INTRODUCTION
Renal artery dissection may be caused by iatrogenic injury, trauma, underlying arterial diseases such as fibromuscular disease, atherosclerotic disease, or connective tissue disease. Often, renal artery dissection is detected during diagnostic work-up for malignant hypertension, acute flank pain, or renovascular hypertension in the chronic stage1). Some patients do well with conservative treatment, while others need emergent or urgent surgery1-3). Treatment is chosen based on the patient's hemodynamic status, renal function, and the feasibility of treatment modality2). Here we report a case of renal infarction that came about as a consequence of renal artery dissection and also discuss the proper treatment modality.
CASE REPORT
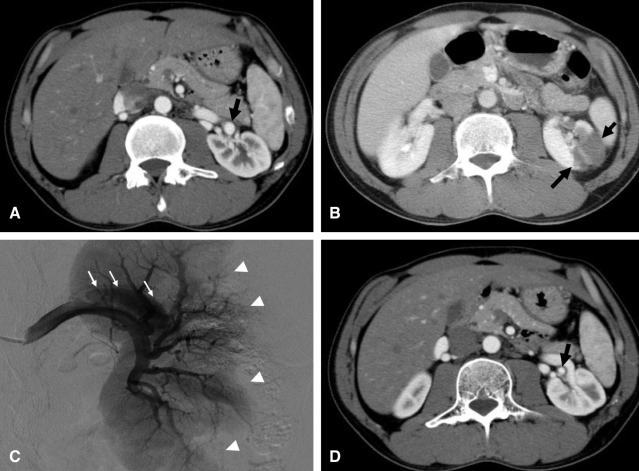
A 38-year-old male presented to our clinic with a history of persistent left flank pain. Three days before admission, while intoxicated with alcohol, he slipped on the bathroom floor. Other than that, there was no unusual medical history. His blood pressure was 128/72 mmHg. Physical examination revealed severe tenderness at the left costovertebral angle. Laboratory indices were as follows: hemoglobin 15.6 g/dL, white blood cell count 12.08x103/┬ĄL, platelet count 24.1├Ś104/┬ĄL, blood urea nitrogen 17 mg/dL, creatinine 0.97 mg/dL, and LDH 980 IU/L (normal, 218-472 IU/L). Urinalysis showed negative dip stick for protein and blood, with normal urine sediment. Electrocardiography showed normal sinus rhythm. Contrast-enhanced computed tomography (CT) scan showed a small aneurysm (arrow) in the distal portion of the left renal artery (Figure 1A). In addition, a well-demarcated, non-enhanced left kidney parenchyma (arrow) was demonstrated, suggesting infarction (Figure 1B). Renal angiography demonstrated a dissecting aneurysm of the left renal artery (arrow) and multiple filling defects along the peripheral portion of left kidney (arrowhead) (Figure 1C). Since the patient was hemodynamically stable, and his pain was gradually subsiding, we treated him conservatively. Two months later, on follow-up CT, a focal pseudoaneurysm was still present at the same site on the left renal artery (arrow), while the previously infarcted region of the left kidney had resolved completely, leaving only some parenchymal scarring (Figure 1D).
DISCUSSION
Renal artery injury is a rare complication of blunt abdominal trauma. However, exercise and sports activities have been associated with renal artery dissection in cases where the dissection was considered secondary to anatomical variation or acceleration/deceleration injury to the renal artery and subsequent intimal tearing4, 5). In the presented case, there was no anatomic variation of the renal artery on radiologic studies, so we hypothesized that the dissection was related to acceleration/deceleration injury to a normal renal artery.
An isolated renal artery dissection may be suspected in patients complaining of severe flank pain after blunt abdominal trauma6). Radiological imaging may be helpful in detecting renal artery pathology, such as renal artery dissection. For patients with acute, isolated renal artery dissection, surgical treatment, endovascular management, or medical treatment have been considered as measures to preserve renal function7). M├╝ller et al.1) reported that renal artery dissection can be treated with surgical revascularization. Their indications for surgical intervention were organ preservation and the treatment or improvement of a patient's renovascular hypertension1). Recently, Lee et al.2) reported the case of a patient who had renal artery dissection complicated by renal infarction, that was successfully treated using endovascular management for salvaging the renal parenchyma. The patient's lesion was easily accessible using percutaneous angioplasty and stent.
Management of renal artery dissection remains controversial. Surgical revascularization after renal artery dissection requires skillful expertise because of perivascular inflammation and scarring potentially present in the diseased renal artery segment. Before planning surgical revascularization, careful preoperative examination may be necessary to evaluate the precise pathologic status of the diseased renal artery segment1). Endovascular intervention of the renal artery has largely been used to treat renal artery stenosis in renovascular hypertension. Recently, its use in cases of arterial dissection has increased. However, the feasibility and effectiveness of this modality in treating renal artery dissection has not been confirmed2). Moreover, if renal function and vital signs are normal, invasive treatment such as surgical or endovascular revascularization may not be necessary, because medical treatment alone with strict blood pressure control is as effective as surgical management3, 8). Beroniade et al.9) also suggested that surgery should be reserved as a second-line modality. In our case, renal angiography was performed for diagnosis of renal infarction, but no revascularization of renal artery dissection was performed. Because of the patient's stable vital signs and normal renal function, we elected to manage him conservatively. Follow-up CT showed that the infarcted area of the left kidney was recovering with small cortical scarring, while the patient's blood pressure remained normal.
In conclusion, physician should take the patient's medical status into consideration when deciding treatment modality for renal artery dissection. When renal function is normal, medical treatment rather than surgical or endovascular revascularization may be sufficient.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





