 |
 |
| Korean J Intern Med > Volume 20(2); 2005 > Article |
|
Abstract
Plasmacytomas are a localized proliferation of plasma cells in the bone marrow, and are less frequently seen in extraosseous organs or tissues. Extramedullary plasmacytoma is a rare malignant neoplasm, and is especially uncommon when it arises from the mediastinum. Here, we report on a case of posterior mediastinal extramedullary plasmacytoma in a 64-year-old man. He was admitted with an asymptomatic right apical mediastinal mass, which was provisionally diagnosed as a neurogenic mass. However, a subsequent investigation revealed that this tumor was a rare case of IgG kappa type extramedullary plasmacytoma arising from the posterior mediastinum. The patient was treated with local radiation to the mediastinum and is doing well without further evidence of disease.
Malignant plasma cell dyscrasias are caused by the proliferation and differentiation of B lymphocytes into autonomous clones of immunoglobulin-producing plasmacytoid cells. Dalrymple and Bence-Jones first identified a plasma dyscrasia in 1846 when they described a condition with diffuse bone pain and marked proteinuria. However, it was not until 1873 that Rustizky et al. successfully recognized this condition as a distinct histopathologic entity: multiple myeloma1). Since then, this plasma cell neoplasm has been classified into one of two categories, namely, multiple myeloma, in which the cancer cells are found in the bone marrow, or extramedullary plasmacytoma (EMP), in which the cancer cells develop in tissues other than bone marrow. EMP is a rare soft tissue plasma cell tumor, and it usually presents as a mass within the upper respiratory tract2). It is most unusual for this condition to present in the posterior mediastinum as a primary solitary lesion. In this case report, we describe a patient who was provisionally diagnosed as having a neurogenic tumor, but subsequent investigations revealed this tumor to be an EMP arising from the posterior mediastinum.
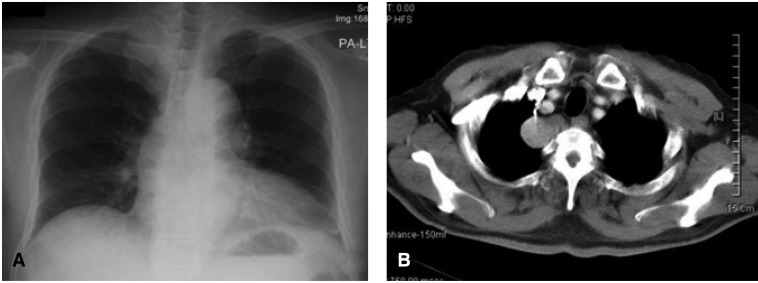
A 64-year-old man was referred to the pulmonary department of Korea University Ansan Hospital for an evaluation of a lung mass. He had received a medical checkup 1 month previously, when the mass-like lesion was incidentally found on plain chest X-ray. He was asymptomatic and had well controlled hypertension and diabetes; he also had a smoking history of 40 pack-years. On physical examination, no palpable lymphadenopathy or other abnormality was noted. His hemoglobin, white cell count, platelets, urea and electrolytes, glucose, liver function tests, and serum calcium were normal. The plain chest X-ray revealed a smooth marginated 3├Ś4 cm sized mass-like lesion in the right upper mediastinal area (Figure 1A). Chest computerized tomographic (CT) studies, performed after the intravenous administration of a contrast agent, revealed a 2.5├Ś2 cm sized, well defined, bilobed, homogeneously enhancing mass lesion in the right upper posterior mediastinum (Figure 1B). No definite evidence of bony erosion of the thoracic vertebrae was observed. On magnetic resonance imaging (MRI), the tumor was visualized as a homogeneous signal intensity mass with a signal intensity similar to muscle on T1-weighted images, whereas on T2-weighted images, the signal intensity was moderately higher than that of muscle. Moderate heterogeneous enhancement was noted with gadolinium-enhancement (Figure 2).
A provisional diagnosis of neurogenic tumor was made and percutaneous needle aspiration was performed for diagnosis. However, the histologic examination showed aggregates of small round cells. Therefore, a right lateral mediastinotomy was performed for a confirmatory diagnosis. Histologically, the tumor was characterized by a well circumscribed proliferation of plasma cells (Figure 3A). Immunohistochemical staining was positive for IgG and kappa light chain (Figure 3C), but not for lambda chain. The tumor cells were positive for CD79a (a pan-B cell marker) (Figure 3B), and CD45, and were negative for CD3 (a pan-T cell marker) and cytokeratin, which was consistent with plasma cell differentiation. Based on these findings, the tumor was diagnosed as a plasmacytoma. We investigated the possibility of multiple myeloma. Serum protein electrophoresis analysis showed a monoclonal gamma globulin peak of 1.8 g/dL (0.6~1.7 g/dL), and serum immunoelectrophoresis revealed IgG kappa type monoclonal gammopathy, but this was insufficient to meet the diagnostic criteria of multiple myeloma. Surveys for a skeletal lesion, bone marrow biopsy, and Bence-Jones protein in urine were all normal. 