 |
 |
| Korean J Intern Med > Volume 28(3); 2013 > Article |
|
Abstract
Background/Aims
Several prognostic markers for heart failure (HF) have been determined but the importance of liver function tests (LFTs) remains unknown. The aim of this study was to determine the prognostic significance, if any, of abnormal LFTs in acute decompensated HF.
Methods
All adult patients (> 18 years of age) who were admitted to a community hospital with a diagnosis of acute decompensated HF during the period January 2008 to December 2009 were identified. Exclusion criteria included acute coronary syndrome, active hepatobiliary disease, renal failure (serum creatinine Ōēź 2 mg/dL), and malignancy. The primary end point was readmission secondary to acute exacerbation of HF. The Cox proportional hazard model was used for statistical analyses.
Results
Univariate analysis showed that serum total bilirubin (TB, p < 0.01), serum B-type natriuretic peptide (p < 0.05), ejection fraction (EF, p < 0.05), and heart rate (p < 0.05) were significant predictors of hospital readmission secondary to acute decompensated HF. Multivariate analysis showed that high serum TB (> 1.3 mg/dL) on admission was an independent predictor (p < 0.05) of hospital readmission secondary to HF. The 'at-risk' group-patients with serum TB > 1.3 mg/dL and/or EF < 35% on admission-had a readmission rate that was 87% ┬▒ 20% (p < 0.05) higher than those with neither criterion.
Heart failure (HF) is the most common cause of hospitalization among people older than 64 years in the United States [1,2]. About 25% of these patients are readmitted within 30 days after discharge [2]. Several risk factors for readmission secondary to HF have been identified in previous clinical studies.
To improve mortality and shorten hospital stays, there is a need to identify predictors of poor prognosis, at earlier stages of HF, so that more aggressive therapy can be initiated sooner. Abnormal liver function tests (LFTs) on admission are common in HF patients, secondary to passive hepatic congestion and low perfusion to the liver, resulting from altered hemodynamics [3,4].
The role of abnormal LFTs in determining poor prognosis and early future readmission secondary to HF has not been extensively investigated previously. The aim of this study was to determine the prognostic significance of abnormal LFTs in HF for early future readmission, secondary to acute exacerbation of HF.
