemic and chronic pulmonary disease had the greatest impact on the CCI score, decreasing sharply from 45.2% in 2018 to 31.0% in 2022. The decrease may be partly attributed to the reduced frequency of routine healthcare visits during the pandemic, impacting the management and diagnosis rates of conditions such as DM complications and congestive heart failure. Furthermore, specific public health measures, such as lockdowns reducing physical activity, alongside changes in patient behaviorŌĆōincluding increased use of masks and social distancingŌĆōlikely contributed to the observed decrease in chronic pulmonary disease prevalence [18].
This study investigated the ESKD incidence rates by KRT modality and age. ITS analysis revealed that no immediate change was observed in any KRT modality or age group following the COVID outbreak. Age-specific analysis revealed that higher age groups had higher incidence rates of ESKD, with the elderly population, particularly those aged 75 and older, experiencing notably higher rates. This finding is consistent with the well-established association between aging and the risk of ESKD [19]. The incidence of ESKD in children under 18 decreased before COVID-19, but no significant trend was observed after COVID-19. Chronic kidney disease in children under 18 is mainly associated with congenital factors such as congenital kidney malformations and congenital urinary tract disorders [20]. During the COVID-19 era, it is plausible that factors such as psychological stress could have exerted a negative effect on fetal health, thereby potentially contributing to the absence of a decline in ESKD incidence among children under 18. Additionally, due to the significantly lower incidence of ESKD in children compared to other age groups, itŌĆÖs impossible to entirely rule out the possibility of error. Contrary to those under 18, older adults aged 65 and older exhibited a tendency of increasing ESKD incidence before the onset of COVID-19. They are more vulnerable to ESKD due to age-related weakening of kidney health, making those with pre-existing conditions such as hypertension and diabetes more susceptible to ESKD [9]. However, there was a tendency for the incidence of ESKD to decrease among the 45ŌĆō64 age group and the 65ŌĆō74 age group. The lack of such trends during the COVID-19 era may be attributed to the development of new treatments delaying the progression to ESKD (such as SGLT-2 inhibitors, GLP-1 agonist, RAAS blockers, etc) or changes in healthcare utilization patterns during the pandemic [21]. It is also possible that there was an underestimation of ESKD due to deaths occurring before reaching KRT. As previous data [22], during the COVID-19 pandemic, there were more excess deaths observed in the age groups of ŌĆś50ŌĆō64ŌĆÖ and ŌĆś65ŌĆō79ŌĆÖ compared to those aged ŌĆś80 and olderŌĆÖ when compared to the previous years.
We investigated whether the COVID-19 pandemic caused difficulties in hospitalization or led to situations where the necessary medical care was not provided. There were no significant changes in hospitalization-related medical care for PD or KT recipients before and after COVID-19. Only patients undergoing HD showed a tendency for reduced hospitalization and LOS, reflecting potential changes in patient care patterns during the pandemic. While a decrease in hospitalization may, in some instances, be seen as a positive outcome indicative of outpatient management or improved disease management, but their potential impact needs to be examined more carefully. During the COVID-19 pandemic, there was a widespread culture of reluctance to visit and admit hospitals due to concerns about infection, and the provision of medical services was very different from the time when there were no infectious diseases. Despite the fact many patients receiving HD are admitted to nursing hospitals under special circumstance, there continues to be a decrease in both LOS and the number of admissions.
