INTRODUCTION
Patients who are admitted to hospitals with acute heart failure (HF) have a grim prognosis, and they show a very high event rate within up to six months after discharge. According to data from the Korean Acute HF Registry (KorAHF), the mortality rate for acute HF during hospitalization is approximately 6%, while the mortality rate for acute HF within one year after discharge is reported to be around 18% [
1]. Guideline-directed medical therapy (GDMT), which consists of renin-angiotensin system inhibitors (RASI) including angiotensin receptor/neprilysin inhibitor, beta-blockers, mineralocorticoid receptor antagonists (MRAs), and the recently added sodium-glucose cotransporter-2 inhibitors (SGLT2i), has been reported to improve the treatment outcomes of HF patients [
2ŌĆō
5].
Despite its proven benefits, the implementation of GDMT in real-world practice remains unsatisfactory [
6]. In the Asia-Pacific regions, including Korea, the GDMT prescription rate upon discharge has only been reported to be around 50% [
7]. There are several factors that contribute to the suboptimal application of GDMT in HF patients. Patient non-adherence and intolerance to medications, which occur due to side effects or fragile patient condition, including low blood pressure and marginal renal function, hinder optimal GDMT application. However, physician inertia also represents a significant obstacle to optimal GDMT application. The reluctance or hesitance among physicians to initiate or intensify GDMT may stem from concerns about its potential side effects, perceived patient tolerance issues, or a preference for maintaining the status quo in treatment plans. One of the strategies that can be used in an