 |
 |
| Korean J Intern Med > Volume 22(4); 2007 > Article |
|
Abstract
A 48-year-old woman who was without any abnormal past medical history underwent colonoscopy as a screening procedure for colorectal disease. The procedure was uneventful and there was no sign of inflammation around the appendicular orifice or the luminal surface of the cecum. The patient did not complain of pain or significant discomfort throughout the procedure. She then developed pain in the right lower quadrant of the abdomen that evening and this persisted for four days. She visited the outpatient department and underwent abdominal ultrasonography, which showed a swollen appendix with a collection of pericecal fluid. Surgical exploration and appendectomy were performed; the final diagnosis was acute suppurative appendicitis. Colonoscopists should be aware of this rare complication and consider it when making the differential diagnosis of post-colonoscopy abdominal pain.
Colonoscopy is usually performed to identify or correct a problem in the colon and distal small bowel, and its clinical applications have increased enormously in recent years. Intestinal perforation and hemorrhage are well-known complications of colonoscopy, but the incidence of these problems is very low1, 2). Furthermore, the incidence of appendicitis caused by a colonoscopic examination is very rare. The first such case was reported in 1988 by Houghton and Aston3), and there have been only a few reports since then. The usual pathogenesis of appendicitis involves obstruction of the orifice of this organ. Fecaliths, lymphoid hyperplasia, foreign bodies and parasites can block the inner lumen, leading to increased intraluminal pressure, impaired blood flow and inflammation. Barium remnants after a barium enema examination can also induce luminal obstruction. Here we describe a 48-year-old woman who developed acute appendicitis immediately after colonoscopy.
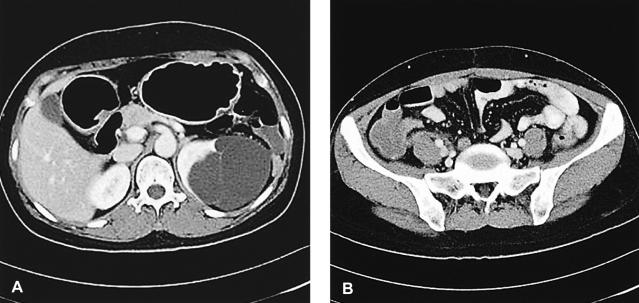
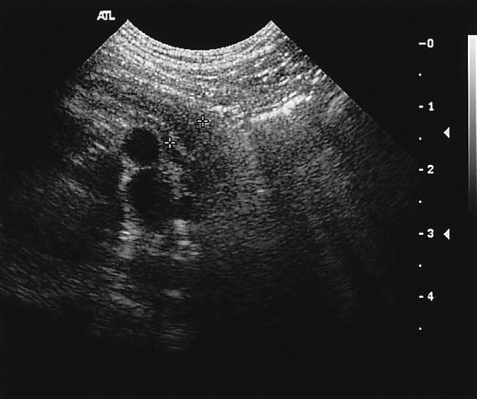
A 48-year-old woman underwent colonoscopy for colorectal disease screening at a health care center. She was healthy and had no medical problems before the procedure. She also had a computed tomographic (CT) scan of the abdomen performed before the colonoscopic examination, which revealed no abnormalities except for a 7├Ś6 cm multilobulated left renal cyst (Figure 1). Before the procedure, the patient took three liters of polyethylene glycol for bowel preparation. The patient was conscious after an intravenous injection of 50 mg meperidine. Intubation into the cecum was performed without any difficulties within 10 minutes. The bowel preparation was excellent and good visualization of the cecal landmarks was obtained. There was no sign of inflammation around the cecum or the appendicular orifice (Figure 2). She felt well after the colonoscopic examination, and she was discharged promptly after passing bowel gas. However, that evening, she felt a right lower abdominal pain that gradually intensified.
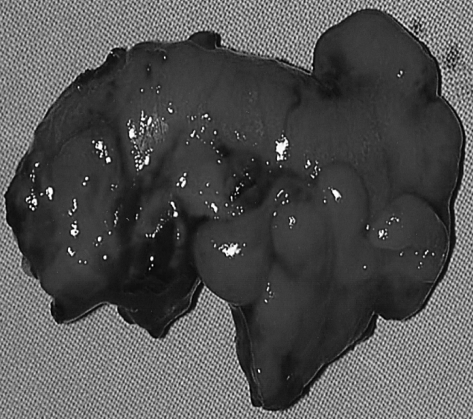
Four days later, she visited our outpatient department with complaints of right lower abdominal pain. Her vital signs were stable with a body temperature of 37Ōäā. The abdomen was slightly distended with right lower quadrant tenderness and rebound tenderness. The initial white blood cell count was 7,300 cells/mm3 with 5,100 neutrophils/mm3; the other blood profiles (hemoglobin, hematocrit and the platelet count) and tests for liver function, electrolytes and urinalysis were within normal limits. The chest and abdominal radiographic findings showed no abnormalities. Acute appendicitis was suspected, and so ultrasonography was performed for making an accurate diagnosis. The results showed a swollen appendix with pericecal fluid accumulation and inflammation of the terminal ileum and cecum (Figure 3).
Surgical exploration and appendectomy were performed. The appendix was about 5.5 cm long, 1 cm wide and phlegmonous. The lumen was filled with fecal material (Figure 4). Histological examination revealed acute suppurative appendicitis with focal mucosal hyperplasia (Figure 5). The postoperative course was uneventful and the patient was discharged three days after surgery.