Although informative, this study had some limitations. First, there may have been minor errors in the number of people infected with COVID-19. Patients who could not be traced in claims data owing to data privacy concerns were excluded from the study. Cases that could not be traced in the claims data were as follows. First, if hospitals had treated fewer than three COVID-19 patients during the entire study period, these patients were excluded. Second, patients infected with COVID-19 between January and March 2020 were excluded from the study. However, it is important to note that during January to March 2020, the early stages of the COVID-19 outbreak, the number of COVID-19 cases was extremely low. Although there may have been variations in patient numbers, the patients included in this study adequately represented the overall population of patients who underwent KRT. Second, it was not possible to distinguish between living and deceased donor KT based on claims data alone. However, all preemptive KT cases were probably living donor cases, and there appeared to be no significant change in either total or preemptive KT before and after the COVID pandemic. Third, we could only access the claims data until June 2022. This limited timeframe may have affected the comprehensiveness of our findings. This constrained timeframe restricted our analysis to a specific period, potentially limiting the depth and breadth of insights obtained from a more extended dataset. Future research extending beyond this period is crucial to capture the evolving dynamics and potential long-term consequences of the observed shifts in ESKD and KRT patterns.
This study provides valuable insights into the dynamics of ESKD and KRT during the COVID-19 pandemic in South Korea. These findings highlight the stability of ESKD incidence while revealing shifts in the choice of KRT modalities, with a notable increase in HD utilization. While there have been individualistic differences as COVID-19 has impacted everyone, this study showed that the overall healthcare system remained stable during the pandemic, with no major disruptions to care for patients with ESKD in South Korea. As we navigate the complexities of future infectious disease outbreaks, these insights serve as a foundation for informed strategies to safeguard the well-being of patients with ESKD.
1. Despite the COVID-19 pandemic, there was no significant increase in the overall incidence of ESKD in South Korea.
2. While ESKD incidence remained stable, there were notable changes in the distribution of KRT modalities, with a decrease in PD utilization and an increase in HD usage, suggesting ongoing treatment trends rather than direct consequences of the pandemic.
3. Patients undergoing HD showed a tendency for reduced hospitalization and LOS, potentially reflecting changes in patient care patterns during the pandemic, highlighting the need for further examination of these trends and their ramifications on patient outcomes.
Notes
CRedit authorship contributions
Ah-Young Kim: conceptualization, methodology, data curation, formal analysis, validation, writing - original draft, visualization; Min-Jeong Lee: conceptualization, investigation, writing - original draft, visualization; Heejung Choi: writing - review & editing, visualization; Hankil Lee: methodology, resources, writing - review & editing, supervision, project administration, funding acquisition; Inwhee Park: writing - review & editing, supervision, project administration
Figure┬Ā1
ESKD incident rate by KRT modality and age. (A) Incidence rate of ESKD per 100,000 population by KRT modality. (B) Age-standardized incidence rate per 100,000 population. ESKD, end-stage kidney disease; KRT, kidney replacement therapy; HD, hemodialysis; PD, peritoneal dialysis; KT, kidney transplantation. *Statistically significant trends.
