 |
 |
| Korean J Intern Med > Volume 40(6); 2025 > Article |
|
Abstract
Global population aging has substantially increased in the number of older adults who undergo kidney replacement therapy (KRT). Age-related physiological changes and functional dependence in this population lead to the multifaceted clinical and ethical challenges associated with KRT. Geriatric syndromes, including functional impairment, frailty, malnutrition, and multi-morbidity, can influence the choice of dialysis modality and modify dialysis prescriptions, often resulting in patients requiring assistance with dialysis implementation. Although dialysis remains a key life-sustaining therapy, the limited life expectancy and multiple comorbidities of older adults increase the risk of adverse outcomes, supporting the consideration of conservative kidney management as an alternative. Furthermore, because many older adults prioritize quality of life and reduced treatment burdens over longevity and biochemical targets, dialysis-related decisions should be tailored to individual preferences and goals. Shared decision-making involving older patients, their caregivers, healthcare professionals, and nephrologists is essential for determining the most appropriate treatment approach. This review addresses the clinical considerations in decision- making regarding dialysis and proposes optimal treatment strategies tailored to the unique needs of older patients with chronic kidney disease.
As the global population continues to age, the incidence of end-stage kidney disease (ESKD) among older adults has increased in many countries [1,2]. Most of them require kidney replacement therapy (KRT), such as dialysis or kidney transplantation. However, older adults are generally not considered suitable candidates for kidney transplantation, resulting in a gradual increase in the number of older patients undergoing dialysis. According to the Korean Renal Data System (KORDS), patients aged ≥ 65 years have accounted for more than half of the total dialysis population in Korea since 2018 [3]. Older patients undergoing dialysis have a high prevalence of adverse clinical outcomes. From 2013 to 2023, hospitalization rates were the highest among individuals aged ≥ 75 years, and all-cause mortality increased in this group while it declined in younger populations [4]. These trends highlight the growing importance of individualized management strategies for older adults undergoing dialysis.
Physiological age with well-preserved physical function is likely more clinically relevant than chronological age or longevity for quality of life in older patients [5]. Collectively, frailty, malnutrition, and multimorbidity are used to define the physiological age of older adults. In older adults requiring dialysis, these age-related conditions can influence the choice of dialysis modality and lead to changes in dialysis prescriptions as well as often result in patients requiring assistance with treatment implementation. Therefore, physicians play a key role in supporting older patients in making decisions about dialysis initiation and modalities and establishing treatment strategies tailored to patients’ clinical status. This review addresses clinical considerations in dialysis decision-making and proposes optimal treatment strategies tailored to the unique needs of older patients with chronic kidney disease (CKD). This review focuses primarily on issues related to dialysis therapy in the treatment management of older adults with ESKD, with the exception of kidney transplantation.
In general, dialysis improves both the quality of life and survival of patients with advanced CKD compared to conservative management [6,7]. However, several studies have found that the survival benefit of dialysis over conservative management tends to disappear in patients aged > 80 years [6,7]. Early mortality within the first 120 days after hemodialysis (HD) initiation remains higher in older patients than in younger patients [8]. In older adults with limited life expectancy, dialysis may not offer a survival benefit and could be potentially harmful. In this context, conservative kidney management (CKM), in which supportive care and symptom- focused treatment are provided without dialysis, may be an alternative for older adults with limited life expectancy [9]. Therefore, whether CKM or dialysis is more appropriate for older patients with limited life expectancy who require KRT must be determined.
Prediction tools and scoring systems can help guide risk stratification for mortality and progression to ESKD in older patients with CKD stages 3b–5 and support individualized decision-making for KRT initiation. In 2017, the European Renal Best Practice (ERBP) guidelines recommended a stepwise approach using validated tools to estimate kidney failure and mortality risks (Fig. 1, Supplementary Table 1) [10]. This framework advises physicians to assess both the 5-year mortality risk using Bansal scores and the risk of progression to kidney failure using the Kidney Failure Risk Equation (KFRE) [11,12]. When the mortality risk is high, CKM is generally considered more appropriate than KRT. Conversely, a high KFRE score combined with a low mortality risk may support early preparation for KRT, whereas a low KFRE score favors continued nephroprotective care without immediate KRT. When patients are expected to initiate KRT within 3–6 months, their Renal Epidemiology and Information Network scores can be used to estimate short-term mortality after dialysis initiation, helping physicians and patients more accurately weigh the potential benefits and burdens of dialysis [13]. However, these models and guidelines were developed based on European cohorts and have not been specifically adapted for use in Korean clinical settings. To address this issue, To address this issue, the Korean Society of Geriatric Nephrology recently developed a 6-month mortality prediction model for patients aged ≥70 years requiring HD, using data from a multicenter retrospective cohort including 16 institutions in Korea [14]. Further development of prediction models based on Korean data could improve clinical decision-making and support dialysis planning tailored to the older Korean population.
The preferences of older patients and their caregivers are important when deciding whether to initiate dialysis. Although dialysis is a vital life-sustaining therapy, it can cause burdens and adverse effects, such as fatigue, repeated needle punctures, frequent hospitalizations, and high maintenance costs [15]. Some older patients with advanced CKD prioritize their care goals and values over longevity and prefer CKM to avoid complications. In addition, caregivers of older patients, who are usually family members, play a key role in the decision-making process for dialysis because they share patients’ physical, psychological, and financial burdens [16]. They provide practical support for peritoneal dialysis (PD), assist with transportation to HD units, and often act as primary decision-makers for older patients with cognitive impairment. Therefore, shared decision-making (SDM) involving patients, caregivers, and healthcare providers is essential throughout the course of treatment from the initiation of dialysis to its maintenance and withdrawal. SDM can help close medical information gaps among patients, caregivers, and clinicians, support patient-centered decisions, and promote patients’ decisional autonomy [17].
Age is a well-established risk factor for unplanned dialysis because older patients tend to delay decisions regarding dialysis initiation and fail to achieve mature vascular access (VA) [18]. Unplanned dialysis initiation in older adults is associated with higher mortality and hospitalization risks [19,20]. Therefore, accurate prediction of progression to kidney failure and timely initiation of dialysis are essential for older patients.
Accurate assessment of kidney function in older patients is essential to determine the optimal timing of dialysis. However, serum creatinine levels and uremic symptoms may not be reliable indicators of kidney failure in this population. Serum creatinine has inherent limitations as a marker of glomerular filtration because non-glomerular filtration rate (GFR) determinants, such as muscle mass, tubular secretion, and dietary intake, influence its accuracy. In older patients with frailty and sarcopenia, estimated GFR (eGFR) is over-estimated due to reduced muscle mass and low creatinine levels. Given these limitations, the 2024 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines recommend using the combined creatinine-cystatin C equation (eGFRcr-cys) in clinical situations in which creatinine generation is reduced due to low muscle mass or creatinine secretion or extrarenal elimination is altered by specific medications [21]. Therefore, the eGFRcr-cys equation is recommended for assessing kidney function in older adults.
