 |
 |
| Korean J Intern Med > Volume 30(2); 2015 > Article |
|
To the Editor,
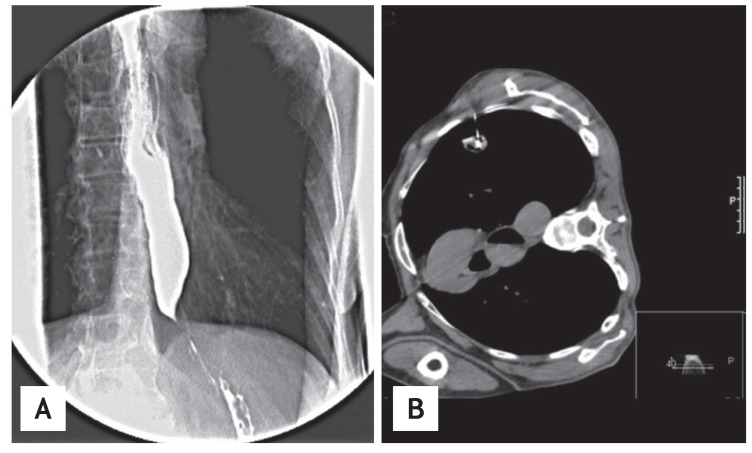
Pseudoachalasia is a rare entity and is difficult to distinguish from idiopathic achalasia. The most common cause of achalasia secondary to neoplasia is adenocarcinoma of the distal esophagus and the gastroesophageal junction. The second most common cause is small-cell lung cancer [1]. We report a case of lung adenocarcinoma secondary to achalasia. A 72-year-old man had dysphagia to liquids and solids, abdominal pain, gush-style vomiting without nausea, and a 10-kg weight loss over the past 6 months. He was vomiting immediately after eating. He had been diagnosed with opsomyoclonus and had a 60-year smoking history. Barium esophagography showed a proximal esophageal dilatation tapering into a "bird's beak" (Fig. 1A). Mild pressure was applied by the endoscope to open the gastroesophageal junction. Long time smoking history, older age, opsomyoclonus, and rapidly progressive achalasia symptoms-especially weight loss-indicate that cancer should be considered. Physical examination and chest imaging were normal, so we decided to screen for cancer by computed tomography (CT) scan. A thoracic and abdominal CT scan revealed esophageal dilatation and a spiculated lesion located in the left lung subpleural area. Botulinum toxin was injected endoscopically into the gastroesophageal junction, and the patient's symptoms improved. A transthoracic needle biopsy was performed by interventional radiology (Fig. 1B), and the diagnosis was lung adenocarcinoma. We referred the patient to the oncology department. Positron emission tomography-CT scan was performed by the oncology department for staging. There was bilateral mediastinal lymphadenopathy; therefore, the diagnosis was stage 3B lung cancer. Neoplasia causes achalasia by directly obstructing the lower esophageal sphincter and by paraneoplasia (depending on the antibodies) [2]. Direct involvement of the esophageal myenteric plexus is the most common mechanism, and endoscopic ultrasonography is a useful method to show tumor infiltration [3]. Type 1 antineuronal nuclear antibody (ANNA-1 or anti-Hu), type 1 Purkinje cell cytoplasmic antibody (PCA-1 or anti-Yo), and N-type calcium channel antibodies have been shown to be related to pseudoachalasia [1]. We do not have any serological or pathological evidence for pseudoachalasia and, therefore, cannot prove that it was present in this patient. CT scan and endoscopic examination did not suggest tumor invasion, so we thought that paraneoplasia was the cause of achalasia. Some clinical differences have been noted between idiopathic achalasia and pseudoachalasia. Three criteria were identified by Tucker et al. [4] to distinguish pseudoachalasia from primary achalasia: age older than 50 years, symptoms with a duration of less than 1 year, and rapid weight loss. Weight loss is more rapid at the onset of pseudoachalasia symptoms than at those of idiopathic achalasia, and pseudoachalasia occurs in older patients [4]. Patients with idiopathic achalasia commonly have a long duration of symptoms before being diagnosed [5]. Pseudoachalasia in lung cancers frequently arises during the course of small-cell carcinoma [1]. As in the reported case, it occurs more rarely with lung adenocarcinoma. In particular, the possibility of malignancy should be investigated in a patient of advanced age with achalasia accompanied by rapidly developing symptoms and in patients without a detectable lesion of the distal esophagus or adjacent structures.
References
1. Lee HR, Lennon VA, Camilleri M, Prather CM. Paraneoplastic gastrointestinal motor dysfunction: clinical and laboratory characteristics. Am J Gastroenterol 2001;96:373–379PMID : 11232678.


2. Gockel I, Eckardt VF, Schmitt T, Junginger T. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol 2005;40:378–385PMID : 16028431.


3. Lee TH, Cho JY. Sonographic evaluation of esophageal achalasia. Korean J Intern Med 2014;29:262. PMID : 24648815.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