Colonoscopy is useful as a diagnostic and therapeutic tool for colorectal disease. It is a relatively safe procedure, but it has some risks. Major complications such as bleeding, colonic perforation and postpolypectomy syndrome are rare. Other minor complications such as abdominal pain, nausea, vomiting, bowel spasm and mucosal tears in the lining of the colon can occur frequently1, 2). This procedure can on rare occasions lead to splenic rupture, pneumomediastinum, pneumothorax, incarcerated hernia, ileus and diverticulitis. More often, hemodynamic alterations that occur during colonoscopy may be the cause of cardiovascular and cerebrovascular sequelae1, 2).
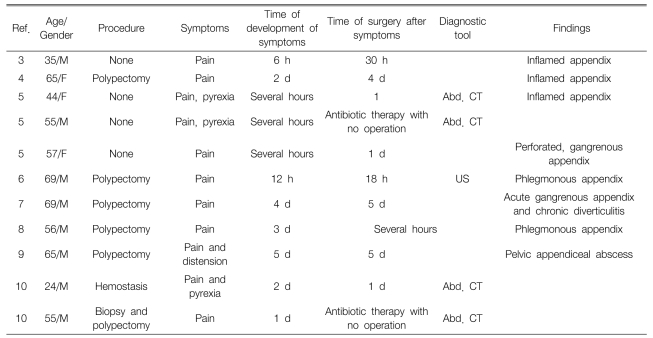
Acute appendicitis after colonoscopy is a very rare complication. Houghton and Aston3) firstly described appendicitis as a rare complication of colonoscopy, and only 12 cases of acute appendicitis following colonoscopy have currently been reported in the English medical literature (Table 1)3-9). Vender, et al.5) reported on three cases that occurred at two institutions where a total of about 8000 colonoscopic examinations were performed. Therefore, the incidence of appendicitis following colonoscopy was about 0.038%. This is lower than the incidence of bleeding (0.21%), colonic perforation (0.1%) or abdominal pain (0.09%)2) after colonoscopy. Because abdominal pain after colonoscopy is generally caused by retained gas or colonic spasm secondary to colonoscopy2), it is not easy to suspect acute appendicitis as the cause of this pain. It is also important to distinguish appendicitis from post-polypectomy syndrome, which is a combination of pain, peritoneal irritation, leukocytosis and fever after colonoscopy7, 8).
Among the 12 reported cases, there were eight men and four women with a mean age of 53.5 years (range: 24-69). This high mean age may be because colonoscopy is generally performed on patients during their fifth and sixth decades. Most patients commonly present with right lower abdominal or suprapubic pain, with or without fever and chilling. One unusual case revealed only abdominal pain and distension with ileus10). In nine patients, these symptoms developed between several hours and two days after colonoscopic examination, but the symptoms occurred after two days in the other three patients. Ten patients underwent surgery and two were treated with antibiotics and supportive care. Four of the ten patients underwent surgery four days after the development of symptoms, and three showed a perforated appendix, which suggests that a delayed diagnosis may increase the likelihood of perforation.
Acute appendicitis is thought to be mainly caused by luminal obstruction, like the so called barium appendicitis after a barium enema, and this can occur by obstruction of the appendiceal orifice via the retention of barium11, 12). The suggested mechanisms of appendicitis after colonoscopy are 1) pre-existing subclinical disease of the appendix5), 2) elevation of the intraluminal pressure with insufflated air can obstruct the luminal orifice by lengthening the appendix, 3) elevated intraluminal pressure can force bowel contents, and especially fecaliths, into the appendix6), 4) direct intubation of the colonoscope into the appendiceal lumen can induce inflammation5) and 5) mucosal injury around the appendiceal orifice can cause local edema and obstruction of the appendiceal lumen10). Seven of the reported cases suggested the importance of the procedure's duration because therapeutic procedures such as polypectomy and hemostasis are lengthy. The second and third mechanisms described above may be the causes in our case.
In conclusion, appendicitis is a very rare but important complication of colonoscopy and this can be easily confused with other complications of the procedure. Prompt recognition of this complication can lead to early, effective treatment, and delayed diagnosis can lead to serious results. Therefore, clinicians should always keep the possibility of this complication in mind as the cause of abdominal pain after performing colonoscopic examination.
References
1. McHardy G. In: Berk JE, ed. Appendix. Bockus gastroenterology 1985. 4th ed. Philadelphia: WB Saunders, 2609ŌĆō2624.
2. Viiala C, Zimmerman M, Cullen DJ, Hoffman NE. Complication rates of colonoscopy in an Australian teaching hospital environment. Intern Med J 2003. 33:355ŌĆō359PMID : 12895166.


