1. Knuuti J, Wijns W, Saraste A, et al.; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407ŌĆō477.

4. El-Menyar A, Zubaid M, Sulaiman K, et al.; Gulf Registry of Acute Coronary Events (Gulf RACE) Investigators. Atypical presentation of acute coronary syndrome: a significant independent predictor of in-hospital mortality. J Cardiol 2011;57:165ŌĆō171.


5. Sheifer SE, Rathore SS, Gersh BJ, et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation 2000;102:1651ŌĆō1656.


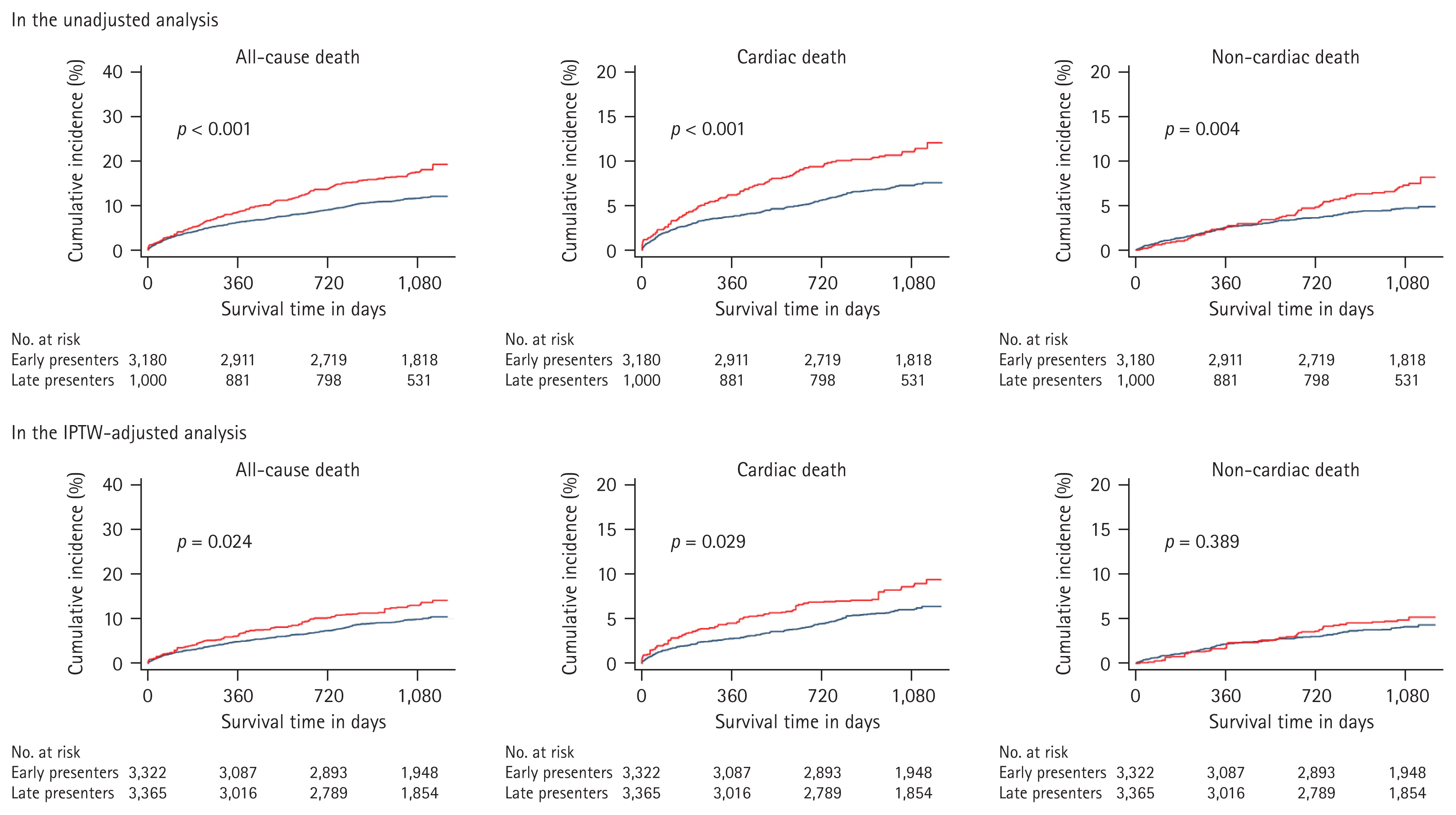
6. Cha JJ, Bae S, Park DW, et al. Clinical outcomes in patients with delayed hospitalization for non-ST-segment elevation myocardial infarction. J Am Coll Cardiol 2022;79:311ŌĆō323.