attempt to overcome physician inertia is the fulfillment of a discharge checklist to review the discharge prescriptions being administered, thus offering a chance to initiate or intensify GDMT [
8].
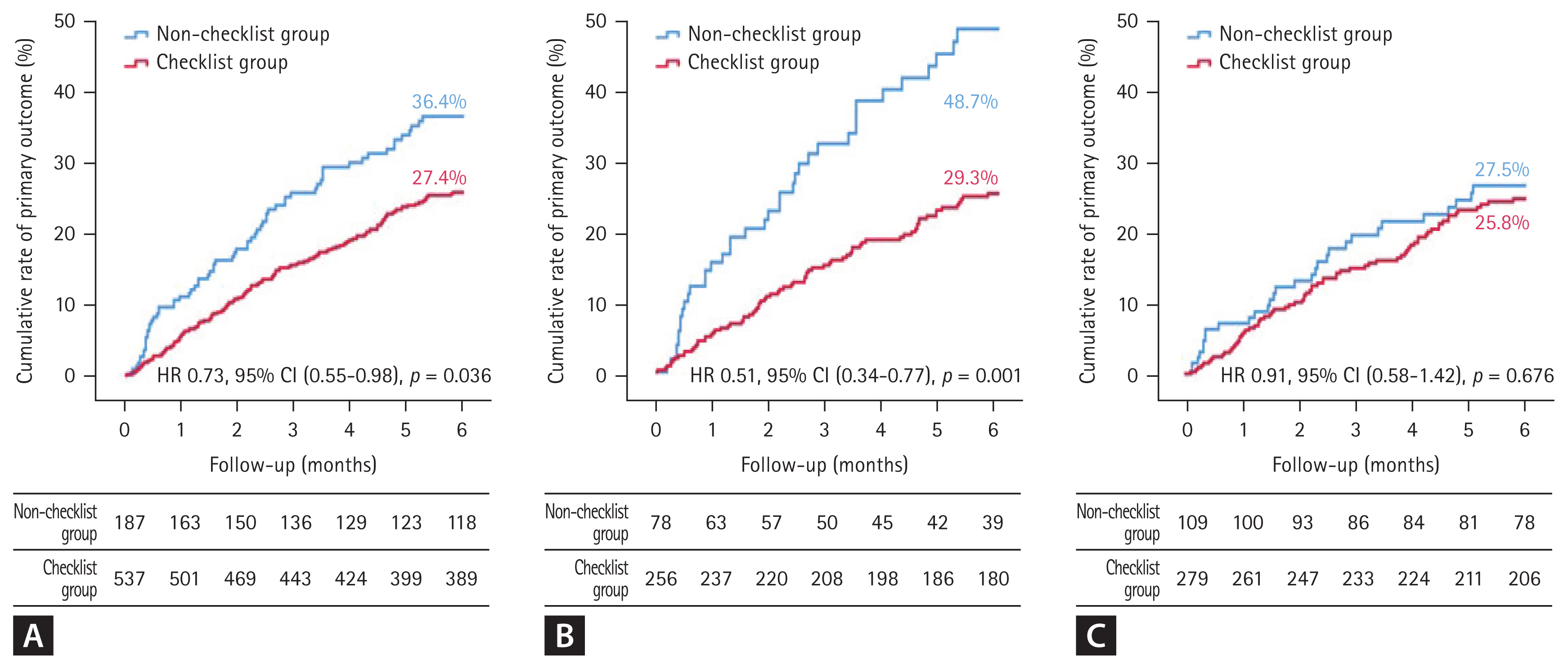
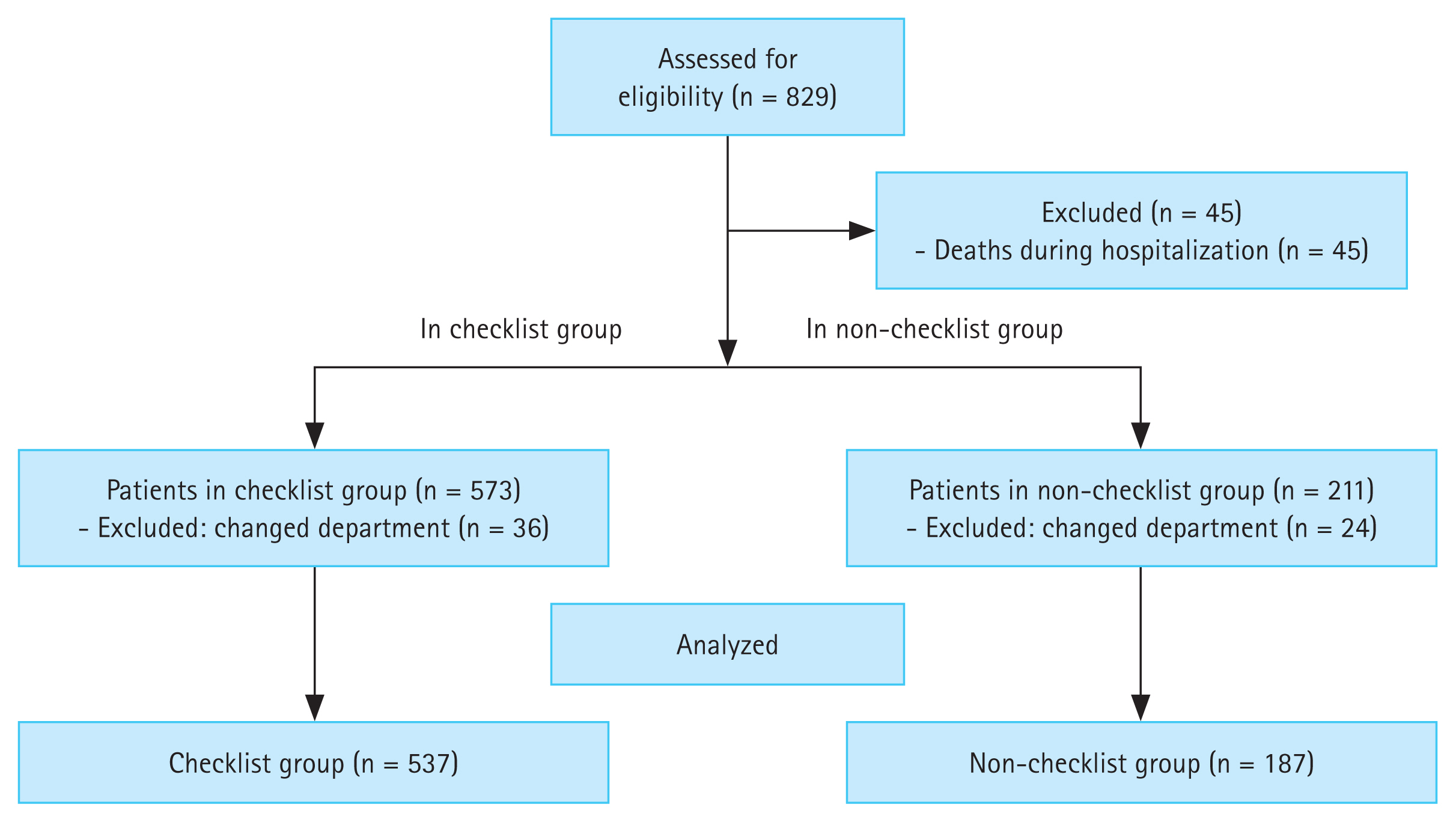
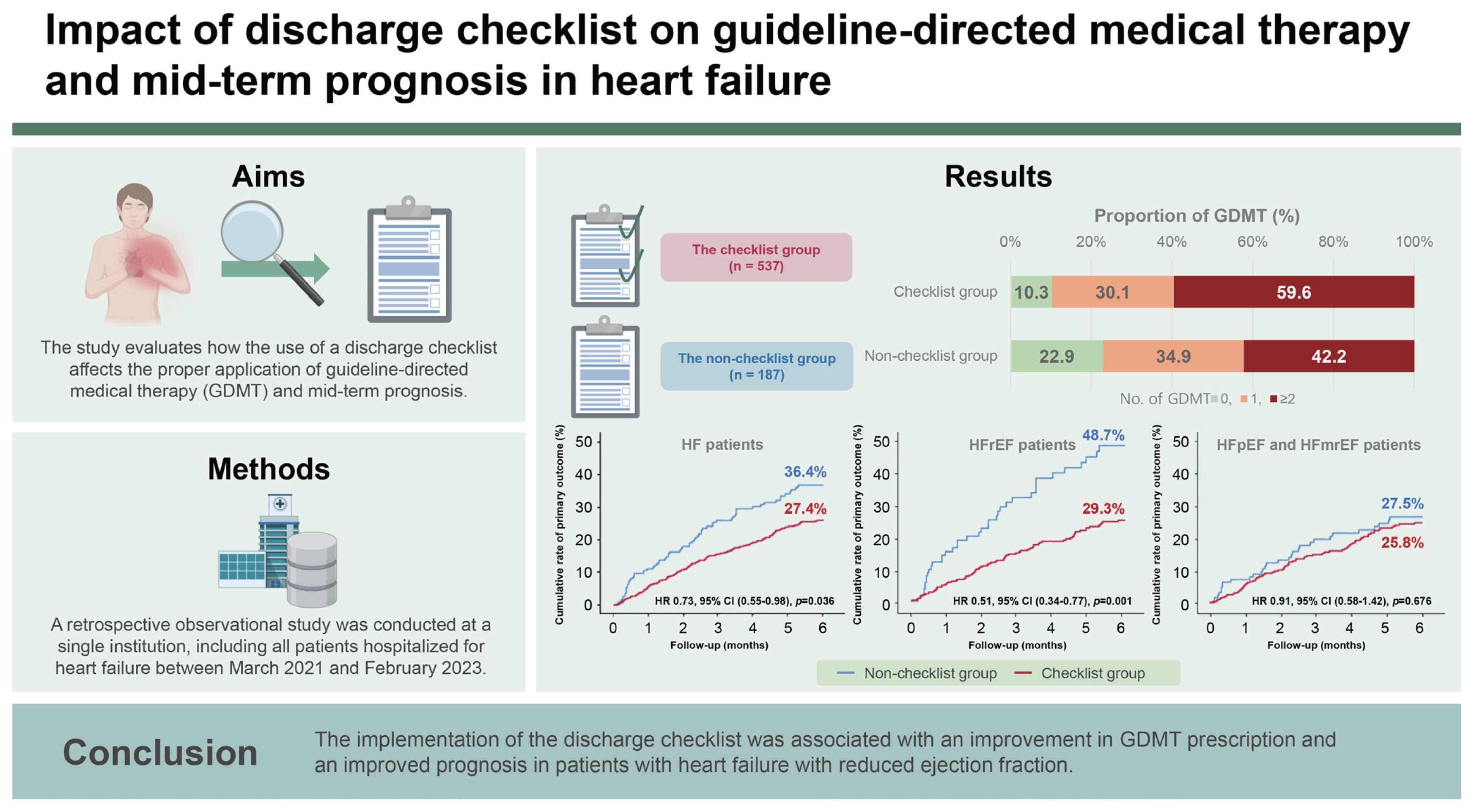
Surprisingly, the use of the discharge checklist was associated with a 55% lower risk of short-term death and rehospitalization within two months. However, since the previous study was small-scale and only had a follow-up period of two months, we aimed to confirm the beneficial effect in a larger-scaled, longer follow-up study. We also evaluated the impact of the discharge checklist according to the HF phenotypes: HF with reduced ejection fraction (HFrEF) and HF with mildly-reduced or preserved ejection fraction (HFmrEF and HFpEF).