Figure┬Ā2
Incident rate ratios by KRT modalities and age group. (A) Incidence rate ratios for ESKD and its KRT modalities compared to the corresponding quarter in 2019. (B) Incidence rate ratios by age group for ESKD compared to the corresponding quarter in 2019. KRT, kidney replacement therapy; ESKD, end-stage kidney disease.
Table┬Ā1
Characteristics of adult patients with newly diagnosed ESKD
| Variable | 2018 | 2019 | 2020 | 2021 | 2022a) | p value |
|---|---|---|---|---|---|---|
| Incident case | 15,338 | 15,610 | 15,718 | 15,833 | 5,494 | |
| Age (yr) | 63.3 ┬▒ 14.4 | 63.3 ┬▒ 15.1 | 64.0 ┬▒ 14.9 | 64.7 ┬▒ 14.8 | 63.8 ┬▒ 15.1 | < 0.001 |
| Sex | 0.3039 | |||||
| ŌĆāMale | 9,273 (60.5) | 9,462 (60.6) | 9,595 (61.0) | 9,686 (61.2) | 3,402 (61.9) | |
| ŌĆāFemale | 6,065 (39.5) | 6,148 (39.4) | 6,123 (39.0) | 6,147 (38.8) | 2,092 (38.1) | |
| Insurance | 0.0171 | |||||
| ŌĆāNHI | 13,256 (86.4) | 13,473 (86.3) | 13,561 (86.3) | 13,688 (86.5) | 4,823 (87.8) | |
| ŌĆāMA | 2,013 (13.1) | 2,035 (13.0) | 2,076 (13.2) | 2,059 (13.0) | 654 (11.9) | |
| ŌĆāVA | 69 (0.4) | 102 (0.7) | 81 (0.5) | 86 (0.5) | 17 (0.3) | |
| DM | 10,803 (70.4) | 11,165 (71.5) | 11,385 (72.4) | 11,401 (72.0) | 3,799 (69.1) | |
| Types of KRT | < 0.001 | |||||
| ŌĆāHD | 12,509 (81.6) | 12,845 (82.3) | 13,174 (83.8) | 13,454 (85.0) | 4,473 (81.4) | |
| ŌĆāCatheter utilization at initiation of HD | 7,961 (63.6) | 8,038 (62.6) | 8,066 (61.2) | 7,886 (58.6) | 2,477 (55.4) | |
| ŌĆāPeritoneal dialysis | 881 (5.7) | 633 (4.1) | 480 (3.1) | 362 (2.3) | 71 (1.3) | |
| ŌĆāKT | 1,948 (12.7) | 2,132 (13.7) | 2,064 (13.1) | 2,017 (12.7) | 950 (17.3) | |
| ŌĆāPreemptive KT | 990 (50.8) | 1,010 (47.4) | 970 (47.0) | 963 (47.7) | 424 (44.6) | |
| CCI score | 5.8 ┬▒ 2.3 | 5.6 ┬▒ 2.3 | 5.6 ┬▒ 2.3 | 5.5 ┬▒ 2.3 | 5.4 ┬▒ 2.3 | < 0.001 |
| ŌĆāMyocardial infarction | 1,159 (7.6) | 1,120 (7.2) | 1,109 (7.1) | 1,036 (6.5) | 340 (6.2) | < 0.001 |
| ŌĆāCongestive heart failure | 5,162 (33.7) | 4,837 (31.0) | 5,022 (32.0) | 5,141 (32.5) | 1,733 (31.5) | < 0.001 |
| ŌĆāPeripheral vascular disease | 3,132 (20.4) | 3,237 (20.7) | 3,397 (21.6) | 3,567 (22.5) | 1,279 (23.3) | < 0.001 |
| ŌĆāCerebrovascular disease | 3,819 (24.9) | 3,828 (24.5) | 3,951 (25.1) | 3,900 (24.6) | 1,182 (21.5) | < 0.001 |
| ŌĆāChronic pulmonary disease | 6,940 (45.2) | 6,575 (42.1) | 6,189 (39.4) | 5,084 (32.1) | 1,704 (31.0) | < 0.001 |
| ŌĆāRheumatic disease | 680 (4.4) | 654 (4.2) | 695 (4.4) | 705 (4.5) | 220 (4.0) | 0.494 |
| ŌĆāPeptic ulcer | 5,151 (33.6) | 4,789 (30.7) | 4,772 (30.4) | 4,506 (28.5) | 1,581 (28.8) | < 0.001 |
| ŌĆāLiver disease | 1,404 (9.2) | 1,411 (9.0) | 1,462 (9.3) | 1,570 (9.9) | 476 (8.7) | 0.022 |
| ŌĆāDiabetes mellitus | 9,588 (62.5) | 9,467 (60.6) | 9,271 (59.0) | 9,220 (58.2) | 3,148 (57.3) | < 0.001 |
| ŌĆāDM complication | 8,056 (52.5) | 7,723 (49.5) | 7,843 (49.9) | 7,769 (49.1) | 2,643 (48.1) | < 0.001 |
| ŌĆāParaplegia | 562 (3.7) | 445 (2.9) | 467 (3.0) | 423 (2.7) | 104 (1.9) | < 0.001 |
| ŌĆāKidney disease | 14,971 (97.6) | 15,051 (96.4) | 15,204 (96.7) | 15,345 (96.9) | 5,372 (97.8) | < 0.001 |
| ŌĆāCancer | 1,832 (11.9) | 1,964 (12.6) | 1,988 (12.6) | 2,169 (13.7) | 623 (11.3) | < 0.001 |
| ŌĆāMetastatic tumor | 229 (1.5) | 193 (1.2) | 201 (1.3) | 218 (1.4) | 69 (1.3) | 0.2987 |
| ŌĆāSevere liver disease | 325 (2.1) | 317 (2.0) | 284 (1.8) | 297 (1.9) | 94 (1.7) | 0.1594 |
Table┬Ā2
Changes in trends and levels before and after the COVID-19 pandemic: an interrupted time series results
| Group | Mean incidence (intercept) | Change in trend before COVID-19 pandemic (95% CI) | Change in level after COVID-19 outbreak (95% CI) | Change in trend after COVID-19 outbreak (95% CI) |