The KDIGO 2024 clinical practice guidelines recommend that decisions regarding dialysis initiation be based on a composite assessment of uremic symptoms and signs, quality of life, preferences, kidney function, and laboratory abnormalities [21]. The guidelines emphasize that clinical circumstances that require dialysis initiation typically occur when eGFR falls between 5 and 10 mL/min/1.73 m2. However, the decision should primarily be guided by clinical signs, symptoms, and overall patient condition rather than eGFR alone. Assessment of uremic symptoms in older patients is particularly challenging. Symptoms such as cognitive impairment, fatigue, anorexia, and pruritus are often subjective and nonspecific in this population. Furthermore, these symptoms can overlap with comorbidities commonly observed in older adults, including cardiovascular disease, neurocognitive disorders, and psychiatric conditions, making true uremic manifestations difficult to distinguish. Therefore, careful clinical observation and differentiation of uremic signs and symptoms from those related to other comorbidities are essential when considering dialysis initiation in older adults.
HD and PD have no absolute contraindications, except when VA cannot be established or the peritoneal membrane is nonfunctional in older patients. In general, dialysis modality selection is based on comorbidities, occupational and lifestyle factors, and the need to preserve residual kidney function (RKF). In older adults, additional factors such as functional impairment, multiple comorbidities, and familial support should be considered because they may further influence the advantages and disadvantages of each modality.
The advantages of PD include RKF preservation, feasibility of home-based dialysis, and improved cardiovascular stability. However, functional impairments associated with frailty and aging may increase the risk of peritonitis, particularly in relation to malnutrition and difficulties in performing PD procedures [22,23]. Poor performance status often prevents older adults from performing PD independently; thus, they require caregiver assistance. Regarding HD, patients benefit from prompt medical attention from physicians and can maintain social relationships through regular hospital visits. However, HD requires patients and their caregivers to spend additional time and financial costs on transportation to dialysis facilities. Moreover, older adults, especially those with cardiovascular disease or impaired immune function, are vulnerable to intradialytic hypotension (IDH) and dialysis-related bloodstream infections.
In older patients with ESKD, the effects of dialysis modality on mortality risk must be considered when making appropriate treatment decisions [24]. A recent meta-analysis revealed that PD has a higher mortality rate than HD in patients aged ≥ 60 years, particularly among those with diabetes, comorbidities, or prolonged dialysis duration. However, the difference in mortality risk between the two modalities appears to have diminished in studies conducted after 2010 [25]. Furthermore, a nationwide retrospective cohort study using data from the Korean National Health Insurance Service demonstrated that PD was associated with higher mortality rates than HD between 2004 and 2015 [26]. However, between 2012 and 2015, the mortality rate of PD became comparable to that of HD, regardless of age ≥ 65 years, diabetes status, or comorbidity burden. This improvement may be attributable to advancements in PD solutions and techniques and improvements in the management of cardiovascular complications.
In Korea, HD centers are unevenly distributed between urban and rural areas, and a substantial proportion of older patients live in rural areas. These patients often face a high risk of falls during transportation to HD facilities. Therefore, in older patients with a favorable physiological status who do not have diabetes or other major comorbidities, PD can be a practical and appropriate treatment strategy, particularly in Korean healthcare settings. Thus, an assisted PD system that provides a model of care in which trained healthcare personnel or caregivers support patients in performing PD at home needs to be established to increase PD adoption [27].
Arteriovenous fistula (AVF) is generally preferred over other types of VA because of its lower risks of complications, infection, and mortality, as well as superior patency compared to arteriovenous graft (AVG) [28,29]. Trends in VA creation have shifted from the “fistula-first” approach outlined in the 2006 Kidney Disease Outcomes Quality Initiative (KDO-QI) guidelines to the “patient-first” approach in the updated 2019 guidelines [30]. The 2019 KDOQI guidelines recommend the use of a long-term central venous catheter (CVC) or AVG over AVF in patients with limited life expectancy or restricted vascular anatomy. Older adults frequently present with poor vascular anatomy and multiple comorbidities that contribute to reduced life expectancy. The 2023 KORDS showed that among older patients in Korea, the proportion of AVF tended to decrease with age, whereas those of AVG and CVC increased [4].
AVF is the preferred type of VA because of its superior long-term patency and lower complication rates. However, AVF requires a longer maturation period and is associated with a higher primary failure risk [31]. The high prevalence of diabetes, peripheral vascular disease, and anatomic restrictions makes older patients particularly vulnerable to primary failure of AVF [32]. The high risk of maturation failure may increase the likelihood of death before successful AVF use in older patients with limited life expectancy. In contrast, a CVC-only strategy enables prompt dialysis initiation and avoids unnecessary procedures related to arteriovenous (AV) access (Table 1). Furthermore, AVG allows for early cannulation to ensure timely dialysis initiation and serves as a catheter-sparing option [33,34]. Therefore, CVC and AVG may be more suitable than AVF for older patients with a limited life expectancy who are at high risk for AVF failure.
Patients undergoing HD with CVC have poorer survival rates than those with other AV access [33,35,36]. However, a selection bias may be present in older patients. Older adults often remain dependent on CVCs without transitioning to AV access owing to their short life expectancy and multiple comorbidities. Thus, their lower survival rates may not be entirely attributable to CVC use [37]. A retrospective study from the Korean insurance claims data found that the mortality rate between AVF and AVG was not significantly different in patients aged ≥85 years [29]. Therefore, when treating older patients, nephrologists and vascular surgeons should take a patient-centered approach rather than strictly follow the “fistula-first” strategy in older patients.
Almost all patients undergoing HD follow a standard thrice-weekly schedule from the start, whereas those undergoing PD typically adjust dialysis doses incrementally based on a decline in RKF [38]. RKF gradually declines after dialysis initiation, regardless of modality; therefore, an approach similar to “incremental HD” can be applied to PD. In incremental HD, dialysis starts at a reduced dose, such as twice-weekly or three hours per session, and gradually increases to the standard thrice-weekly, four hours per session, to compensate for progressive RKF loss (Fig. 2) [39]. Furthermore, the prescriptions of the size of dialyzer membrane, dialysate volume, and blood flow rate can be adjusted over time to maintain dialysis adequacy.
The incremental HD strategy may be suitable for older patients with low dietary intake and interdialytic weight gain (IDWG) because preserved RKF can compensate for skipped or shortened dialysis sessions. An incremental approach allows older patients to adjust gradually to the dialysis procedure and its associated complications, such as post-dialysis fatigue and muscle cramps. Furthermore, it reduces the frequency of hospital visits, thereby alleviating the burden on both patients and their caregivers, particularly for patients without a nearby HD facility.
Two pilot randomized controlled trials (RCTs) reported that incremental HD preserves RKF and reduces hospitalization rates without deteriorating metabolic derangements or increasing mortality compared with standard thrice-weekly HD in incident patients with RKF undergoing HD [40,41]. However, these studies did not specifically focus on older patients. In Korea, a pragmatic RCT has been underway since November 2021 to compare clinical outcomes, including mortality, hospitalization, and quality of life, between incremental HD with an initial twice-weekly schedule and conventional thrice-weekly HD in incident HD patients aged ≥ 60 years [42]. The findings from this and other ongoing RCTs are expected to support the clinical benefits and feasibility of an individualized approach to incremental HD in older patients (Table 2) [43–47].
Timely adjustments to the HD dose according to the patient’s decline in RKF are essential to prevent underdialysis. This requires regular assessment of RKF through urea clearance and other biomarkers, close monitoring of nutritional and fluid status, ongoing evaluation of patient adherence to dialysis schedules, and proactive patient education, especially for older adults, on the risks of underdialysis and the need for dose escalation [39].