DISCUSSION
The current study evaluated the impact of a discharge checklist on the prescription of GDMT and clinical outcomes in patients who were hospitalized for acute HF. The checklist group exhibited a significantly lower composite outcome of all-cause mortality or HF readmission within 6 months, which could be attributable to the significantly higher GDMT prescription rate. This beneficial effect was shown to persist after adjusting for various clinical variables, suggesting that the completion of the discharge checklist contributes to improved outcomes in HF patients. In a previous paper we reported the results of a small, short-term observational study which suggested that discharge checklist usage might be an effective strategy for GDMT initiation during hospitalization and that it could also be beneficial in terms of short-term outcome in two months [
9]. This study confirmed the findings of the previous study in a larger, longer follow-up study. The present study is also meaningful for the following reasons: First, completion of the discharge checklist had greater impacts on GDMT rate and clinical outcomes in patients with HF in HFrEF than it did in HFpEF/HFmrEF. Most of the main contents of the HF discharge checklist that have been published by the Korean Heart Failure Society focus on HFrEF management. This may explain why completing the discharge checklist had a greater impact on clinical outcomes in patients with HFrEF than it did in those with HFpEF/HFmrEF in our study. Approximately 50% of HF patients are reported to have HFpEF [
17]. HFpEF/HFmrEF is also associated with considerable mortality [
18]. Early intervention and optimization of the prevention and treatment of comorbidities could potentially prevent adverse events in patients with HFmrEF/HFpEF. Because HFmrEF/HFpEF has different characteristics from HFrEF, the contents of the discharge checklist should be constructed differently according to the HF classification. Second, the rate of completion of the discharge checklist was more than 50% in patients with HFrEF, while it was less than 50% in patients with HFpEF/HFmrEF in our study. Therefore, despite the reported effectiveness of SGLT2 inhibitors in patients with HFmrEF/HFpEF, the prescription rate of SGLT2 inhibitors was lower in patients with HFmrEF/HFpEF than it was in those with HFrEF. This suggests that physicians are either unaware of or not interested in the management of HFmrEF/HFpEF patients. Therefore, there is a need for further research and efforts to care for and effectively manage patients with HFmrEF/HFpEF. Third, although the adverse event rate was lower in the checklist group than it was in the non-checklist group, the rate of adverse events gradually increased over time in both groups (
Fig. 2). This result suggests that the discharge checklist may have affected the initiation of GDMT, but that it did not affect the up-titration of GDMT. According to the STRONG-HF study, an intensive treatment strategy of rapid up-titration of GDMT after an acute HF admission reduced symptoms, improved quality of life, and reduced the risk of death or HF readmission [
19]. Altogether, these findings indicate that it is important not only to initiate GDMT, but also to rapidly up-titrate GDMT until the patient can tolerate it. Considering this, although the completion of the discharge checklist impacts GDMT initiation, it may not affect the up-titration of GDMT or clinical inertia.
In this study, the discharge checklist was used solely for educational purposes. However, if the clinical significance of the discharge checklist were to be recognized, it is anticipated that the checklist could also come to be utilized by HF specialists to confirm patient discharges.
