INTRODUCTION
A meta-analysis of randomized controlled trials (RCTs) conducted in asymptomatic general population reported 34% reduction in gastric cancer incidence after
Helicobacter pylori eradication [
1]. Gastric cancer mortality risk also decreased by 33%, but a non-significant 9% increase in the overall mortality risk was found after
H. pylori eradication [
1]. A RCT in high-risk patients who underwent endoscopic resection for early gastric cancer reported a non-significant increased overall mortality risk among patients included in the
H. pylori treatment group (hazard ratio [HR], 1.95;
p = 0.19) despite a significant reduction of metachronous gastric cancer risk [
2]. A more recent meta-analysis also demonstrated a non-significant risk increase in overall mortality with
H. pylori treatment (risk ratio, 1.12; 95% confidence interval [CI], 0.93 to 1.34) [
3]. These data suggest a potential harmful effect of
H. pylori treatment in terms of increased non-gastric cancer mortality. However, the true nature of this observation and the plausible underlying mechanisms remain unclear.
Globally, the leading causes of death include ischemic heart disease and stroke and cancer [
4–
6]. A significant association between increased cardiovascular disease mortality and clarithromycin, which is a commonly used antibiotic for
H. pylori eradication, has been suggested [
7–
9]. Thus, we hypothesized that
H. pylori treatment might be associated with increased risk of mortality due to these major causes of death which might over-compensate the decrease of gastric cancer mortality. Type 2 diabetes is an important risk factor for cardiovascular disease, cerebrovascular disease, and cancers [
10,
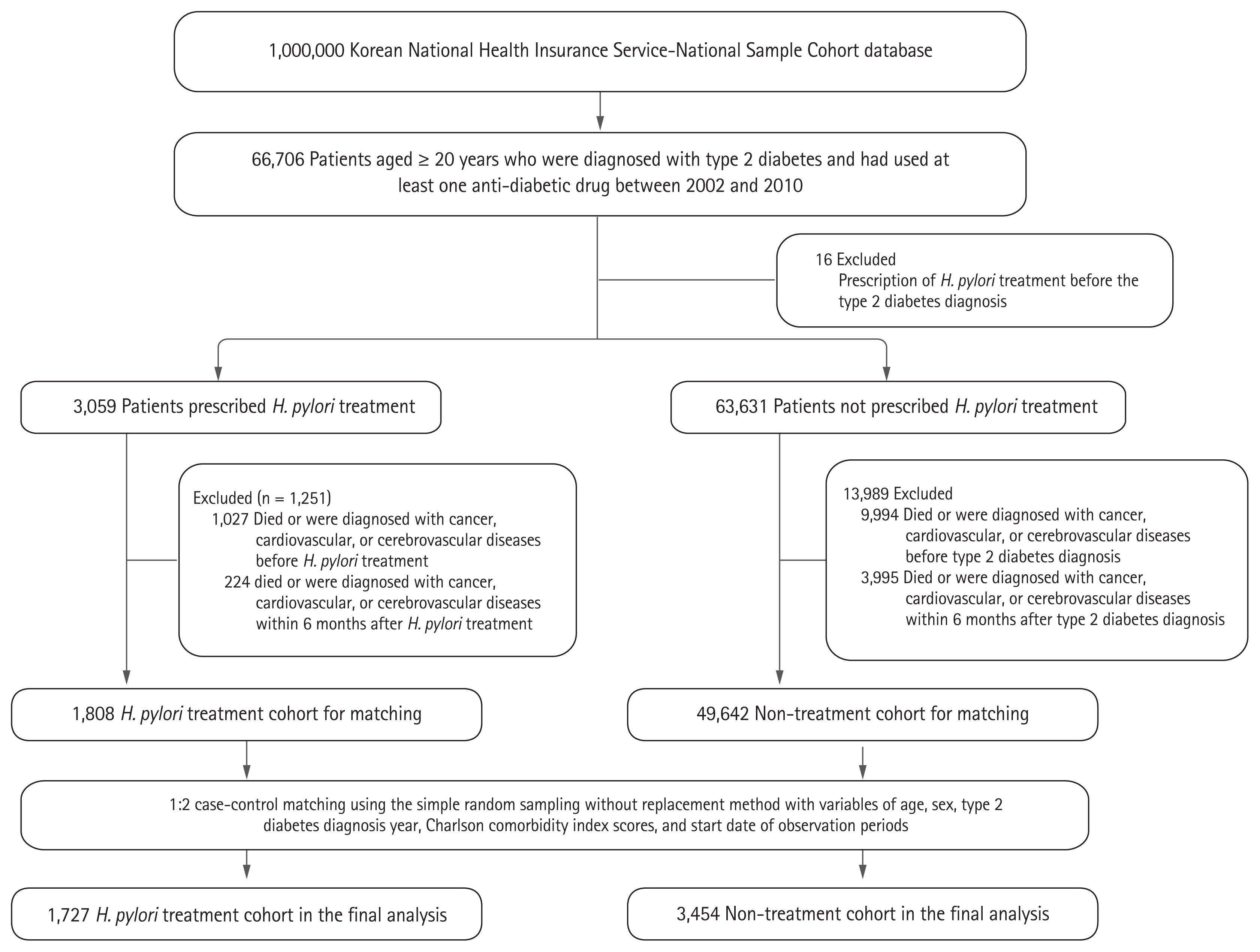
11]. In this retrospective cohort study, we investigated whether
H. pylori treatment is associated with overall mortality increase or with mortality increase from the main causes in patients with type 2 diabetes.