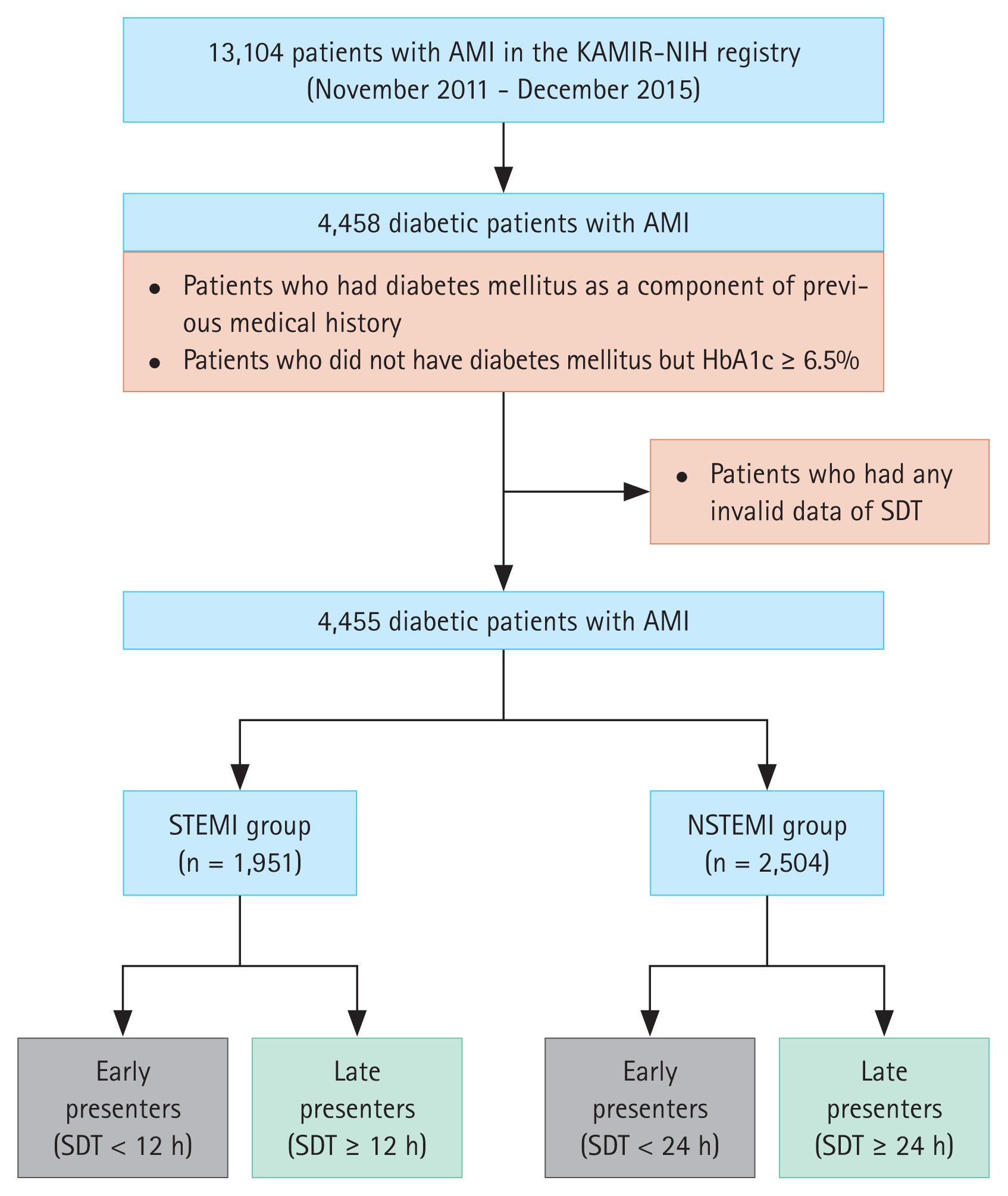
7. Kim JH, Chae SC, Oh DJ, et al.; Korea Acute Myocardial Infarction-National Institutes of Health Registry Investigators. Multicenter cohort study of acute myocardial infarction in Korea - interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health Registry. Circ J 2016;80:1427ŌĆō1436.


8. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191ŌĆō2194.


9. Ibanez B, James S, Agewall S, et al.; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119ŌĆō177.

10. Roffi M, Patrono C, Collet JP, et al.; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267ŌĆō315.


11. Stone GW, Brodie BR, Griffin JJ, et al. Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators. J Am Coll Cardiol 1998;31:23ŌĆō30.