99mTc-scintigraphy did not detect any other systemic lesions. Accordingly, multiple myeloma was ruled out, and the patient was finally diagnosed as having EMP of the posterior mediastinum. The patient received treatment with 40 Gy of radiation for five consecutive weeks to a field covering the right upper mediastinum. Six months after his diagnosis, the patient is doing well without further evidence of disease.
EMP represents approximately 3% of all plasma cell neoplasms3,4). The median age of patients suffering from this malady is 60 years, and 75% are men2). These tumors can occur at any site, but almost 90% develop in the head and neck area, with a predilection for the upper respiratory tract. Rare sites of involvement include the gastrointestinal tract, liver, spleen, pancreas, and other organs such as breast, testis, or skin2). It is most unusual for this tumor to present in the posterior mediastinum as a primary solitary lesion.
In the presented case, the patient was admitted for an incidentally discovered upper posterior mediastinal mass. On plain x-ray, neurogenic tumor seemed the most likely diagnosis. However, a needle aspiration biopsy revealed aggregates of small round cells, and the subsequent histologic examination of the excised mass revealed EMP consisting of monoclonal plasma cells. Primary EMP arising from the posterior mediastinum is rare, few similar cases have been reported in the medical literature5,6).
A diagnosis of EMP requires the demonstration of a monoclonal plasma cell infiltrate without any evidence of multiple myeloma elsewhere. The diagnosis of multiple myeloma is generally based on three clinical findings: 1) histologic evidence of a plasmacytoma or plasmacytosis of the bone marrow (at least 10%); 2) clinical evidence of disease such as bone pain, anemia, or renal failure; and 3) serum (3 g/dL of monoclonal serum protein) or urine (>1 g/day) monoclonal gammopathy or the presence of osteolytic bone lesions by radiographic studies. In the present case, increased levels of serum monoclonal protein were observed, but these were documented as under 3 g/dL. Monoclonal protein can be detected in the serum or urine of approximately 25% of patients7). CT and MRI have been reported to be useful radiological modalities for the diagnosis of plasmacytoma. The tumor mass usually appears homogenous with well-defined margins, and it shows slight to moderate enhancement following the introduction of contrast material8).
Plasma cell neoplasms are relatively sensitive to radiation, and surgical resection is commonly combined with radiotherapy. Radiation doses of 40 to 50 Gy over 4 to 5 weeks are associated with less than a 5% risk of local recurrence9-11), and no local recurrences were observed with radiation doses of at least 45 Gy4). As a result, EMP has a relatively favorable prognosis, and most carefully staged patients with solitary extramedullary plasmacytoma can be cured. At least 70% of these patients remain disease-free at 10 years, and most patients with EMP die of unrelated causes2). However, local recurrence is observed in 30% of cases, and signs of dissemination were observed in 40%12). One report concerned two cases of EMP presenting as a mediastinal mass, which preceded the onset of full-blown multiple myeloma13). An increase in the baseline levels of serum monoclonal proteins or urinary Bence-Jones protein may signify the recurrence of primary disease or it may indicate the onset of multiple myeloma. Furthermore, dissemination into multiple myeloma has been reported to occur in 10~30% of extramedullary plasmacytoma cases within the first 2 years14). Thus, close long-term follow-up by the physician is considered appropriate and necessary.
References
1. Ching AS, Khoo JB, Chong VF. CT and MR imaging of solitary extramedullary plasmacytoma of the nasal tract. AJNR Am J Neuroradiol 2002;23:1632ŌĆō1636PMID : 12427612.


