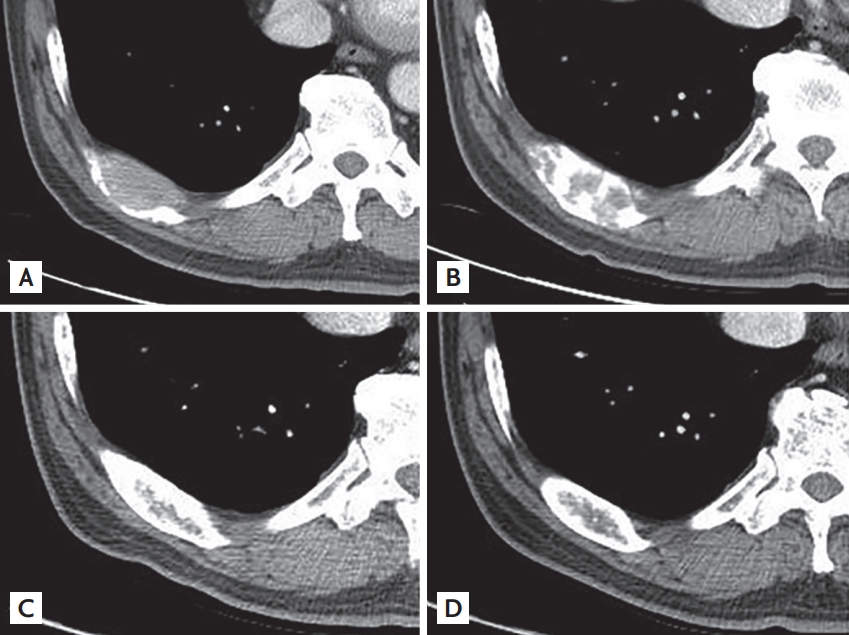
A 64-year-old man visited our hospital because of chest pain. He had undergone a left nephroureteretomy due to sarcomatoid-variant urothelial carcinoma 1 year ago. Computed tomography (CT) showed osteolytic bone lesions on the ribs (Fig. 1A) and spine, suggesting bone metastases. He was administered pembrolizumab, a checkpoint inhibitor, as he was unfit to undergo platinum therapy. After 12 weeks from the start of the treatment, CT revealed an osteoblastic change of the metastatic bone lesions (Fig. 1B), and a later image showed consistent bone remodeling reaction. After 1 year, the lesions changed in morphology to more closely resemble normal cortical bone (Fig. 1C); and after 2 years (Fig. 1D), the lesions completely changed to resemble normal cortical bone. Whole-body bone scan showed nearly normal uptake at the metastatic bone lesions. Currently, it remains uncertain whether the osteoblastic reaction responds to immune checkpoint inhibitors that target malignant bone lesions. This case suggests that immune checkpoint inhibitors are effective against bone lesions by converting metastatic bone lesions from osteolytic lesions to osteoblastic lesions.
Informed consent was obtained from the patient



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