3. Houghton A, Aston N. Appendicitis complicating colonoscopy. Gastrointest Endosc 1988. 34:489. PMID : 3234692.

4. Brandt E, Naess A. Acute appendicitis following endoscopic polypectomy. Endoscopy 1989. 21:44. PMID : 2917538.


5. Vender R, Larson J, Garcia J, Topazian M, Ephraim P. Appendicitis is a rare complication of colonoscopy. Gastrointest Endosc 1995. 41:514ŌĆō516PMID : 7615235.


6. Hirata L, Noguchi J, Yoshikawa I, Tabaru A, Nagata N, Murata I, Itoh H. Acute appendicitis immediately after colonoscopy. Am J Gastroenterol 1996. 91:2239ŌĆō2240PMID : 8855760.

7. Lipton S, Estrin J. Postcolonoscopy appendicitis: a case report. J Clin Gastroenterol 1999. 28:255ŌĆō256PMID : 10192615.


8. Takagi Y, Abe T. Appendicitis following endoscopic polypectomy. Endoscopy 2000. 32:S49. PMID : 10935805.

9. Srivastava V, Pink J, Swarnkar K, Feroz A, Stephenson B. Colonoscopically induced appendicitis. Colorectal Dis 2004. 6:124ŌĆō125PMID : 15008912.


Figure┬Ā1
Abdominal computed tomography performed before colonoscopy showed a 7├Ś6 cm multilobulated left renal cyst (A), but no inflammation in the appendix (B).
Figure┬Ā2
The colonoscopy showed non-specific findings of the cecum and no inflammation at the appendiceal orifice.

Figure┬Ā3
Abdominal ultrasonography performed after the patient complained of right lower abdominal pain showed an inflamed appendix with a pericecal fluid collection and inflammation of the terminal ileum and cecum.
Figure┬Ā4
The postoperative findings revealed a phlegmonous appendicitis. On cross section, the lumen of the appendix was filled with fecal material.



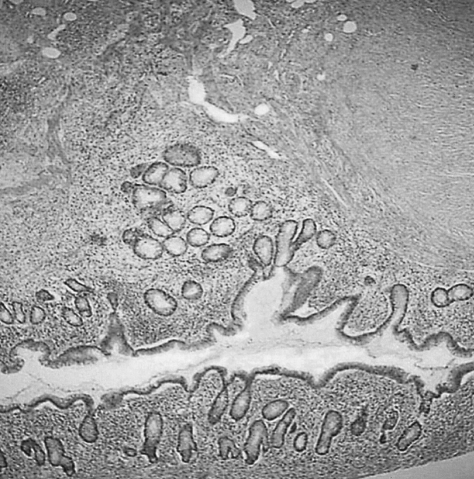
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