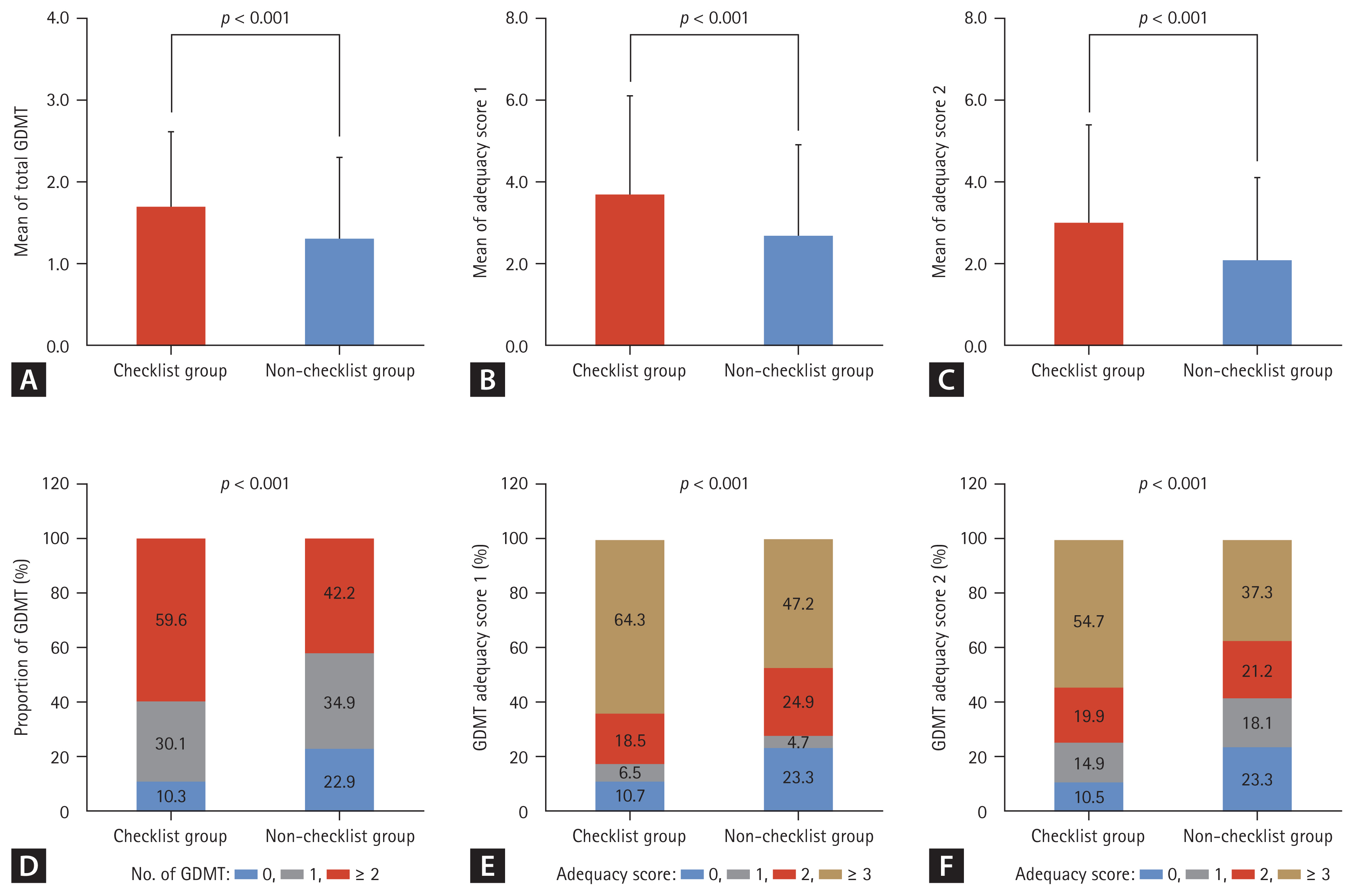
The results revealed the existence of a significant association between checklist completion and increased GDMT prescription, showcasing the checklistŌĆÖs efficacy in optimizing medical therapy for HF patients. Although GDMT prescription has benefits for HF patients, research has shown a lack of adherence to GDMT prescriptions in the real world. According to the Acute Decompensated HF National Registry (ADHERE) in the United States, only 83%, 80%, and 33% of patients received prescriptions for RASI, beta-blockers, and MRA, respectively [
20]. In the Asia-Pacific region, GDMT prescription rates were even lower. According to the Acute Decompensated HF Registry International-Asia Pacific (ADHERE-AP), only 63%, 41%, and 31% of patients were prescribed RASI, beta-blockers, and MRA, respectively [
21]. The existence of a higher number of GDMT classes and higher adequacy scores in the checklist group underscores the checklistŌĆÖs role in guiding physicians toward a more comprehensive prescription. This finding aligns with the results of previous studies emphasizing the underutilization of GDMT in real-world practice and highlights the checklist as a potential solution to address this gap. The checklistŌĆÖs impact on blood pressure readings and heart rate categories suggests that it influences not only medication choice but also individualized treatment adjustments, which ultimately emphasizes its role in tailoring therapy to patient needs.