2. Dimopoulos MA, Kiamouris C, Moulopoulos LA. Solitary plasmacytoma of bone and extramedullary plasmacytoma. Hematol Oncol Clin North Am 1999;13:1249ŌĆō1257PMID : 10626148.


3. Knowling MA, Harwood AR, Bergsagel DE. Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol 1983;1:255ŌĆō262PMID : 6668499.


4. Shih LY, Dunn P, Leung WM, Chen WJ, Wang PN. Localised plasmacytomas in Taiwan: comparison between extramedullary plasmacytoma and solitary plasmacytoma of bone. Br J Cancer 1995;71:128ŌĆō133PMID : 7819027.



5. Alekseenko AV, Slivka VP, Iatskiv VV. Plasmacytoma of the posterior mediastinum. Klin Khir 1984;10:64. PMID : 6513309.
6. Ganesh M, Sankar NS, Jagannathan R. Extramedullary plasmacytoma presenting as upper back pain. J R Soc Promot Health 2000;120:262ŌĆō265PMID : 11197455.


7. Galieni P, Cavo M, Avvisati G, Pulsoni A, Falbo R, Bonelli MA, Russo D, Petrucci MT, Bucalossi A, Tura S. Solitary plasmacytoma of bone and extramedullary plasmacytoma: two different entities? Ann Oncol 1995;6:687ŌĆō691PMID : 8664190.


8. Rodriguez-de-Velasquez A, Weber AL, Montgomery W. Extramedullary laryngeal plasmacytoma. Ann Otol Rhinol Laryngol 1996;105:483ŌĆō486PMID : 8638902.


9. Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R. Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol 1999;52:245ŌĆō249PMID : 10580871.


10. Mayr NA, Wen BC, Hussey DH, Burns CP, Staples JJ, Doornbos JF, Vigliotti AP. The role of radiation therapy in the treatment of solitary plasmacytomas. Radiother Oncol 1990;17:293ŌĆō303PMID : 2343147.


11. Mill WB, Griffith R. The role of radiation therapy in the management of plasma cell tumors. Cancer 1980;45:647ŌĆō652PMID : 6153562.


12. Holland J, Trenkner DA, Wasserman TH, Fineberg B. Plasmacytoma: treatment results and conversion to myeloma. Cancer 1992;69:1513ŌĆō1517PMID : 1540888.


Figure┬Ā1
Plain chest roentgenography (A) showed a smooth, marginated 3├Ś4 cm sized mass-like lesion on the right upper mediastinal area. Chest computed tomographic (CT) with enhancement (B) revealed a 2.5├Ś2 cm sized, well defined bilobed, homogeneously enhancing mass lesion, in the right upper posterior mediastinum. No definite evidence of bony erosion of thoracic vertebrae was noted.
Figure┬Ā2
Magnetic resonance imaging (MRI) revealed a tumor of homogeneous signal intensity with a signal intensity similar to that of muscle on T1-weighted images (A). Moderate heterogeneous enhancement was observed after introducing gadolinium contrast (B).

Figure┬Ā3
Microscopically, the tumor consisted of extensively infiltrating, diffuse sheets of mature and immature plasma cells with eccentric, pleomorphic nuclei, nucleoli, and variably stained cytoplasm (A) (Hematoxylin and eosin stain, ├Ś400). Immunohistochemical staining showed that the neoplastic plasma cells were reactive for CD79a B-cell marker (B) and had kappa monoclonality (C). (Immunohistochemical stain: CD79a, ├Ś400 and kappa light chain, ├Ś400)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