This was a retrospective study in which the medical records of all patients older than 18 years admitted to a community hospital in Scranton, Pennsylvania, with acute exacerbation of HF during the period January 2008 to December 2009 were reviewed. Acute exacerbation of HF was diagnosed based on clinical findings, chest X-ray, serum B-type natriuretic peptide (BNP) levels, and transthoracic echocardiography. Patients with acute coronary syndrome, active hepatobiliary disease, renal failure (serum creatinine Ōēź 2 mg/dL), and malignancy on admission were excluded. All study subjects were followed retrospectively until December 2010 to monitor for readmission secondary to HF. Readmitted patients were identified using the diagnostic codes in the hospital medical records.
Patients were not followed prospectively because this was a retrospective study. The primary end point was readmission or in-hospital death, secondary to acute exacerbation of HF. In total, 187 patients were recruited initially; 17 were then excluded based on the exclusion criteria. This study was approved by the Institutional Review Board.
Blood samples for basal metabolic profile and LFTs were drawn from the peripheral vein of the patients at the time of hospital admission. Plasma concentrations of BNP in the venous blood samples were determined using point-of-care fluorescence immunoassay with a Triage BNP test kit (Biosite Diagnostics Inc., San Diego, CA, USA). Serum aspartate transaminase, serum alanine transaminase, serum alkaline phosphatase, serum total bilirubin (TB), and serum direct bilirubin were tested at the hospital's core laboratory. Hyperbilirubinemia was defined as serum TB > 1.3 mg/dL. A transthoracic echocardiogram was performed during the study hospital admission or within the 4 months prior to the study admission.
The Cox proportional hazard model was used to determine clinical variables that were independent predictors of survival. Links with readmission times were analyzed and p values were calculated using the log-rank method; the Breslow method was used for ties in the data. Clinical variables with a p value Ōēż 0.05 in the univariate analysis were examined using multivariate analysis in a Cox proportional hazard model.
Two variables were transformed prior to analysis. Ejection fraction (EF; corrected) was recorded as the number of 5% steps below 50% or zero if EF Ōēź 50%. The other transformed variable, serum TB (corrected), was recorded as the number of mg/dL beyond 1.0 mg/dL. Negative values were recorded as zero for both variables.
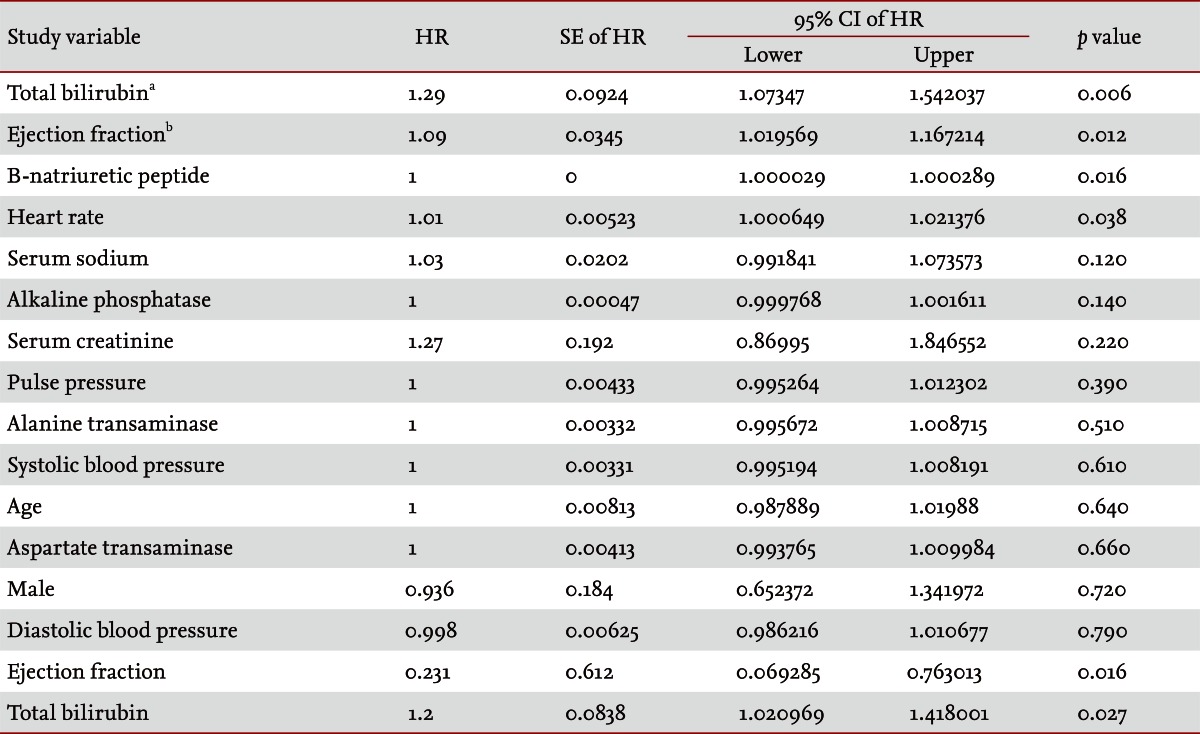
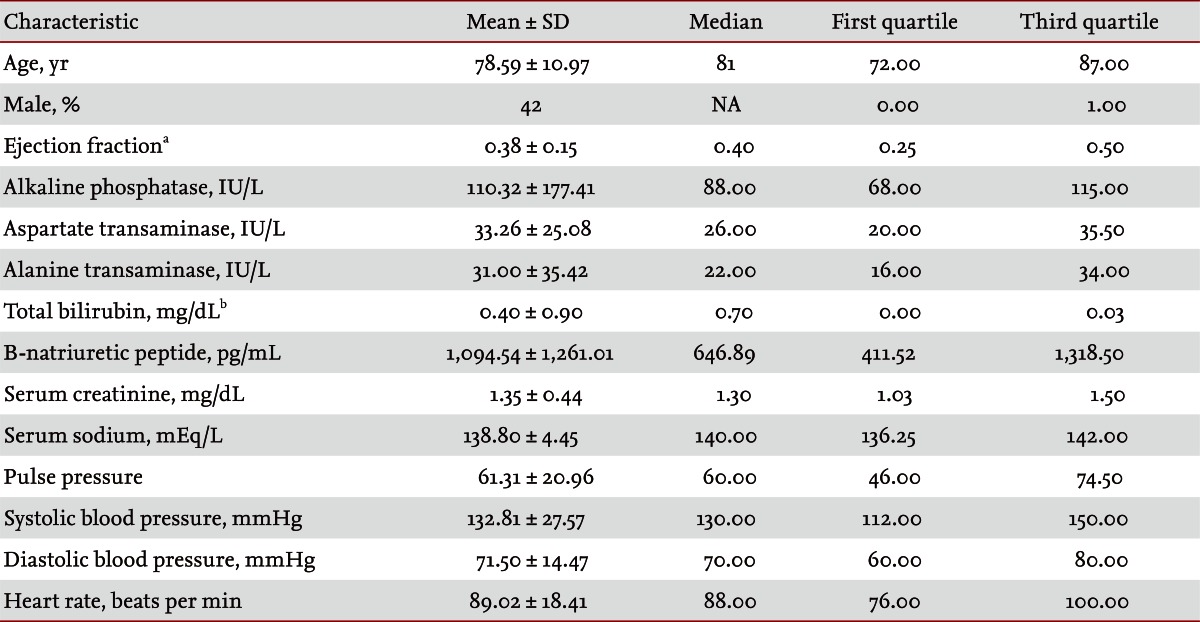
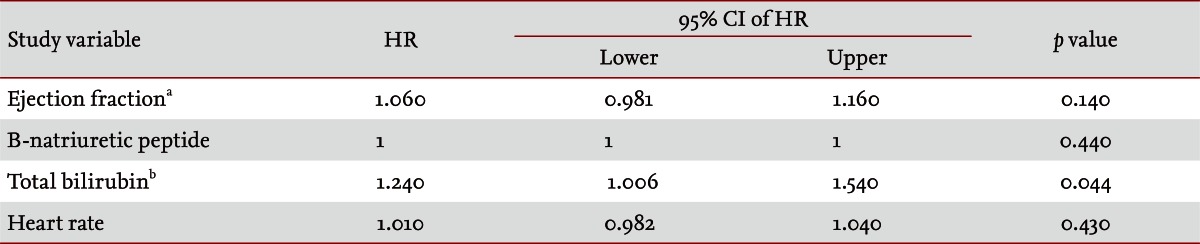