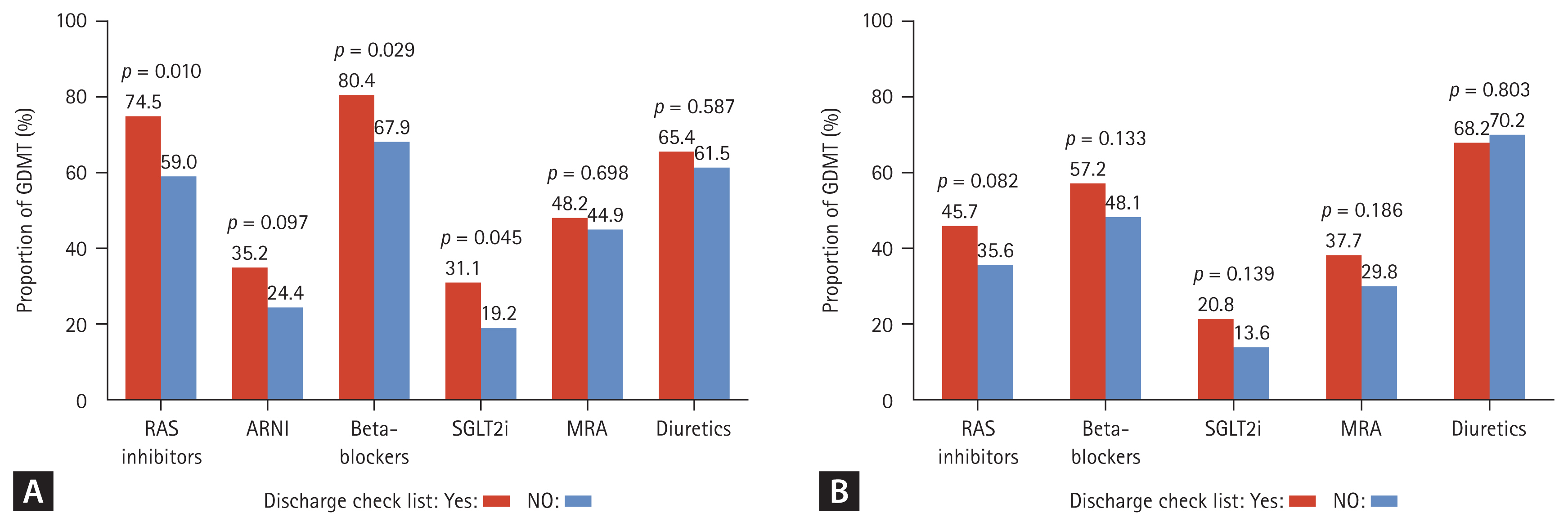
An analysis in which the results were stratified based on HF phenotypes revealed a substantial impact on HFrEF patients, with higher prescription rates of RASI, beta-blockers, and SGLT2i in the checklist group. This aligns with existing evidence supporting the efficacy of GDMT in HFrEF. Previous studies demonstrated the efficacy of four pillars for HFrEF therapy, and our previous study reported that discharge checklist usage is an effective strategy for GDMT initiation during hospitalization. The discharge checklist also improves adherence to GDMT in patients with HFrEF. Survival analysis demonstrated the existence of a significantly lower event rate in the checklist group, particularly in HFrEF patients. This suggests that the checklistŌĆÖs impact extends beyond prescription rates, as it influences clinical outcomes such as all-cause mortality and HF readmission. However, the lack of a significant difference on clinical outcomes in HFpEF and HFmrEF patients underscores the complexity involved in managing these conditions and raises questions about the checklistŌĆÖs effectiveness in improving outcomes in these specific populations. This may reflect the ongoing challenges in establishing evidence-based therapies for these HF subtypes while also highlighting the need for further research to identify effective treatment strategies for patients with preserved or mildly-reduced ejection fraction [
15,
16]. As effective therapies come to be established for patients with preserved or mildly-reduced ejection fraction, the utility of the discharge checklist is expected to increase for these individuals.