Dry weight is defined as the lowest post-dialysis body weight tolerated without signs of hypovolemia [48]. The high prevalence of cardiovascular disease and autonomic dysfunction indicates that older patients are vulnerable to circulatory stress and volume changes during HD. Inappropriate titration of dry weight can increase the risk of IDH [48,49], which is associated with adverse outcomes, including post-dialysis fatigue, dialysis interruption, RKF decline, multi-organ ischemia, and mortality [50–52]. Recurrent IDH can also lead to cerebral hypoperfusion and worsening cognitive impairment in older patients [53,54]. Common strategies to prevent IDH include limiting IDWG and optimizing the target dry weight [48]. Dietary restriction is a feasible approach for reducing IDWG at the patient level. However, the risk of malnutrition must be carefully considered when treating older patients. Physicians should avoid setting the dry weight excessively low without properly assessing volume status. Instead, careful evaluation of fluid balance and individualized dry weight adjustment are essential, particularly when managing comorbidities in older patients.
HD adequacy is typically assessed based on urea clearance, expressed as Kt/V, which reflects the removal of small solutes. Clinical guidelines recommend a target single-pool (sp) Kt/V greater than 1.4, with a minimum delivered spKt/V of 1.2 [55]. However, age-related changes in body composition should be considered when interpreting Kt/V in older patients. Older adults often have lower muscle mass relative to total body mass than younger people, making their actual fluid volume smaller than the estimated distribution volume and leading to the potential underestimation of Kt/V. Consequently, older patients may receive unnecessarily high dialysis doses, increasing their exposure to HD-related materials and the risk of adverse events without clear clinical benefits [56,57]. A recent Korean study found that achieving a Kt/V greater than 1.4 did not provide additional survival benefits in patients aged ≥ 85 years [58]. In older patients undergoing HD, survival is closely associated with systolic blood pressure, mineral metabolism, nutritional status, and cardiovascular comorbidities [59]. Therefore, the adequacy of HD in older patients should be assessed through a comprehensive evaluation of clinical parameters, in addition to urea clearance.
Middle molecule clearance is another important indicator of HD adequacy. High-flux dialyzers and hemodiafiltration (HDF) provide superior clearance of middle molecules compared to low-flux dialyzers [60]. However, low-flux dialyzers are often preferred in older patients because they can achieve Kt/V targets while minimizing mineral and nutrient loss [61]. The accumulation of middle molecules can lead to adverse clinical outcomes such as dialysis-related amyloidosis and cardiovascular mortality [62,63]. Several studies have demonstrated the clinical advantages of high-flux HD and HDF in older patients. Huang et al. [64] found that high-flux HD had a lower risk of cardiovascular mortality compared with low-flux HD in older patients. A recent RCT showed that high-dose HDF with a convection volume of at least 23 L per session provides a survival benefit over high-flux HD, but only in patients aged ≥ 65 years [65]. Another RCT that included patients aged ≥ 65 years demonstrated that HDF was associated with a lower risk of asymptomatic IDH compared with high-flux HD, although health-related quality of life, morbidity, and mortality were similar between groups [66]. Therefore, when prescribing HD for older patients, nephrologists should prioritize comprehensive clinical benefits beyond laboratory targets for dialysis adequacy. Accordingly, high-flux HD and HDF may be favorable treatment options.
Many centers have adopted incremental PD as an initial PD strategy since its introduction in the 1990s [67,68]. In incremental PD, the initial PD dose is lower than the standard full dose, but achieves target clearance with the support of RKF. Then, the dose is progressively increased as RKF declines [69]. For example, an incremental approach to continuous ambulatory peritoneal dialysis begins with three 1.5-L exchanges per day, with a gradual increase to the standard four 2-L exchanges as RKF declines. In automated peritoneal dialysis (APD) using a cycler, treatment starts with three 1.5- L nighttime exchanges, without daytime dwell. As RKF deteriorates, the dwell volume can be increased or daytime dwell can be added. In addition, PD can be prescribed for fewer than seven days per week by incorporating “PD holidays” during which dialysis is not performed (Table 3).
Incremental PD offers several advantages over standard full-dose PD, including better RKF preservation, reduced glucose exposure, and lower peritonitis risk [70]. Compared with standard PD, incremental PD is associated with superior technique survival, defined as a lower likelihood of transfer from PD to HD because of complications such as peritonitis, catheter dysfunction, or peritoneal membrane failure [71]. The 2020 International Society of Peritoneal Dialysis (ISPD) guidelines recommend modifying PD prescriptions to minimize the treatment burden on frail and older patients [72]. Incremental PD supports this strategy by requiring fewer PD exchanges and shorter dwell times during the early treatment phase. Thus, it enables older patients to gradually adapt to life with PD and offers them greater flexibility in daily life.
The 2020 ISPD guidelines highlight a paradigm shift from traditional adequacy targets based solely on small solute clearance to a goal-directed, person-centered approach to PD [72]. This approach emphasizes a comprehensive assessment that includes not only solute clearance but also laboratory parameters, nutritional status, and health-related quality of life. Therefore, alternative PD strategies, such as decremental PD and low-clearance non-incremental PD, may be appropriate for older patients. Decremental PD gradually reduces the volume and number of exchanges in response to changes in the patient’s clinical condition, taking an approach opposite to that of incremental PD. This strategy may be suitable for older patients who only require relief from uremic symptoms and are not aiming for specific clearance targets due to life expectancy or intractable illnesses. Low-clearance non-incremental PD delivers a lower dose than standard full-dose PD during the early phase. Unlike in incremental PD, the dose is not increased because the initial prescription meets low metabolic demands, particularly in older patients with low muscle mass and poor dietary intake.
Functional dependence has frequently been a barrier to PD eligibility for older patients. Decreased vision, reduced hand coordination, and cognitive dysfunction can interfere with the precise handling of PD equipment, potentially leading to adverse clinical outcomes [73,74]. Assisted PD, which involves support from family members, nurses, or paid caregivers, has allowed many older patients to become eligible for PD [75]. These caregivers assist patients by lifting dialysate bags, connecting and disconnecting them from the cycler, providing exit site care, and performing basic physical assessments [76].
Assisted PD is associated with favorable clinical outcomes in older patients. Advanced age has consistently been identified as a risk factor for peritonitis, likely because of multiple comorbidities and cognitive or functional impairments [22,23,73]. A retrospective analysis of the French PD registry demonstrated that nurse-assisted PD could reduce the risk of peritonitis in patients aged ≥ 75 years [77]. Another study from the same cohort revealed a significant association between nurse-assisted PD and lower risk of transfer to HD due to inadequate dialysis or infection than self-care PD [78]. Compared with patients who performed self-care PD, those receiving nurse-assisted PD were significantly older, with a median age of 80 years, and had a higher comorbidity index [78]. Therefore, assisted PD is an effective strategy to improve PD accessibility for older patients with functional dependence because it supports the proper manipulation of PD equipment and precise implementation of dialysis regimens prescribed by physicians.