DISCUSSION
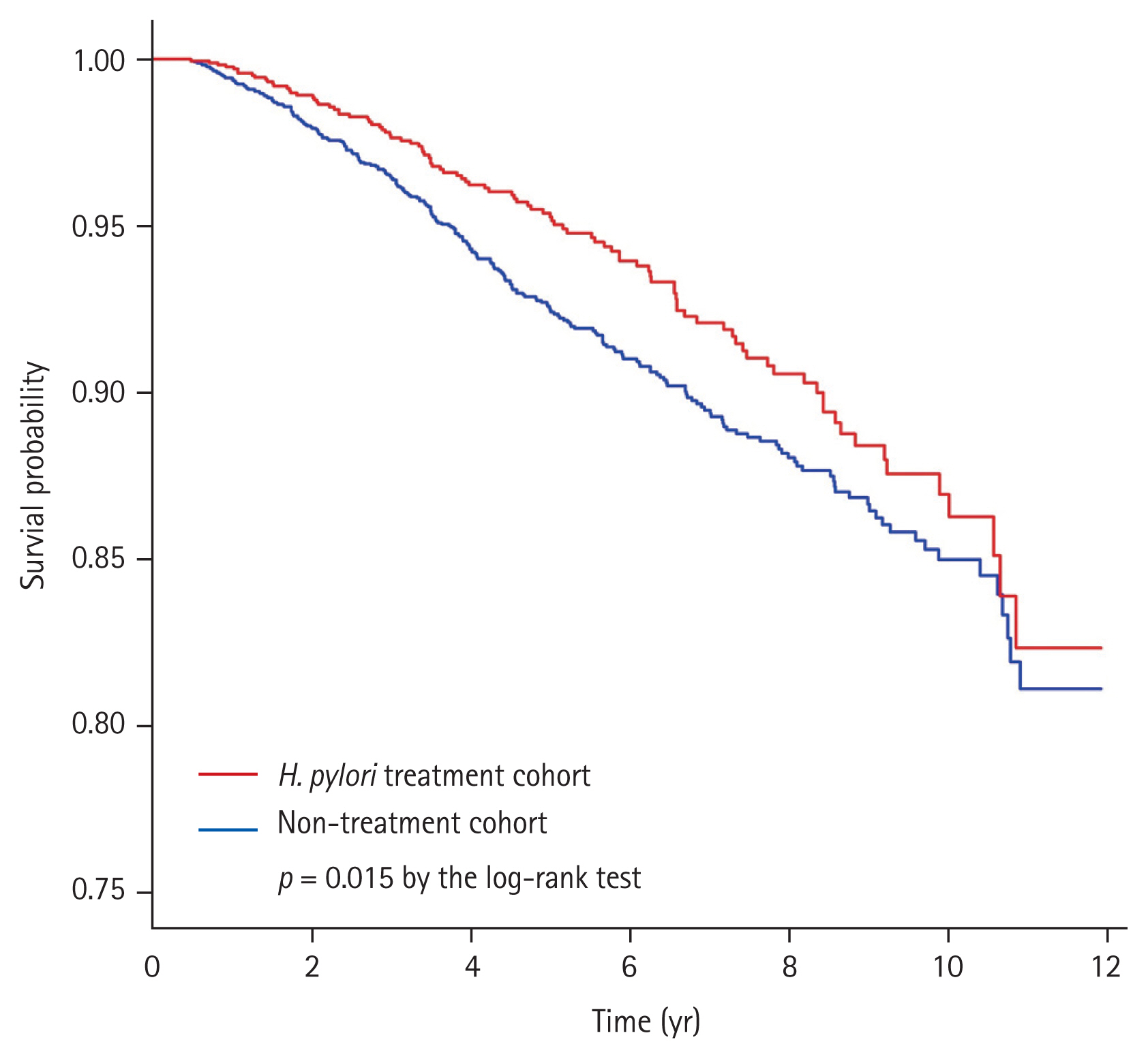
In this retrospective cohort study, we investigated overall mortality risk according to H. pylori treatment as the primary outcome, and evaluated cause-specific mortality risks due to major causes of death in patients with type 2 diabetes. H. pylori treatment was associated with a significant decrease in the risk of overall mortality. However, H. pylori treatment was not associated with mortality risks due to cardiovascular disease, cerebrovascular disease, and overall cancers.