|---|---|---|---|---|
| All KRT | 2.50 | ŌłÆ0.001 (ŌłÆ0.004 to 0.003) | 0.083 (0.008 to 0.157) | ŌłÆ0.001 (ŌłÆ0.006 to 0.003) |
| Types of KRT | ||||
| ŌĆāHD | 2.03 | 0.001 (ŌłÆ0.002 to 0.004) | 0.061 (ŌłÆ0.010 to 0.132) | 0.001 (ŌłÆ0.003 to 0.005) |
| ŌĆāPD | 0.17 | ŌłÆ0.004a) (ŌłÆ0.004 to ŌłÆ0.003) | 0.020 (0.010 to 0.030) | 0.001a) (0.001 to 0.002) |
| ŌĆāKT | 0.31 | 0.001 (0.000 to 0.002) | 0.007 (ŌłÆ0.013 to 0.028) | ŌłÆ0.003a) (ŌłÆ0.005 to ŌłÆ0.002) |
| Age group (yr) | ||||
| ŌĆā< 18 | 0.05 | 0.002a) (0.001 to 0.002) | ŌłÆ0.020 (ŌłÆ0.036 to ŌłÆ0.004) | ŌłÆ0.002 (ŌłÆ0.003 to ŌłÆ0.001) |
| ŌĆā18ŌĆō44 | 0.70 | 0.001 (ŌłÆ0.001 to 0.003) | 0.004 (ŌłÆ0.040 to 0.048) | ŌłÆ0.004 (ŌłÆ0.006 to ŌłÆ0.001) |
| ŌĆā45ŌĆō64 | 3.19 | ŌłÆ0.001a) (ŌłÆ0.014 to ŌłÆ0.005) | 0.063 (ŌłÆ0.039 to 0.165) | 0.000 (ŌłÆ0.006 to 0.006) |
| ŌĆā65ŌĆō74 | 7.35 | ŌłÆ0.042a) (ŌłÆ0.057 to ŌłÆ0.027) | 0.265 (ŌłÆ0.057 to 0.058) | 0.017 (ŌłÆ0.004 to 0.039) |
| ŌĆāŌēź 75 | 10.28 | ŌłÆ0.012 (ŌłÆ0.028 to 0.004) | 0.606 (0.252 to 0.959) | 0.005 (ŌłÆ0.015 to 0.026) |
Table┬Ā3
Changes in annual number of admissions and LOS among incident ESKD patients during the COVID-19 pandemic
| Type of hospital | Overall | Hemodialysis | Peritoneal dialysis | Kidney transplantation | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||||||
| 2018 | 2019 | 2020 | 2021e) | 2018 | 2019 | 2020 | 2021e) | 2018 | 2019 | 2020 | 2021e) | 2018 | 2019 | 2020 | 2021e) | ||
| All types | N | 15,338 | 15,610 | 15,718 | 9,019 | 12,509 | 12,845 | 13,174 | 7,884 | 772 | 575 | 421 | 204 | 1,860 | 2,070 | 1,967 | 975 |
|
|
|||||||||||||||||
| Admissiona,b,c) | 2.67 (2.07) | 2.65 (2.11) | 2.50 (1.98) | 2.52 (2.00) | 2.74 (2.12) | 2.70 (2.15) | 2.54 (2.02) | 2.56 (2.04) | 2.43 (1.70) | 2.69 (1.86) | 2.48 (1.75) | 2.67 (1.73) | 2.25 (1.74) | 2.28 (1.89) | 2.24 (1.66) | 2.10 (1.62) | |
|
|
|||||||||||||||||
| LOSa,b) | 61.34 (83.24) | 60.11 (82.55) | 57.53 (80.67) | 55.58 (78.16) | 66.67 (88.23) | 64.93 (87.59) | 61.66 (85.19) | 59.38 (82.31) | 34.78 (50.16) | 35.75 (45.33) | 33.34 (47.63) | 36.52 (52.81) | 32.04 (30.50) | 33.27 (33.42) | 32.15 (31.17) | 28.95 (23.46) | |
|
|
|||||||||||||||||
| Nursing hospital | N | 2,717 | 2,831 | 2,768 | 1,531 | 2,665 | 2,776 | 2,727 | 1,510 | 40 | 35 | 24 | 16 | 12 | 20 | 17 | 9 |
|
|
|||||||||||||||||
| Admissiona,b) | 1.77 (1.13) | 1.69 (1.11) | 1.60 (1.01) | 1.76 (1.19) | 1.77 (1.13) | 1.69 (1.10) | 1.60 (1.01) | 1.72 (1.18) | 2.08 (1.61) | 1.83 (0.98) | 1.42 (0.72) | 1.94 (1.65) | 1.25 (0.62) | 1.25 (0.55) | 1.71 (1.57) | 2.11 (1.36) | |
|
|
|||||||||||||||||
| LOSa,b) | 165.01 (125.8) | 160.28 (127.0) | 154.95 (126.9) | 147.77 (122.4) | 165.98 (125.8) | 161.88 (94.4) | 156.15 (127.0) | 148.69 (122.4) | 132.55 (114.3) | 94.37 (108.3) | 91.46 (105.4) | 121.25 (128.5) | 58.58 (62.3) | 53.55 (52.5) | 52.00 (78.7) | 41.00 (28.2) | |
|
|
|||||||||||||||||
| General hospital | N | 13,986 | 14,260 | 14,182 | 7,488 | 11,406 | 11,670 | 11,835 | 6,334 | 732 | 540 | 397 | 188 | 1,848 | 2,050 | 1,950 | 966 |
|
|
|||||||||||||||||
| Admissiona,b,c,d) | 2.84 (2.16) | 2.84 (2.21) | 2.68 (2.07) | 2.68 (2.09) | 2.97 (2.23) | 2.94 (2.26) | 2.75 (2.14) | 2.76 (2.15) | 2.45 (1.70) | 2.74 (1.89) | 2.54 (1.77) | 2.73 (1.73) | 2.26 (1.74) | 2.29 (1.89) | 2.24 (1.66) | 2.10 (1.62) | |
|
|
|||||||||||||||||
| LOSa,b,d) | 41.20 (52.03) | 40.22 (50.80) | 38.52 (49.21) | 36.68 (46.80) | 43.46 (55.27) | 41.86 (53.76) | 39.89 (51.83) | 38.09 (49.62) | 29.44 (37.48) | 31.96 (34.79) | 29.83 (39.30) | 29.31 (32.20) | 31.87 (30.14) | 33.07 (33.14) | 31.97 (30.42) | 28.83 (23.40) | |
REFERENCES
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019 N Engl J Med 2020;382:727ŌĆō733.
2. ERA-EDTA Council; ERACODA Working Group. Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA. Nephrol Dial Transplant 2021;36:87ŌĆō94.