Several strategies could promote the wider adoption of assisted PD in older patients. Stepwise and planned dialysis initiation can help start assisted PD in a timely manner, thereby preventing urgent HD via CVC and the subsequent transition to long-term HD [79]. Early identification of assistance needs and selection of assistance in advance during the initial assessment for PD eligibility can help establish PD as a practical and feasible option for older patients. Furthermore, APD or incremental PD strategies can reduce caregiver burden and barriers to PD entry. After PD initiation, regular assessment of changes in barriers to PD and timely adjustments to assistance are essential to sustain assisted PD. Patients may require additional assistance as their functional capacity declines with age or during acute illness. However, some patients regain independence after initiating dialysis and can transition from assisted to self-care PD. The 2024 ISPD position paper emphasizes that assisted PD should be recognized as a standard modality for patients with functional limitations, especially older patients [27]. The position paper further highlights the importance of implementing adaptable service models tailored to local resources, such as nurse-led or family-supported PD. These recommendations aim to enhance access to PD and reduce reliance on hospital-based HD services. Assisted PD programs, which include funding mechanisms and a stable supply of assistance, are provided by national or regional healthcare systems in many European countries [80,81]. However, in Korea, assistance is largely dependent on family members without financial support or systematic supervision, which may lead to difficulties in maintaining assisted PD. Therefore, establishing financial support through reimbursement policies, structured assisted PD programs, and standardized assistant training at the national level will be the key to expanding assisted PD among older patients in Korea.
Geriatric syndrome is a multifaceted clinical condition characterized by physical frailty, malnutrition, multiple comorbidities, and cognitive impairment associated with aging. With the growing number of older patients in this population, the prevalence of geriatric syndrome among patients with ESKD is increasing [82]. Most older patients with ESKD have two or more geriatric impairments that are often interrelated [83]. A comprehensive geriatric assessment should be implemented using a multidisciplinary approach involving nutritionists, physiatrists, psychiatrists, and neurologists to improve clinical outcomes in this population [84]. In this section, we discuss the clinical significance of frailty and nutrition, which are the two key components of geriatric syndrome, and propose strategies to improve outcomes in older patients undergoing dialysis.
Frailty is a state of reduced ability to recover from physical or medical stress, leading to adverse clinical outcomes [85]. It is more prevalent in patients undergoing dialysis than in the general population [86]. A pre-existing uremic environment and metabolic disturbances during the pre-dialysis period activate inflammatory pathways and contribute to the development of sarcopenia [87]. Older patients often continue to experience frailty even after initiating dialysis because of nutritional losses during dialysis and frequent hospitalization related to comorbidities [88,89]. Frailty remains an under-recognized but important risk factor for adverse clinical outcomes in this population, including all-cause mortality and hospitalization [90,91].
Frailty assessments include indicators such as unintentional weight loss, self-reported exhaustion, low physical activity, and poor physical performance (Table 4) [90–96]. These assessments should be integrated into every step of the dialysis planning process for older adults. Frailty is a risk factor for death before dialysis initiation and during the course of dialysis in older patients with advanced CKD. Therefore, CKM may be considered a reasonable alternative to dialysis in patients with significant frailty [97]. When older patients decide to initiate dialysis, frailty assessments can help evaluate their physical function and predict the need for additional support. Individualized strategies should be developed to support dialysis based on the type and severity of functional impairment. For example, caregivers may be required to accompany patients who are unable to transfer themselves to HD centers or to support assisted PD in patients with impaired precise handling of PD or cognitive dysfunction. When establishing VA in older patients who opt for HD, frailty increases the risk of AVF maturation failure in addition to factors such as advanced age and comorbidities [98]. In such cases, CVC or AVG may be considered as VA alternatives.
Physical activity interventions can mitigate frailty, improve muscular strength and cardiovascular function, and reduce hospitalization in patients receiving dialysis [99–101]. The 2017 ERBP Clinical Practice Guidelines recommend structured and individualized exercise programs for older patients with advanced CKD, including those undergoing dialysis [10]. Exercise programs tailored to patients’ functional capacities and personal preferences can provide feasible and safe exercise training for older patients undergoing dialysis. In particular, intradialytic exercise during HD sessions can potentially enhance safety, improve adherence under the supervision of healthcare professionals, and transform sedentary dialysis time into opportunities for health promotion [99]. Similarly, for patients undergoing PD, the 2022 recommendations of the Global Renal Exercise Network and ISPD advocate the incorporation of home-based aerobic and resistance exercises, such as walking, cycling, and resistance band training, into daily routines to help prevent frailty and maintain functional independence [102].
Protein-energy wasting (PEW) refers to a form of malnutrition in patients with CKD characterized by an imbalance in protein metabolism, in which catabolism exceeds anabolism, leading to reduced nutritional biomarkers, body mass, and muscle mass [103,104]. The high prevalence of PEW in older patients undergoing dialysis may be attributable to nutritional loss during dialysis, chronic inflammation, inadequate dietary intake associated with aging, and multiple comorbidities [105,106].
Laboratory parameters, dietary records, and body composition measurements can be used to assess the nutritional status of older patients undergoing dialysis [105]. However, changes in body composition in this population present a significant challenge for the accurate assessments of nutritional status. Dilution caused by volume overload can affect nutritional biochemical parameters, such as serum albumin and prealbumin levels. In patients receiving PD, aging and chronic exposure to peritoneal dialysate glucose contribute to an increased proportion of body fat and reduced muscle mass as part of overall body composition. Anthropometric parameters, such as calf circumference, skinfold thickness, and waist circumference, may provide more accurate nutritional assessments than body mass index or total body weight because they better reflect muscle and fat mass. Composite nutritional indices that incorporate both subjective and objective aspects, such as Subjective Global Assessment and Malnutrition Inflammation Scores, can provide a comprehensive approach for evaluating nutritional status [107,108]. Furthermore, body composition analysis using technical devices such as bioelectrical impedance analysis or dual-energy X-ray absorptiometry may support more objective and quantitative assessments of patients undergoing dialysis [107].
Adequate dietary intake is essential for protein synthesis and regarded as a key nutritional intervention. The 2020 KDOQI guidelines for nutrition in CKD recommend 1.0–1.2 g/kg/day of protein and 25–35 kcal/kg/day of energy intake for patients undergoing dialysis, considering increased nutritional loss and catabolism associated with dialysis [107]. When these targets cannot be achieved through dietary intake alone, nutritional supplementation, such as oral, enteral, or intradialytic parenteral nutrition, should be considered [109]. A protein-rich diet contains high phosphate levels, which are associated with increased vascular calcification and mortality risks in patients undergoing dialysis [110]. However, strict phosphorus restrictions can increase the risk of malnutrition, which is particularly detrimental in older patients. Therefore, adequate protein intake combined with phosphate binders can be a practical strategy for maintaining nutritional status while controlling phosphorus levels [111].
Several age-related factors, such as cognitive dysfunction, depression, social deprivation, and functional disorders of the gastrointestinal tract, contribute to suboptimal dietary intake in older patients undergoing dialysis. Psychological and social support should be integrated into a multidisciplinary approach to enhance the effectiveness of dietary interventions. Physicians should perform comprehensive assessments and implement multifaceted strategies to improve the nutritional status of this population.
In older patients with advanced CKD, the aging process substantially affects clinical outcomes throughout the trajectory of dialysis from initiation to long-term maintenance. Age-related factors should be carefully considered when determining the timing of dialysis initiation, selecting an appropriate modality, and adjusting dialysis prescriptions. Dialysis management in older patients must evolve toward a more individualized approach, with treatment decisions guided by patient-centered goals, such as quality of life and functional preservation, rather than focusing only on biochemical treatment targets. A multidisciplinary approach and regular reassessments are essential for providing appropriate care to this vulnerable population.