In the report of global cancer statistics 2018 (GLOBOCAN 2018), gastric cancer was the fifth most common cancer, and the third leading cause of cancer death worldwide [
19].
H. pylori was classified as a group 1 carcinogen for gastric cancer by the International Agency for Research on Cancer [
20]. More than 50% of the world’s population (approximately 4.4 billion individuals) was infected with
H. pylori in 2015 [
21]. In Korea, gastric cancer was the most commonly diagnosed cancer in 2015 [
22], and the estimated prevalence of
H. pylori infection is about 54% [
21]. However,
H. pylori treatment as a primary prevention strategy for gastric cancer has not yet been implemented. Meta-analysis of RCTs showed 9% to 12% non-significant increase of overall mortality [
1,
3]. Of the two largest RCTs included in those meta-analyses, Wong et al. [
23] reported no increase in overall mortality risk (relative risk, 0.95; 95% CI, 0.53 to 1.69), whereas Ma et al. [
24] showed 10% non-significant increase of overall mortality risk (relative risk, 1.10; 95% CI 0.89 to 1.36). However, overall mortality was evaluated as a secondary outcome in the previous trials and no primary outcome study has been performed [
1,
23,
24]. Therefore, we evaluated the overall mortality after
H. pylori treatment as the primary study outcome in type 2 diabetes patients selected from the national cohort database who had increased cardiovascular or cerebrovascular disease risks. This database provides reliable data for mortality including exact date and cause of death. Overall mortality risk did not increase after
H. pylori treatment, and this result is similar to that of our previous study evaluating the association between overall mortality and
H. pylori treatment in a hypertension patient cohort [
16]. These results might be an evidence for supporting the use of
H. pylori treatment as a primary prevention strategy for gastric cancer.
In the present study, most of the patients (98.4%) in the
H. pylori treatment cohort received clarithromycin-containing standard triple therapy. A clinical trial reported that clarithromycin use for 2 weeks in stable coronary artery disease increased cardiovascular mortality and overall mortality risk during 10-year follow-up period, although the exact underlying mechanism is unknown [
7,
25,
26]. In addition, clarithromycin use was associated with increased risk of cardiovascular mortality during short-term periods, especially because of arrhythmia-related cardiovascular events [
9,
27]. Meanwhile, retrospective studies evaluating the association between mortality and clarithromycin use for
H. pylori treatment have reported inconsistent results [
28–
30]. A retrospective study demonstrated that overall mortality risk after clarithromycin-containing
H. pylori treatment significantly increased during a median follow-up of 3 years (aHR, 1.09; 95% CI, 1.00 to 1.18) [
28], whereas two studies did not show any increased risk in long-term overall mortality [
29,
30]. Previous studies included high-risk patients diagnosed with cardiovascular diseases (arrhythmia, ischemic heart disease, or heart failure) who might develop short-term adverse events or mortality associated with clarithromycin use [
28–
30]. We excluded patients with cardiovascular or cerebrovascular diseases before or within 6 months after
H. pylori treatment to avoid the short-term cardiovascular effects of clarithromycin use. In our study, the long-term cardiovascular mortality was not significantly associated with