Survival analysis demonstrated a significantly lower event rate in the checklist group, particularly in HFrEF patients. This suggests that the checklistŌĆÖs impact extends beyond prescription rates, in turn influencing clinical outcomes such as all-cause mortality and HF readmission. The lack of a significant difference in HFpEF and HFmrEF patients underscores the complexity of managing these conditions and raises questions about the checklistŌĆÖs effectiveness in improving outcomes in these specific populations. The results of univariable and multivariable analyses further supported the checklistŌĆÖs independent association with lower event rates, ultimately emphasizing its potential utility as a valuable tool in the management of HF patients.
This study set a hypothesis predicting that the completion of a discharge checklist would improve patient outcomes by ensuring better physician adherence to guidelines when prescribing medications. This hypothesis can be divided into two assumptions: first, that checklist completion increases the prescription rate of GDMT, and second, that elevated GDMT prescription rates lead to improved patient outcomes. Previous research has supported each of these assumptions. In a study evaluating the effectiveness of a discharge checklist in the care of patients with acute decompensated HF, it was concluded that the discharge checklist serves as a simple tool to ensure the prescription of GDMT [
22]. Further, although not a discharge checklist specifically, another study evaluating the impact of checklists on medication prescriptions for HF patients found that the checklist group exhibited a higher prescription rate of RASI compared to the non-checklist group [
8]. In the current study, patients in the checklist group also demonstrated a higher GDMT adequacy score compared to patients in the non-checklist group, thus aligning with the anticipated results.
There is substantial evidence supporting the idea that GDMT contributes to improved patient outcomes. According to the real-life SMYRNA study, the non-use or suboptimal use of GDMT is associated with increased rates of hospitalization and cardiovascular death in patients with HF [
23]. Clinical trials evaluating the effects of GDMT in specific patient populations have also emphasized the importance of considering the prescription of medications included in GDMT for potential benefits in such populations [
24,
25].
Despite the compelling findings it has obtained, the present study has certain limitations that warrant consideration. First, its retrospective nature may introduce biases and limit the establishment of causation. For instance, clinicians might have been inclined to utilize the checklist more frequently for patients with more severe profiles, with the aim of ensuring thorough care at discharge. To mitigate bias, we conducted comparisons of baseline characteristics and performed subgroup analyses. Additionally, the study was conducted in a single-center, which potentially limited the generalizability of its results to broader populations. The reliance on retrospective data collection and the exclusion of patients who died or were transferred to other departments during hospitalization may also have introduced selection bias. Further, the studyŌĆÖs duration and follow-up period may not capture long-term effects, and caution should be taken when considering the checklistŌĆÖs generalizability to different healthcare settings.
In conclusion, the findings of this study support the use of a discharge checklist as a valuable intervention to enhance GDMT prescription and improve clinical outcomes in patients hospitalized for HF, particularly those with reduced ejection fraction. However, this studyŌĆÖs limitations underscore the need for further research, including prospective, multicenter studies, to validate these findings and address potential biases. Future investigations should explore the effectiveness of the checklist in different HF phenotypes and its long-term impact on patient outcomes to optimize its implementation in clinical practice.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement figure 1
Supplement figure 1 Print
Print