SDM involving nephrologists, other healthcare professionals, patients, and caregivers should be integrated throughout the course of dialysis for older patients with ESKD. In addition, developing clinical guidelines tailored to older adults undergoing dialysis, expanding access to home-based dialysis and conservative care options, and investing in assisted dialysis infrastructure could help provide more effective and individualized care. Future research should establish standardized strategies that incorporate geriatric assessments to ensure high-quality personalized dialysis in the growing older adult population.
Notes
Acknowledgments
The authors would like to thank the Korean Society of Geriatric Nephrology for its valuable support and ongoing contribution to the advancement of research in geriatric nephrology.
Figure 1
Decision to initiate kidney replacement therapy in older patients with advanced CKD based on the 2017 ERBP guidelines. CKD, chronic kidney disease; KFRE, Kidney Failure Risk Equation; REIN, Renal Epidemiology and Information Network; ERBP, European Renal Best Practice.
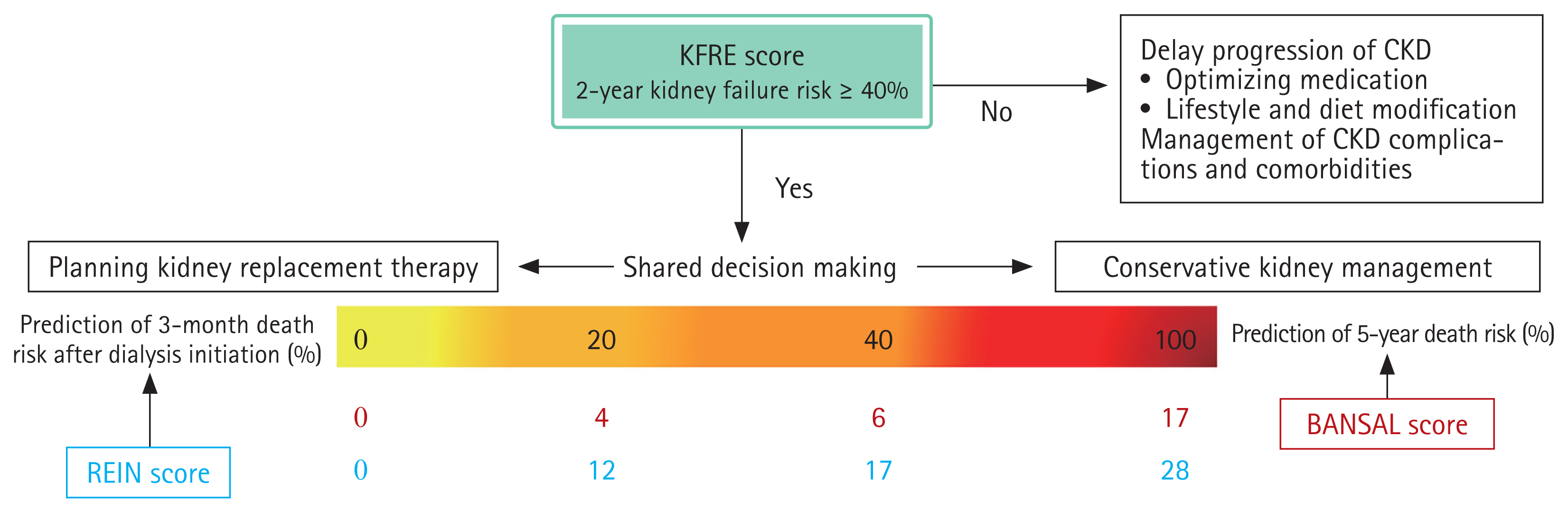
Figure 2
Schematic representation of the incremental HD approach with twice-weekly HD initiation. The diagram outlines a stepwise approach for initiating patients on a twice-weekly HD schedule. Patients begin with two sessions per week and ongoing monitoring of RKF, urine output, and clinical status. As RKF declines or clinical indications occur (e.g., volume overload, hyperphosphatemia, and hyperkalemia), HD frequency is gradually increased to three times per week. This approach also includes decremental palliative hemodialysis for patients with limited life expectancy, focusing on symptom relief and quality of life rather than achieving conventional dialysis adequacy targets. eGFR, estimated glomerular filtration rate; HD, hemodialysis; RKF, residual kidney function.
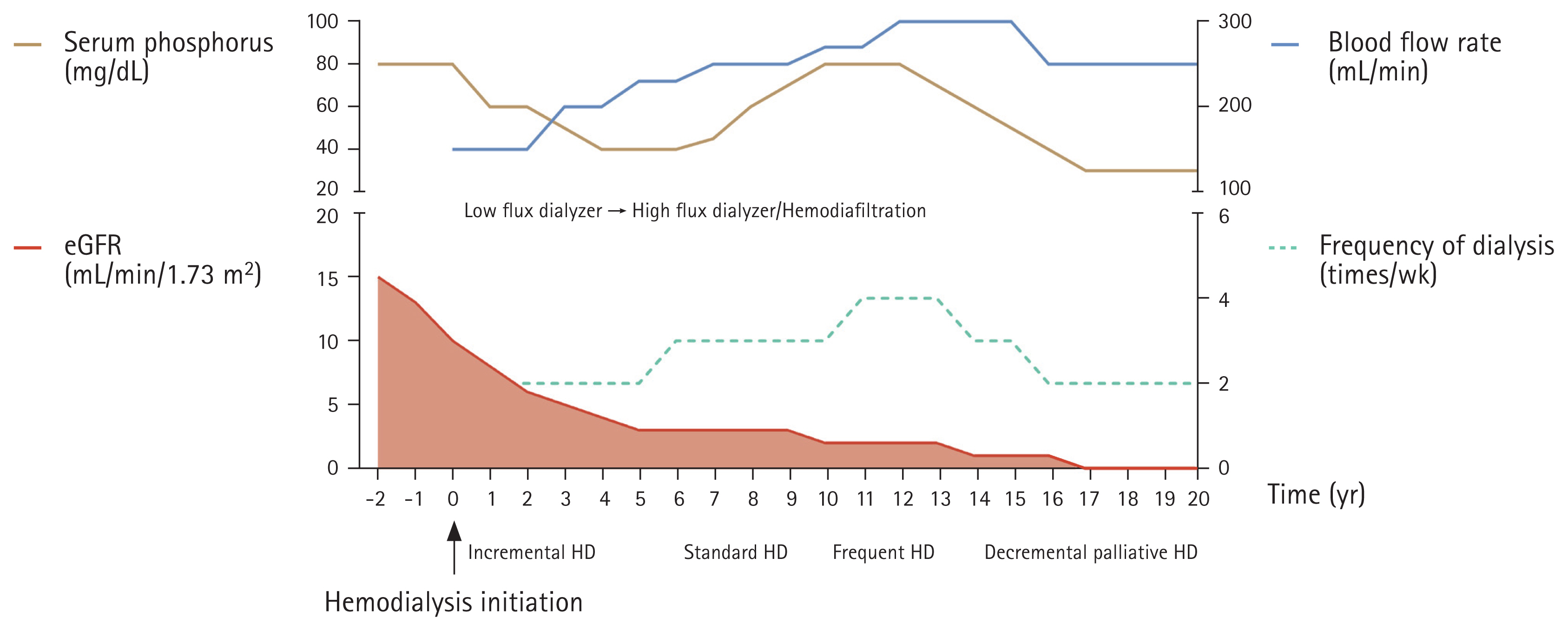
Table 1
Clinical indications for long-term use of tunneled central venous catheters in older patients based on the 2019 KDOQI guidelines
Table 2
Overview of completed and ongoing randomized controlled trials comparing incremental and conventional HD
| Study | Country | Target sample | Study participants | Follow-up duration | Residual kidney function eligibility/Actual residual kidney function | Outcome | Results |
|---|---|---|---|---|---|---|---|
| PRIDE [42] | Republic of Korea | 428 |
Twice-weekly HD vs. Thrive-weekly HD Age ≥ 60 yr |
24 mo | UO ≥ 500 mL/day |
Primary outcome: all-cause hospitalization Secondary outcome: dialysis-related hospitalization rate, length of hospital day, mortality rate, and quality of life |
In progress |
| TWOPLUS [40] | United States | 50 |
Twice-weekly HD for 6 wk followed by thrice-weekly at week 7 (n = 23) vs. Thrice-weekly HD (n = 25) Mean age: 61.3 ± 14.0 |
12 mo |
KrU ≥ 5 mL/min/1.73 m2 Urine output ≥ 500 mL/day /24-h urine volume (mL/day): Twice-weekly HD group: 914 ± 522 Thrice-weekly HD: 1,424 ± 955 |
Primary outcome: feasibility Secondary outcome: RKF (24-h urine volume, urea clearance, creatinine clearance), total urea clearance, and volume status |
Incremental HD group vs. conventional HD group Percentage change in urine volume from baseline to week 24: +22.8 vs. −28.2 (estimated difference of 51.0 (−0.7 to 102.8) Percentage change in average renal urea and creatinine clearance from baseline to week 24: +12.4 vs. −45.5 |
| Impact of incremental versus conventional initiation of hemodialysis on residual kidney function [41] | United Kindom | 54 |
Twice-weekly HD for 3.5–4 h (n = 29) vs. Thrive-weekly HD for 3.5–4 h (n = 26) Mean age: Incremental HD: 61.4 ± 15.2 vs. Standard HD: 63.1 ± 12.3 |
12 mo |
KrU ≥ 3 mL/min/1.73 m2/Twice-weekly HD group: 4.41 (4.00–5.69) Thrice-weekly HD group: 4.21 (3.65–5.17) |
Primary outcome: feasibility, change in RKF (BSA-corrected GFR slope), and hospitalization rate related to dialysis complications Secondary outcome: frailty, quality of life, cognitive function, and biochemistry |
Incremental HD group vs. conventional HD group Hospitalization events: IRR 0.31 (0.17–0.59, p < 0.001) Change in RKF (mL/min/1.73 m2): −0.32 ± 0.38 vs. −0.08 ± 0.51 (p = 0.07) |
| IHDIP [43] | Spain | 152 | Once a week HD vs. Thrive-weekly HD | 24 mo | KrU ≥ 4 mL/min/1.73 m2 |
Primary outcome: survival Secondary outcome: hospitalization rate, RKF preservation, HD adequacy, biochemistry, and quality of life |
In progress |
| REAL LIFE [44] | Italy and Poland | 116 | Once-weekly HD vs. Thrive-weekly HD | 24 mo |
KrU between 5 and 10 mL/min/1.73 m2 UO ≥ 600 mL/day |
Primary outcome: loss of RKF, defined as UO ≤ 200 mL/day Secondary outcome: survival, biochemistry, and composite cardiovascular events |
In progress |
| Initiating renal replacement therapy through incremental hemodialysis [45] | Spain | 88 | Twice-weekly HD vs. Thrive-weekly HD | 12 mo | KrU ≥ 2.5 mL/min/1.73 m2 |
Primary outcome: loss of RKF, defined as UO < 100 mL/day Secondary outcome: mortality, hospitalization rate, biochemistry, HD adequacy, and quality of life |
In progress |
| INCH-HD [46] | Australia and Canada | 372 | Twice-weekly HD vs. Thrive-weekly HD | 18 mo | UO ≥ 500 mL/day |
Primary outcome: health-related quality of life (KDQOL-SF) Secondary outcome: RKF, mortality, MACE, and hospitalization rate |
In progress |
| INCHVETS [47] | United States | 252 | Twice-weekly HD vs. Thrive-weekly HD | 12 mo | UO ≥ 500 mL/day and KrU >3 mL/min |
Primary outcome: health-related quality of life (SF-36) Secondary outcome: RKF, HD adequacy, and dialysis symptoms |
In progress |
Table 3
Typical incremental PD prescription strategies in CAPD and APD
| Initial PD prescription | Incrementation | Increased PD prescription |
|---|---|---|
| CAPD | ||
| 1.5 L × 4 exchanges | Increase dwell volumes 2 | L × 4 exchangesa) |
| 2 L × 2–3 exchanges only during daytime | Increase the number of exchanges and add night dwell | 2 L × 4 exchangesa) |
| 1 × 2 L icodextrin long dwell during night | Add daytime dwell | 2 L × 2–3 exchanges during daytime + 2 L icodextrin long dwell during night |
| 4 × 2 L exchanges only on weekdays | Increase frequency | Every day for a weeka) |
| APD | ||
| 3 × 1.5 L cycled over 6 h during night | Increase dwell volumes | 2 L × 3 cycled over 6 h during night |
| 3 × 2 L cycled over 6 h during night | Increase number of exchanges | 2 L × 4 cycled over 8 h during night |
| 4 × 2 L cycled over 8 h during night | Add daytime dwell | 2 L × 4 cycled over 8 h during night + 2 L icodextrin long dwell during daytimea) |
| 4 × 2 L cycled every other day | Increase frequency | Every day for a weeka) |
Table 4
Commonly used tool to assess frailty in older adults
| Tool | Domain | Classification | Strength | Limitation | Association with clinical outcomes in older patients with ESKD |
|---|---|---|---|---|---|
| Fried frailty phenotype | Weight loss, exhaustion, physical activity, weakness, and slowness |
Robust: 0 Pre-frail: 1–2 Frail: 3–5 |
Comprehensive assessment of observed performance and self-reported physical function | Measurements, such as grip strength and walking test, are not easy to execute in routine practice, Lack of co-morbidities and psychosocial components |
Mortality [90,92–94] Hospitalization [93,94], Emergency visits [93] |
| Frailty index | 38 frailty components (comorbidities, disabilities, physical function, and self-reported health, etc.) |
Total score of deficits /Total available items: Robust: ≤ 0.08 Pre-frail: 0.09–0.24 Frail: ≥ 0.25 |
Multidimensional assessment of frailty, including psychosocial aspects, cognitive function, and co-morbidities | Timing-consuming and complex to implement in routine clinical care | Mortality and Hospitalization [95] |
| Short physical performance battery | Usual gait speed, repeated standing up from the chair, and standing balance |
Worst performance = 0 Best performance = 12 Frailty: ≤ 9 |
Rapid and objective assessment, Test-retest reliability, clinical applicability | Lack of evaluation of aerobic capacity and psychosocial factor, such as self-efficacy | Mortality and Hospitalization [96] |
| FRAIL scale | Five items of self-report questionnaire: Fatigue, Resistance, Ambulation, Illness, and Loss of weight |
Robust: 0 Pre-frail: 1–2 Frail: ≥ 3 |
Simple and rapid assessment | Lack of objective assessment | N/A |
| Clinical frailty scale | Nine descriptors of composite levels of mobility, energy, physical activity, and function |
Very fit = 1 Terminally ill = 9 Frail: ≥ 5 |
Reflection of overall competency in daily life activities, Easy applicability in routine clinical practice | Subjective clinical judgement by the healthcare provider could lead to misclassification | Mortality [97] |
| Groningen frailty indicator | 15 items of self-reported disabilities in four domains (physical, cognitive, social, and psychological) | Frail: ≥ 4 | Short questionnaire and good feasibility, Usefulness as a frailty screening tool | Lack of objective assessment | Mortality and Hospitalization [91] |
REFERENCES
1. Huijben JA, Kramer A, Kerschbaum J, et al. Increasing numbers and improved overall survival of patients on kidney replacement therapy over the last decade in Europe: an ERA Registry study. Nephrol Dial Transplant 2023;38:1027–1040.