The mean age of the patients was 78.5 ┬▒ 11 years. Of the 170 patients, 42% were males. The means, medians, and standard deviations of the study variables for the total population are presented in Table 1. In total, 122 patients were readmitted secondary to acute decompensated HF during the study period. Serum TB (p < 0.01), serum BNP (p < 0.05), EF (p < 0.05), and heart rate (p < 0.05) were found to be significant predictors of hospital readmission secondary to acute decompensated HF on univariate analyses (Table 2). Multivariate analysis showed that serum TB (> 1.3 mg/dL) on admission was an independent predictor (p < 0.05) of hospital readmission secondary to HF (Table 3). One patient died in the hospital due to cardiac arrest and one patient was transferred to a hospice. The remaining patients were discharged from the hospital after appropriate treatment of their congestive HF. LFTs were performed on admission and data were extracted from patient medical records. LFTs were neither checked at the time of discharge nor during postdischarge follow-up.
Age, gender, systolic blood pressure, diastolic blood pressure, serum sodium, serum creatinine, serum alkaline phosphatase, and serum aspartate transaminase on admission were not significant predictors of readmission secondary to HF.
We stratified the population into two nonoverlaping groups: group A consisted of patients with serum TB >1.3 mg/dL on admission and group B, of patients with serum TB Ōēż 1.3 mg/dL. The resulting Kaplan-Meier curve (Fig. 1) shows the percentages of the populations that were not readmitted over time. In fact, patients with serum TB > 1.3 mg/dL on admission had a readmission rate that was 78% ┬▒ 20% (p < 0.01) higher at any given time than those with serum TB Ōēż 1.3 mg/dL (of 31 patients with TB > 1.3 mg/dL, 29 were readmitted during the study period; of 121 patients with serum TB Ōēż 1.3 mg/dL, 80 patients were readmitted during the study period).
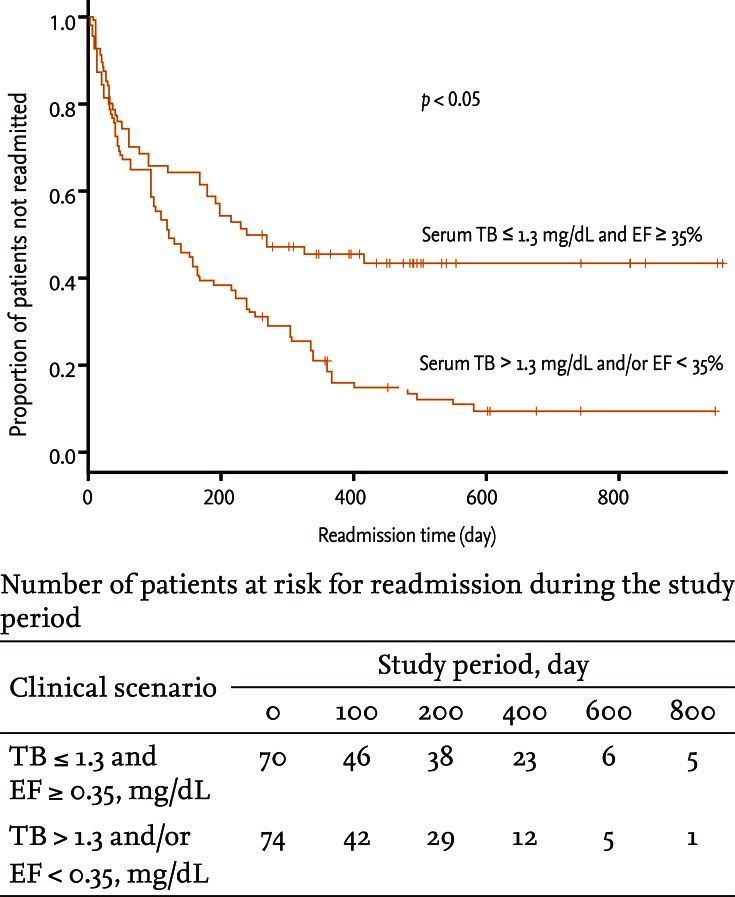
Further analysis was performed by considering the two most significant covariates. The population was again split into two groups. The first (group 1) consisted of patients with serum TB > 1.3 mg/dL and/or an EF < 35% on admission, and this represented the 'at-risk' stratum. The second group (group 2) consisted of all other patients, with serum TB Ōēż 1.3 mg/dL and EF Ōēź 35%. The 'at-risk' group had a readmission rate that was 87% ┬▒ 20% (p < 0.05) higher than those without either criterion (of the 74 patients with serum TB > 1.3 mg/dL and/or an EF < 35% on admission, 64 were readmitted during the study period). In group 2 (serum TB Ōēż 1.3 mg/dL and EF Ōēź 35%), of the 70 patients, 39 were readmitted during the study period. A Kaplan-Meier curve is shown in Fig. 2.