H. pylori treatment, although almost all patients (98.4%) received a clarithromycin-containing standard triple regimen.
Our study showed that
H. pylori treatment was associated with increased risk in overall cancer incidence but reduced risk in overall cancer mortality. Previous studies reported that antibiotics use was associated with increased overall cancer risks [
31], and the risk of various cancers including lung, colon, prostate, and breast cancer [
31,
32]. One of the suggested mechanisms for increased cancer risks is disrupted gut microbiota (dysbiosis) by antibiotics use. Dysbiosis might have negative effects on the process of carcinogenesis including initiation, progression, and dissemination of cancer or cancer treatment efficacy [
33,
34]. However, in our study, significant increased risks were found only in colorectal cancer and thyroid cancer. In contrast, the colorectal cancer mortality risk did not increase, and no thyroid cancer mortality was observed. In Korea, colorectal cancer incidence also increased after the introduction of colorectal cancer screening program in 2004 with decreased trends of colorectal cancer mortality [
22,
35]. In addition, opportunistic thyroid cancer screening was associated with increased thyroid cancer incidence without a concomitant increase in thyroid cancer-related mortality [
36]. Thus, increased overall cancer incidence risk in the
H. pylori treatment cohort seemed to be associated with increased cancer screening. Another explanation for the increased risk of overall cancer incidence in the treatment cohort might be associated with higher economic status. Because the treatment cohort had a higher proportion of patients with household income level of > 50% than the non-treatment cohort, patients in the treatment cohort might have accessed more health-care services, including opportunistic health screening programs. Further prospective studies are needed to investigate whether short duration of antibiotics use for
H. pylori treatment (7 to 14 days) is associated with increased cancer risks due to dysbiosis.
Despite increased risks of cardiovascular disease and cancers in the
H. pylori treatment cohort, no increase in overall mortality risk and cause-specific mortality risks due to cardiovascular disease and cancers were observed. In addition to the
H. pylori treatment, the use of metformin (aHR, 0.56;
p < 0.001) and aspirin (aHR, 0.76;
p = 0.039) were significant factors associated with reduced overall mortality risk. These results might be explained by the healthy user bias, that is, health-seeking patients tend to initiate preventive therapies and try to engage in healthy lifestyle behaviors, and metformin users are more likely to be engaged in healthy behaviors [
37]. In the present study, healthy user bias might be present, and the treatment cohort had higher proportions of better household income levels, and metformin users.
Our study findings should be interpreted in light of several limitations. First, our study population was type 2 diabetes patients, and the severity of diabetes might have been different between the H. pylori treatment cohort and non-treatment cohort. The severity of diabetes could not be assessed because the NHIS-NSC database did not provide any laboratory data such as glycated hemoglobin or blood glucose level. Second, the severity and treatment results of cardiovascular disease, cerebrovascular disease, or cancers might affect overall or disease-specific mortality. However, we could not assess the information due to the limitation of the NHIS-NSC database. Third, compliance for the H. pylori treatment and H. pylori eradication status after the treatment were not available from the database. Thus, we could not analyze whether H. pylori eradication status after treatment affected overall mortality or not. Third, in the non-treatment cohort, both H. pylori infected patients who were not treated and those who were not infected were included. Finally, although we included aspirin and metformin use as the covariate to evaluate risks of incidence and mortality from cardiovascular disease, cerebrovascular disease, and cancers, several factors were not considered in our analyses such as the type of intervention treatment or other drugs including anti-platelet agents or statins.
In conclusion, H. pylori treatment in patients with type 2 diabetes was not significantly associated with increased overall mortality. Among the major causes of death, no significant increase in the risk of mortality due to cardiovascular disease, cerebrovascular diseases, or overall cancers were observed. However, long-term prospective trials are necessary to confirm our findings and to apply H. pylori eradication as a primary gastric cancer prevention strategy in the general population without concern of overall mortality increase.
KEY MESSAGE
In this population-based retrospective cohort study using the Korean National Health Insurance Service-National Sample Cohort database, long-term overall mortality risk was not increased after Helicobacter pylori treatment in patients with type 2 diabetes.
In addition, H. pylori treatment was not associated with mortality risk increase due to cardiovascular disease, cerebrovascular disease, and all cancers.
However, further long-term prospective trials are necessary to confirm our findings and to apply H. pylori eradication as a primary gastric cancer prevention strategy in the general population without concern of overall mortality increase.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print