2. Hanafusa N, Abe M, Joki N, et al. Annual dialysis data report 2021, Japanese Society for Dialysis Therapy (JSDT) renal data registry. Ren Replace Ther 2024;10:78.
3. Hong YA, Ban TH, Kang CY, et al. Trends in epidemiologic characteristics of end-stage renal disease from 2019 Korean Renal Data System (KORDS). Kidney Res Clin Pract 2021;40:52–61.




4. Kim H, Jeong SA, Kim KM, et al. Trends in clinical outcomes of older hemodialysis patients: data from the 2023 Korean Renal Data System (KORDS). Kidney Res Clin Pract 2024;43:263–273.




5. Beard JR, Officer A, de Carvalho IA, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet 2016;387:2145–2154.


6. van Loon IN, Goto NA, Boereboom FTJ, Verhaar MC, Bots ML, Hamaker ME. Quality of life after the initiation of dialysis or maximal conservative management in elderly patients: a longitudinal analysis of the Geriatric assessment in OLder patients starting Dialysis (GOLD) study. BMC Nephrol 2019;20:108.


7. Verberne WR, Geers AB, Jellema WT, Vincent HH, van Delden JJ, Bos WJ. Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol 2016;11:633–640.



8. Robinson BM, Zhang J, Morgenstern H, et al. Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney Int 2014;85:158–165.


9. Hamroun A, Speyer E, Ayav C, et al.; CKD-REIN study Collaborators. Barriers to conservative care from patients’ and nephrologists’ perspectives: the CKD-REIN study. Nephrol Dial Transplant 2022;37:2438–2448.



10. Farrington K, Covic A, Nistor I, et al. Clinical Practice Guideline on management of older patients with chronic kidney disease stage 3b or higher (eGFR<45 mL/min/1.73 m2): a summary document from the European Renal Best Practice Group. Nephrol Dial Transplant 2017;32:9–16.


11. Bansal N, Katz R, De Boer IH, et al. Development and validation of a model to predict 5-year risk of death without ESRD among older adults with CKD. Clin J Am Soc Nephrol 2015;10:363–371.



12. Tangri N, Stevens LA, Griffith J, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 2011;305:1553–1559.


13. Couchoud CG, Beuscart JB, Aldigier JC, Brunet PJ, Moranne OP, REIN registry. Development of a risk stratification algorithm to improve patient-centered care and decision making for incident elderly patients with end-stage renal disease. Kidney Int 2015;88:1178–1186.


14. Park WY, Bae E, Lee HS, et al. Prediction model for 6-month mortality in incident older hemodialysis patients in South Korea. Kidney Res Clin Pract 2025;44:664–678.




15. Hong YA, Chung S, Park WY, et al.; Committee on Ethical Issues of the Korean Society of Nephrology. Nephrologists’ perspectives on decision making about life-sustaining treatment and palliative care at end of life: a questionnaire survey in Korea. J Palliat Med 2021;24:527–535.


16. Zhang R, Pu C, Cui X, Zhang N, Li X, Zheng F. Burden in primary family caregivers caring for uremic patients on maintenance peritoneal dialysis. Perit Dial Int 2020;40:556–562.



17. Guerville F, Pépin M, Garnier-Crussard A, et al. How to make a shared decision with older persons for end-stage kidney disease treatment: the added value of geronto-nephrology. Clin Kidney J 2024;17:sfae281.




18. Magadi W, Birnie K, Santhakumaran S, Caskey FJ, Ben-Shlomo Y. An updated systematic review of the risk factors for unplanned dialysis initiation. Clin Kidney J 2024;17:sfae333.




19. Alizada U, Sauleau EA, Krummel T, et al.; the REIN registry. Effect of emergency start and central venous catheter on outcomes in incident hemodialysis patients: a prospective observational cohort. J Nephrol 2022;35:977–988.



20. Kanno A, Nakayama M, Sanada S, Sato M, Sato T, Taguma Y. Suboptimal initiation predicts short-term prognosis and vulnerability among very elderly patients who start haemodialysis. Nephrology (Carlton) 2019;24:94–101.



21. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 2024;105:S117–S314.


22. Gadola L, Poggi C, Dominguez P, Poggio MV, Lungo E, Cardozo C. Risk factors and prevention of peritoneal dialysis-related peritonitis. Perit Dial Int 2019;39:119–125.



23. Wu H, Ye H, Huang R, et al. Incidence and risk factors of peritoneal dialysis-related peritonitis in elderly patients: a retrospective clinical study. Perit Dial Int 2020;40:26–33.



24. Kim HJ, Park JT, Han SH, et al. The pattern of choosing dialysis modality and related mortality outcomes in Korea: a national population-based study. Korean J Intern Med 2017;32:699–710.




25. Cheng L, Hu N, Song D, Chen Y. Mortality of peritoneal dialysis versus hemodialysis in older adults: an updated systematic review and meta-analysis. Gerontology 2024;70:461–478.



26. Lee SW, Lee NR, Son SK, et al. Comparative study of peritoneal dialysis versus hemodialysis on the clinical outcomes in Korea: a population-based approach. Sci Rep 2019;9:5905.




27. Oliver MJ, Abra G, Béchade C, et al. Assisted peritoneal dialysis: position paper for the ISPD. Perit Dial Int 2024;44:160–170.



28. Lee T, Thamer M, Zhang Q, Zhang Y, Allon M. Vascular access type and clinical outcomes among elderly patients on hemodialysis. Clin J Am Soc Nephrol 2017;12:1823–1830.