Congestive hepatopathy is a common manifestation of acute decompensated HF. Although typically asymptomatic, it is characterized by abnormal LFTs. The most common biochemical abnormality in congestive hepatopathy, secondary to acute decompensated HF, is a mildly elevated serum bilirubin level, occurring in ~70% of cases [4]. The precise cause of this hyperbilirubinemia is unclear. Several contributing factors have been proposed, including hemolysis, pulmonary infarction, medication, and hepatocellular dysfunction. Serum bilirubin levels were reported to correlate with right atrial pressures but not with cardiac output [5]. Batin et al. [6] showed that serum aspartate transaminase and serum bilirubin had better prognostic significance in chronic HF.
Ischemic liver injury occurs when there is imbalance between oxygen delivery and demand [7]. Serum bilirubin has been shown to be more sensitive to hemodynamic disturbance than transaminases in patients with left HF [8]. One study showed that serum bilirubin had prognostic significance in patients with chronic HF with left ventricular EF Ōēż 40% [9]. Our study included patients who had both systolic and diastolic dysfunction and the diagnosis of HF was based principally on the clinical judgment of different clinicians (using clinical, biochemical, and radiological data). Other biochemical liver tests may be elevated, based on the severity of the damage to the liver, secondary to HF. The degree of elevation of transaminases in ischemic liver injury due to decreased cardiac input correlates with the extent of zone 3 necrosis seen in liver biopsy specimens [10]. Follow-up LFTs on discharge or during postdischarge follow-up would strengthen the results of our study; this could perhaps be performed as part of a future prospective study.
Our data suggest that in patients with acute decompensated HF, elevated serum TB on admission, with or without low EF (< 35%), predicted worse prognosis and early future readmission, secondary to HF. Elevated serum bilirubin levels could probably serve as a surrogate marker of elevated right heart pressures in congestive HF. In the absence of expensive and invasive hemodynamics data, it could serve as a useful predictor of future outcomes in this complex patient subset.
A limitation of our study is that its nonrandomized, retrospective nature and inclusion of only a single community hospital. More prospective follow-up studies with larger sample sizes are needed to confirm our results.
1. Elevated serum bilirubin is the most common biochemical abnormality in congestive hepatopathy secondary to acute decompensated heart failure.
2. In the absence of expensive and invasive hemodynamics data, serum bilirubin can serve as a useful predictor of future outcomes in patients with acute decompensated heart failure.
References
1. Liu L. Changes in cardiovascular hospitalization and comorbidity of heart failure in the United States: findings from the National Hospital Discharge Surveys 1980-2006. Int J Cardiol 2011;149:39ŌĆō45PMID : 20060181.