12. Ellis SG, Vandormael MG, Cowley MJ, et al. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation 1990;82:1193ŌĆō1202.


13. Lee M, Kim DW, Park MW, et al. Gender differences in clinical outcomes of acute myocardial infarction undergoing percutaneous coronary intervention: insights from the KAMIR-NIH Registry. J Geriatr Cardiol 2020;17:680ŌĆō693.


14. Cho KH, Han X, Ahn JH, et al.; KAMIR-NIH Investigators. Long-term outcomes of patients with late presentation of ST-segment elevation myocardial infarction. J Am Coll Cardiol 2021;77:1859ŌĆō1870.


17. Brieger D, Eagle KA, Goodman SG, et al.; GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest 2004;126:461ŌĆō469.


22. Bailleul C, Aissaoui N, Cayla G, et al.; FAST-MI investigators. Prognostic impact of prepercutaneous coronary intervention TIMI flow in patients with ST-segment and non-ST-segment elevation myocardial infarction: results from the FAST-MI 2010 registry. Arch Cardiovasc Dis 2018;111:101ŌĆō108.


23. Karwowski J, Polo┼äski L, Gierlotka M, et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularisation. Kardiol Pol 2017;75:108ŌĆō116.


24. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC); Steg PG, James SK, et al.; Atar D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569ŌĆō2619.

27. Yoon CW, Oh H, Lee J, et al. Comparisons of prehospital delay and related factors between acute ischemic stroke and acute myocardial infarction. J Am Heart Assoc 2022;11:e023214.


28. Fu R, Li SD, Song CX, et al. Clinical significance of diabetes on symptom and patient delay among patients with acute myocardial infarction-an analysis from China Acute Myocardial Infarction (CAMI) registry. J Geriatr Cardiol 2019;16:395ŌĆō400.


29. Wackers FJ, Young LH, Inzucchi SE, et al.; Detection of Ischemia in Asymptomatic Diabetics Investigators. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care 2004;27:1954ŌĆō1961.

35. Avogaro A, Albiero M, Menegazzo L, de Kreutzenberg S, Fadini GP. Endothelial dysfunction in diabetes: the role of reparatory mechanisms. Diabetes Care 2011;34(Suppl 2):S285ŌĆōS290.


36. Burgess S, Juergens CP, Yang W, et al. Cardiac mortality, diabetes mellitus, and multivessel disease in ST elevation myocardial infarction. Int J Cardiol 2021;323:13ŌĆō18.


37. Kim YH, Her AY, Rha SW, et al. Effect of delayed hospitalization on 3-year clinical outcomes according to renal function in patients with non-ST-segment elevation myocardial infarction. Cardiol J 2023;May. 29. [Epub]. 10.5603/CJ.a2023.0036.


40. Panoulas V, Rathod KS, Jain AK, et al. Impact of early (Ōēż24 h) versus delayed (>24 h) intervention in patients with non-ST segment elevation myocardial infarction: an observational study of 20,882 patients from the London Heart Attack Group. Cardiovasc Revasc Med 2021;22:3ŌĆō7.


42. Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol 2008;52:1527ŌĆō1539.


44. Ib├Ī├▒ez B, Heusch G, Ovize M, Van de Werf F. Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol 2015;65:1454ŌĆō1471.


45. Kim MC, Jeong MH, Sim DS, et al.; KAMIR-NIH registry investigators. Optimal timing of percutaneous coronary intervention in patients with non-ST-segment elevation myocardial infarction complicated by acute decompensated heart failure (from the Korea Acute Myocardial Infarction Registry-National Institutes of Health [KAMIR-NIH]). Am J Cardiol 2018;121:1285ŌĆō1292.

46. Canto AJ, Kiefe CI, Goldberg RJ, et al. Differences in symptom presentation and hospital mortality according to type of acute myocardial infarction. Am Heart J 2012;163:572ŌĆō579.


47. Cho JY, Jeong MH, Ahn YK, et al.; Korea Acute Myocardial Infarction Registry Investigators. Comparison of outcomes of patients with painless versus painful ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:337ŌĆō343.


48. Fujino M, Ishihara M, Ogawa H, et al.; J-MINUET Investigators. Impact of symptom presentation on in-hospital outcomes in patients with acute myocardial infarction. J Cardiol 2017;70:29ŌĆō34.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement figure 1
Supplement figure 1 Print
Print