29. Lee HS, Song YR, Kim JK, et al. Outcomes of vascular access in hemodialysis patients: analysis based on the Korean National Health Insurance Database from 2008 to 2016. Kidney Res Clin Pract 2019;38:391–398.



30. Lok CE, Huber TS, Lee T, et al.; National Kidney Foundation. KDOQI clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis 2020;75:S1–S164.


31. Harms JC, Rangarajan S, Young CJ, Barker-Finkel J, Allon M. Outcomes of arteriovenous fistulas and grafts with or without intervention before successful use. J Vasc Surg 2016;64:155–162.


32. Yoshida M, Doi S, Nakashima A, et al. Different risk factors are associated with vascular access patency after construction and percutaneous transluminal angioplasty in patients starting hemodialysis. J Vasc Access 2021;22:707–715.



33. DeSilva RN, Patibandla BK, Vin Y, et al. Fistula first is not always the best strategy for the elderly. J Am Soc Nephrol 2013;24:1297–1304.



34. Lyu B, Chan MR, Yevzlin AS, Astor BC. Catheter dependence after arteriovenous fistula or graft placement among elderly patients on hemodialysis. Am J Kidney Dis 2021;78:399–408e1.


35. Drew DA, Lok CE, Cohen JT, Wagner M, Tangri N, Weiner DE. Vascular access choice in incident hemodialysis patients: a decision analysis. J Am Soc Nephrol 2015;26:183–191.

36. Kim HY, Bae EH, Ma SK, Kim SW. Association between initial vascular access and survival in hemodialysis according to age. Korean J Intern Med 2019;34:867–876.



37. van Oevelen M, Heggen BD, Abrahams AC, et al. Central venous catheter-related complications in older haemodialysis patients: a multicentre observational cohort study. J Vasc Access 2023;24:1322–1331.



38. Wong J, Vilar E, Davenport A, Farrington K. Incremental haemodialysis. Nephrol Dial Transplant 2015;30:1639–1648.


39. Canaud B, Stuard S, Laukhuf F, et al. Choices in hemodialysis therapies: variants, personalized therapy and application of evidence-based medicine. Clin Kidney J 2021;14:i45–i58.




40. Murea M, Patel A, Highland BR, et al. Twice-weekly hemodialysis with adjuvant pharmacotherapy and transition to thrice-weekly hemodialysis: a pilot study. Am J Kidney Dis 2022;80:227–240e1.


41. Vilar E, Kaja Kamal RM, Fotheringham J, et al. A multicenter feasibility randomized controlled trial to assess the impact of incremental versus conventional initiation of hemodialysis on residual kidney function. Kidney Int 2022;101:615–625.


42. Han M, Jeon H, Yu BC, et al.; PRIDE Research Group. A pragmatic randomized clinical trial: twice-weekly vs. thrice-weekly Incident hemoDialysis in Elderly patients (PRIDE): study protocol. Kidney Res Clin Pract 2023;Dec. 18. [Epub]. 10.23876/j.krcp.23.177.

43. Deira J, Suárez MA, López F, et al. IHDIP: a controlled randomized trial to assess the security and effectiveness of the incremental hemodialysis in incident patients. BMC Nephrol 2019;20:8.




44. Casino FG, Basile C, Kirmizis D, et al.; Eudial Working Group of ERA-EDTA. The reasons for a clinical trial on incremental haemodialysis. Nephrol Dial Transplant 2020;35:2015–2019.



45. Fernández Lucas M, Ruíz-Roso G, Merino JL, et al. Initiating renal replacement therapy through incremental haemodialysis: protocol for a randomized multicentre clinical trial. Trials 2020;21:206.


46. INCremental Dialysis to Improve Health Outcomes in People Starting Haemodialysis (INCH-HD) [Internet] Brisbane: The University of Queensland, c2024. [cited 2024 April 16]. Available from: https://ctv.veeva.com/study/incremental-dialysis-to-improve-health-outcomes-in-people-starting-haemo-dialysis-inch-hd.
47. Incremental Hemodialysis for Veterans in the First Year of Dialysis (IncHVets) (INCHVETS) [Internet] Washington, D.C: VA Office of Research and Development, c2025. [cited 2025 June 3]. Available from: https://classic.clinicaltrials.gov/ct2/show/NCT05465044.
48. Kanbay M, Ertuglu LA, Afsar B, et al. An update review of intradialytic hypotension: concept, risk factors, clinical implications and management. Clin Kidney J 2020;13:981–993.




49. Gul A, Miskulin D, Harford A, Zager P. Intradialytic hypotension. Curr Opin Nephrol Hypertens 2016;25:545–550.


50. Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT, NECOSAD Study Group. Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int 2002;62:1046–1053.


51. McIntyre CW. Update on hemodialysis-induced multiorgan ischemia: brains and beyond. J Am Soc Nephrol 2024;35:653–664.


52. Chou JA, Streja E, Nguyen DV, et al. Intradialytic hypotension, blood pressure changes and mortality risk in incident hemodialysis patients. Nephrol Dial Transplant 2018;33:149–159.


53. Polinder-Bos HA, García DV, Kuipers J, et al. Hemodialysis induces an acute decline in cerebral blood flow in elderly patients. J Am Soc Nephrol 2018;29:1317–1325.



54. Assimon MM, Wang L, Flythe JE. Cumulative exposure to frequent intradialytic hypotension associates with new-onset dementia among elderly hemodialysis patients. Kidney Int Rep 2019;4:603–606.



55. National Kidney Foundation. KDOQI clinical practice guideline for hemodialysis adequacy: 2015 update. Am J Kidney Dis 2015;66:884–930.

56. Tattersall J, Farrington K, Gentile G, et al.; European Renal Best Practice Guidelines Group and the European Union of Geriatric Medicine Societies (EUGMS) collaborative group for the production of guidelines on the management of older patients with CKD. Is Kt/V useful in elderly dialysis patients? Pro and Con arguments. Nephrol Dial Transplant 2018;33:742–750.


57. Spalding EM, Chandna SM, Davenport A, Farrington K. Kt/V underestimates the hemodialysis dose in women and small men. Kidney Int 2008;74:348–355.


58. Jeon J, Kim GO, Kim BY, et al. Effects of Kt/V
urea on outcomes according to age in patients on maintenance hemodialysis. Clin Kidney J 2024;17:sfae116.


59. Villain C, Ecochard R, Bouchet JL, et al. Relative prognostic impact of nutrition, anaemia, bone metabolism and cardiovascular comorbidities in elderly haemodialysis patients. Nephrol Dial Transplant 2019;34:848–858.


60. Jung JY, Yoo KD, Kang E, et al.; Clinical Practice Guideline Work Group. Executive summary of the Korean Society of Nephrology 2021 clinical practice guideline for optimal hemodialysis treatment. Korean J Intern Med 2022;37:701–718.




61. Cheung AK, Levin NW, Greene T, et al. Effects of high-flux hemodialysis on clinical outcomes: results of the HEMO study. J Am Soc Nephrol 2003;14:3251–3263.

62. Kaneko S, Yamagata K. Hemodialysis-related amyloidosis: is it still relevant? Semin Dial 2018;31:612–618.



63. Liabeuf S, Lenglet A, Desjardins L, et al.; European Uremic Toxin Work Group (EUTox). Plasma beta-2 microglobulin is associated with cardiovascular disease in uremic patients. Kidney Int 2012;82:1297–1303.


64. Huang W, Bai J, Zhang Y, et al. Effects of low-flux and high-flux hemodialysis on the survival of elderly maintenance hemodialysis patients. Ren Fail 2024;46:2338217.



65. Blankestijn PJ, Vernooij RWM, Hockham C, et al.; CONVINCE Scientific Committee Investigators. Effect of hemodiafiltration or hemodialysis on mortality in kidney failure. N Engl J Med 2023;389:700–709.


66. Morena M, Jaussent A, Chalabi L, et al.; FRENCHIE Study Investigators. Treatment tolerance and patient-reported outcomes favor online hemodiafiltration compared to high-flux hemodialysis in the elderly. Kidney Int 2017;91:1495–1509.

67. Ankawi GA, Woodcock NI, Jain AK, Garg AX, Blake PG. The use of incremental peritoneal dialysis in a large contemporary peritoneal dialysis program. Can J Kidney Health Dis 2016;3:2054358116679131.