2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418ŌĆō1428PMID : 19339721.


3. Lau GT, Tan HC, Kritharides L. Type of liver dysfunction in heart failure and its relation to the severity of tricuspid regurgitation. Am J Cardiol 2002;90:1405ŌĆō1409PMID : 12480058.


4. Dunn GD, Hayes P, Breen KJ, Schenker S. The liver in congestive heart failure: a review. Am J Med Sci 1973;265:174ŌĆō189PMID : 4573728.


5. Sherlock S. The liver in heart failure: relation of anatomical, functional, and circulatory changes. Br Heart J 1951;13:273ŌĆō293PMID : 14848381.



6. Batin P, Wickens M, McEntegart D, Fullwood L, Cowley AJ. The importance of abnormalities of liver function tests in predicting mortality in chronic heart failure. Eur Heart J 1995;16:1613ŌĆō1618PMID : 8881855.


7. Fuhrmann V, Kneidinger N, Herkner H, et al. Hypoxic hepatitis: underlying conditions and risk factors for mortality in critically ill patients. Intensive Care Med 2009;35:1397ŌĆō1405PMID : 19506833.


8. Allen LA, Felker GM, Pocock S, et al. Liver function abnormalities and outcome in patients with chronic heart failure: data from the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) program. Eur J Heart Fail 2009;11:170ŌĆō177PMID : 19168515.



Figure┬Ā1
The Kaplan-Meier survival curves show significant differences in heart failure readmissions between the groups. Upper curve, of the 121 patients with serum total bilirubin (TB) Ōēż 1.3 mg/dL, 80 were readmitted within the study period. Lower curve, of the 31 patients with TB > 1.3 mg/dL, 29 were readmitted during the study period.

Figure┬Ā2
The Kaplan-Meier survival curves show significant differences in heart failure readmissions between the groups. Upper curve, of the 70 patients with serum total bilirubin (TB) Ōēż 1.3 mg/dL and ejection fraction (EF) Ōēź 35%, 39 were readmitted during the study period. Lower curve, of the 74 patients with serum TB > 1.3 mg/dL and/or an EF < 35% on admission, 64 were readmitted during the study period.
Table┬Ā2
Univariate analysis of clinical variables for hospital readmission secondary to acute decompensated heart failure
-
METRICS

- Related articles
-
Perioperative and anesthetic management of patients with rheumatoid arthritis2022 July;37(4)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