3. De Meester J, De Bacquer D, Naesens M, et al. Incidence, characteristics, and outcome of COVID-19 in adults on kidney replacement therapy: a regionwide registry study. J Am Soc Nephrol 2021;32:385ŌĆō396.



4. Changsirikulchai S, Sangthawan P, Janma J, Rajborirug S, Ingviya T. COVID-19 incidence and outcomes among patients with kidney replacement therapy. Kidney Res Clin Pract 2023;42:649ŌĆō659.




5. Park HC, Lee YK, Ko E, et al. COVID-19-related clinical outcomes among Korean hemodialysis patients. Kidney Res Clin Pract 2022;41:591ŌĆō600.




6. Chothia MY, Barday Z, Nel J, Davids MR. Impact of COVID-19 on access to chronic kidney replacement therapy in the public sector of Western Cape Province, South Africa. S Afr Med J 2021;111:13442.


7. Kyoung DS, Kim HS. Understanding and utilizing claim data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) database for research. J Lipid Atheroscler 2022;11:103ŌĆō110.




8. Korean Statistical Information Service. Population Projections for Korea: population trends and projections of the world and Korea [Internet] Daejeon: Statistics Korea, 2023. [cited 2024 Mar 31]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040A3.
9. Lee MJ, Ha KH, Kim DJ, Park I. Trends in the incidence, prevalence, and mortality of end-stage kidney disease in South Korea. Diabetes Metab J 2020;44:933ŌĆō937.




10. Obi Y, Kalantar-Zadeh K, Streja E, et al. Seasonal variations in transition, mortality and kidney transplantation among patients with end-stage renal disease in the USA. Nephrol Dial Transplant 2017;32(suppl_2):ii99ŌĆōii105.



11. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299ŌĆō309.


12. National Health Insurance Service, Health Insurance Review & Assessment Service. 2021 medical aid statistics. Wonju: Health Insurance Review & Assessment Service, 2022.
13. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130ŌĆō1139.


14. Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 2020;98:209ŌĆō218.


15. Weinhandl ED, Gilbertson DT, Wetmore JB, Johansen KL. COVID-19-associated decline in the size of the end-stage kidney disease population in the United States. Kidney Int Rep 2021;6:2698ŌĆō2701.



16. Hong YA, Ban TH, Kang CY, et al. Trends in epidemiologic characteristics of end-stage renal disease from 2019 Korean Renal Data System (KORDS). Kidney Res Clin Pract 2021;40:52ŌĆō61.




17. Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 2011;11:2093ŌĆō2109.


18. Huang QS, Wood T, Jelley L, et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat Commun 2021;12:1001.


19. Toyama T, Kitagawa K, Oshima M, et al. Age differences in the relationships between risk factors and loss of kidney function: a general population cohort study. BMC Nephrol 2020;21:477.




20. Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol 2012;27:363ŌĆō373.



21. McCullough KP, Morgenstern H, Saran R, Herman WH, Robinson BM. Projecting ESRD incidence and prevalence in the United States through 2030. J Am Soc Nephrol 2019;30:127ŌĆō135.



22. Lee PH, Kim MS. In-depth analysis of changes in mortality since the outbreak of COVID-19 [Internet] Wonju: Health Insurance Review & Assessment Service, 2023. [cited 2024 Mar 31]. Available from: https://repository.hira.or.kr/handle/2019.oak/3090.
-
METRICS

- Related articles
-
Incidence of rheumatic diseases during the COVID-19 pandemic in South Korea2023 March;38(2)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


