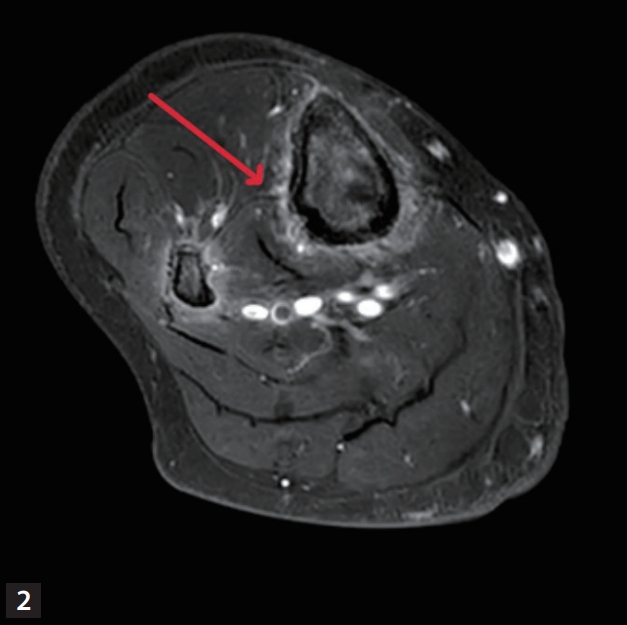
A 58-year-old female was admitted to a hospital for progressive both leg pain and swelling for 1 month. She has a history of myelofibrosis, transformed into acute myeloid leukemia, and received allogeneic hematopoietic stem cell transplantation (HSCT) 2 months ago. One month after HSCT, she was diagnosed as probable invasive pulmonary aspergillosis and received oral voriconazole. After 1 month of voriconazole therapy, she was admitted for progressive swelling and tenderness on both foot and ankle (around malleolus). Absolute neutrophil count was 2,000 u/L (reference value 2,500–7,000 u/L). The blood level of C-reactive protein was 13.6 mg/dL (reference value 0–0.6 mg/dL), creatine kinase 11 U/L (reference value 25–200 U/L), and alkaline phosphatase 351 IU/L (reference value 44–147 IU/L). Empirical cefazolin for possible cellulitis showed no improvement. Bilateral lower leg X-ray showed diffuse thin linear periosteal reaction in both tibia and fibula and diffuse soft tissue swelling in both lower legs (Fig. 1). Magnetic resonance imaging (MRI) of bilateral lower leg revealed diffuse high signal intensity and enhancement along the periosteum of tibia and fibula (Fig. 2).
What is the diagnosis?
DIAGNOSIS: VORICONAZOLE-ASSOCIATED PERIOSTITIS
Blood voriconazole level was 2.7 μg/mL (therapeutic range 1.0–6.0 μg/mL). Imaging suggested possible periostitis. After discontinuation of voriconazole, symptoms started to improve within a month and resolved in a year.
Voriconazole contains three fluoride atoms, when compared to posaconazole and fluconazole which contain two [1-3]. The previous study showed that voriconazole develops hyper-fluorosis, potentially associated with periostitis, whereas other azoles such as fluconazole and posaconazole has lower risk for this condition [4] The most common symptom for voriconazole-associated periostitis is localized diffuse bone pain [5-8]. Radiographs show periosteal reaction, periosteal bone formation and periosteal thickening [8]. Computed tomography reveals periosteal reaction and exostoses [9]. MRI showed thick and irregular periosteal edema along the outer cortical surfaces of the bilateral proximal femoral shafts indicative of periostitis [9-11]. Symptoms usually resolves after discontinuation of voriconazole.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