68. Yan H, Abreu Z, Bargman JM. Incremental peritoneal dialysis in incident end-stage kidney disease patients. Perit Dial Int 2022;42:387–393.



70. Yan H, Fang W, Lin A, Cao L, Ni Z, Qian J. Three versus 4 daily exchanges and residual kidney function decline in incident CAPD patients: a randomized controlled trial. Am J Kidney Dis 2017;69:506–513.

71. Navaratnarajah A, Clemenger M, McGrory J, et al. Flexibility in peritoneal dialysis prescription: impact on technique survival. Perit Dial Int 2021;41:49–56.



72. Brown EA, Blake PG, Boudville N, et al. International Society for Peritoneal Dialysis practice recommendations: prescribing high-quality goal-directed peritoneal dialysis. Perit Dial Int 2020;40:244–253.


73. Liao JL, Zhang YH, Xiong ZB, et al. The association of cognitive impairment with peritoneal dialysis-related peritonitis. Perit Dial Int 2019;39:229–235.



74. Brar R, Whitlock R, Komenda P, et al. The impact of frailty on technique failure and mortality in patients on home dialysis. Perit Dial Int 2019;39:532–538.


75. Oliver MJ, Quinn RR, Richardson EP, Kiss AJ, Lamping DL, Manns BJ. Home care assistance and the utilization of peritoneal dialysis. Kidney Int 2007;71:673–678.


76. Reyskens M, Abrahams AC, François K, van Eck van der Sluijs A. Assisted peritoneal dialysis in Europe: a strategy to increase and maintain home dialysis. Clin Kidney J 2024;17:i34–i43.




77. Duquennoy S, Béchade C, Verger C, Ficheux M, Ryckelynck JP, Lobbedez T. Is peritonitis risk increased in elderly patients on peritoneal dialysis? Report from the French Language Peritoneal Dialysis Registry (RDPLF). Perit Dial Int 2016;36:291–296.




78. Lanot A, Bechade C, Boyer A, Ficheux M, Lobbedez T. Assisted peritoneal dialysis and transfer to haemodialysis: a cause-specific analysis with data from the RDPLF. Nephrol Dial Transplant 2021;36:330–339.



79. Oliver MJ, Quinn RR. Selecting peritoneal dialysis in the older dialysis population. Perit Dial Int 2015;35:618–621.




80. van Eck van der Sluijs A, van Jaarsveld BC, Allen J, et al. Assisted peritoneal dialysis across Europe: practice variation and factors associated with availability. Perit Dial Int 2021;41:533–541.



81. Giuliani A, Karopadi AN, Prieto-Velasco M, Manani SM, Crepaldi C, Ronco C. Worldwide experiences with assisted peritoneal dialysis. Perit Dial Int 2017;37:503–508.



82. Goto NA, van Loon IN, Morpey MI, et al. Geriatric assessment in elderly patients with end-stage kidney disease. Nephron 2019;141:41–48.



83. Nixon AC, Bampouras TM, Pendleton N, Woywodt A, Mitra S, Dhaygude A. Frailty and chronic kidney disease: current evidence and continuing uncertainties. Clin Kidney J 2018;11:236–245.


84. Brown EA, Farrington K. Geriatric assessment in advanced kidney disease. Clin J Am Soc Nephrol 2019;14:1091–1093.



85. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752–762.



86. Zhao Y, Liu Q, Ji J. The prevalence of frailty in patients on hemodialysis: a systematic review and meta-analysis. Int Urol Nephrol 2020;52:115–120.



87. Reese PP, Cappola AR, Shults J, et al.; CRIC Study Investigators. Physical performance and frailty in chronic kidney disease. Am J Nephrol 2013;38:307–315.



88. Johansen KL, Dalrymple LS, Delgado C, et al. Factors associated with frailty and its trajectory among patients on hemodialysis. Clin J Am Soc Nephrol 2017;12:1100–1108.



89. Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 2009;361:1539–1547.



90. López-Montes A, Martínez-Villaescusa M, Pérez-Rodríguez A, et al. Frailty, physical function and affective status in elderly patients on hemodialysis. Arch Gerontol Geriatr 2020;87:103976.


91. Meulendijks FG, Hamaker ME, Boereboom FT, Kalf A, Vögtlander NP, van Munster BC. Groningen frailty indicator in older patients with end-stage renal disease. Ren Fail 2015;37:1419–1424.


92. Guo Y, Tian R, Ye P, Luo Y. Frailty in older patients undergoing hemodialysis and its association with all-cause mortality: a prospective cohort study. Clin Interv Aging 2022;17:265–275.




93. Li Y, Zhang D, Ma Q, Diao Z, Liu S, Shi X. The impact of frailty on prognosis in elderly hemodialysis patients: a prospective cohort study. Clin Interv Aging 2021;16:1659–1667.




94. van Loon IN, Goto NA, Boereboom FTJ, et al. Geriatric assessment and the relation with mortality and hospitalizations in older patients starting dialysis. Nephron 2019;143:108–119.



95. Soldati A, Poggi MM, Azzolino D, Vettoretti S, Cesari M. Frailty index and adverse outcomes in older patients in haemodialysis. Arch Gerontol Geriatr 2022;101:104673.


96. Uchida J, Suzuki Y, Imamura K, et al. The association of short physical performance battery with mortality and hospitalization in patients receiving hemodialysis. J Ren Nutr 2024;34:235–242.


97. Pugh J, Aggett J, Goodland A, et al. Frailty and comorbidity are independent predictors of outcome in patients referred for pre-dialysis education. Clin Kidney J 2016;9:324–329.



98. Yan T, Gameiro J, Grilo J, Filipe R, Rocha E. Hemodialysis vascular access in elderly patients: a comprehensive review. J Vasc Access 2024;25:27–39.



99. Kim S, Park HJ, Yang DH. An intradialytic aerobic exercise program ameliorates frailty and improves dialysis adequacy and quality of life among hemodialysis patients: a randomized controlled trial. Kidney Res Clin Pract 2022;41:462–472.




100. Deligiannis A, D’Alessandro C, Cupisti A. Exercise training in dialysis patients: impact on cardiovascular and skeletal muscle health. Clin Kidney J 2021;14:ii25–ii33.




101. Mallamaci F, D’Arrigo G, Tripepi G, et al. Long-term effect of physical exercise on the risk for hospitalization and death in dialysis patients: a post-trial long-term observational study. Clin J Am Soc Nephrol 2022;17:1176–1182.


102. Bennett PN, Bohm C, Harasemiw O, et al. Physical activity and exercise in peritoneal dialysis: International Society for Peritoneal Dialysis and the Global Renal Exercise Network practice recommendations. Perit Dial Int 2022;42:8–24.



103. Leal-Escobar G, Biruete A, Cano-Escobar KB, Madero M, Osuna-Padilla IA. Comparison between global leadership initiative on malnutrition criteria and protein-energy wasting in patients with kidney failure undergoing peritoneal dialysis. J Ren Nutr 2025;S1051-2276(25)00015-9.

104. Kim SM, Jung JY. Nutritional management in patients with chronic kidney disease. Korean J Intern Med 2020;35:1279–1290.




105. Rodrigues J, Cuppari L, Campbell KL, Avesani CM. Nutritional assessment of elderly patients on dialysis: pitfalls and potentials for practice. Nephrol Dial Transplant 2017;32:1780–1789.


106. Çelik G, Oc B, Kara I, Yılmaz M, Yuceaktas A, Apiliogullari S. Comparison of nutritional parameters among adult and elderly hemodialysis patients. Int J Med Sci 2011;8:628–634.



107. Ikizler TA, Burrowes JD, Byham-Gray LD, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis 2020;76:S1–S107.


108. González-Ortiz AJ, Arce-Santander CV, Vega-Vega O, Correa-Rotter R, de Espinosa-Cuevas ML. Assessment of the reliability and consistency of the “malnutrition inflammation score” (MIS) in Mexican adults with chronic kidney disease for diagnosis of protein-energy wasting syndrome (PEW). Nutr Hosp 2014;31:1352–1358.

109. Marsen TA, Beer J, Mann H, German IDPN-Trial group. Intradialytic parenteral nutrition in maintenance hemodialysis patients suffering from protein-energy wasting. Results of a multicenter, open, prospective, randomized trial. Clin Nutr 2017;36:107–117.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 344 View
- 129 Download
- Related articles
-
Comprehensive approaches to diabetes in the elderly: adapting to evolving trends2025 November;40(6)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print


