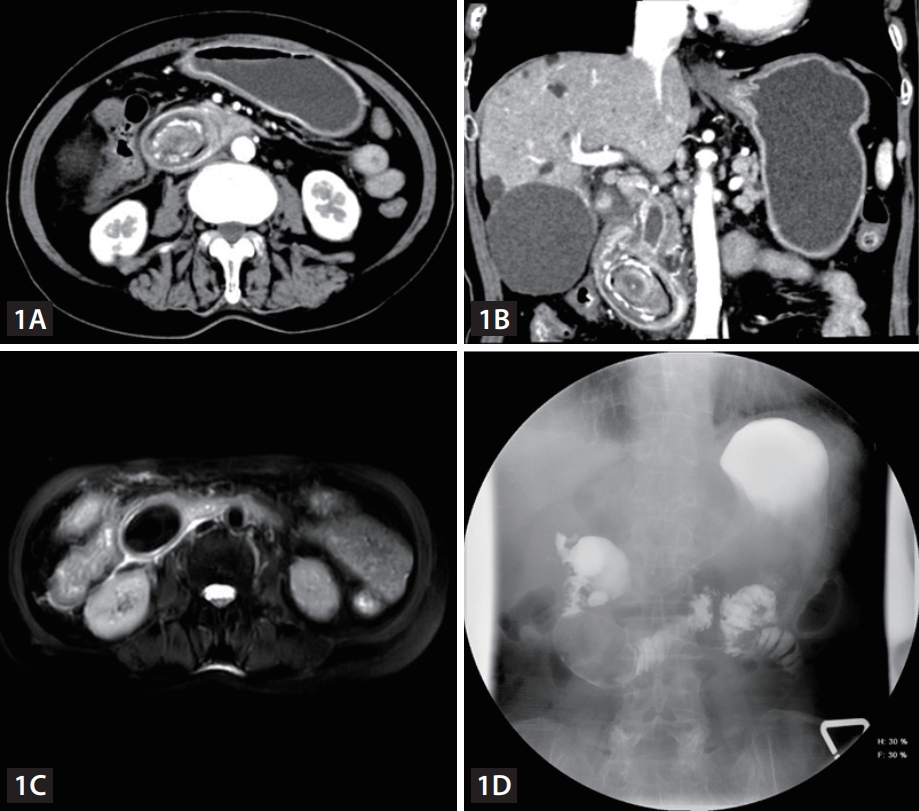
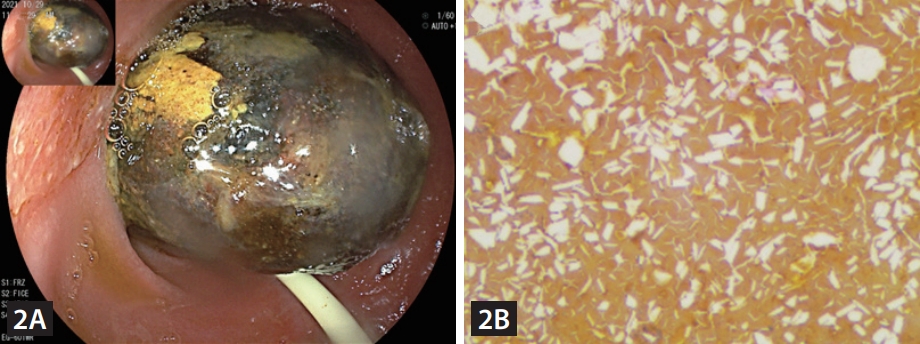
A 76-year-old woman was hospitalized because of abdominal pain for 10 hours. Physical examination showed epigastric tenderness without rebound pain. No palpable mass was found. An initial laboratory finding revealed an elevated serum amylase level of 745 IU/L (normal range, 35 to 135 IU/L) and elevated C-reactive protein of 112 mg/L (normal range, 0ŌĆō12 mg/L). The hemoglobin level was 11.0 g/dL (normal range: 13ŌĆō17.5 g/dL). CA19ŌłÆ9 was 55 IU/ mL (reference range, 0ŌłÆ40 IU/mL). Aspartate aminotransferase and alanine aminotransferase were normal. Alkaline phosphatase was 197 IU/L (normal range: 50ŌĆō130 IU/L), and gamma-glutamyl transpeptidase was 135 IU/L (normal range: 10ŌĆō60 IU/L). Acute pancreatitis was initially diagnosed. However, computed tomography of the abdomen showed a well-defined, ovoid-shaped, intraluminal mass in the descending segment of duodenum causing high grade dilation of common bile duct (Fig. 1A, B), characterized by a solid outer rim and a heterogeneous central portion, which was well-defined by magnetic resonance imaging and upper gastrointestinal barium radiograph (Fig. 1C, D). Ultrasound guided percutaneous transhepatic biliary drainage was reserved just in case of the aggravated obstructive jaundice. Endoscopy showed one huge phytobezoar near the duodenal papilla (Fig. 2A). Further questioning of the patient found that she had eaten dried persimmons. Endoscopic fragmentation with biopsy forceps was failed due to the hard consistency. She ingested Coca-Cola but developed vomiting and duodenal obstruction. An exploratory laparotomy was subsequently performed on the patient. An elastic intraluminal phytobezoar, measured 5 ├Ś 3 ├Ś 3 cm, obstructed the duodenum. Histopathology confirmed the phytobezoar (Fig. 2B).
Bezoars are conglomerates, commonly caused by hypochlorhydria, diminished antral motility and incomplete degradation of food, which are classified as trichobezoar, phytobezoar, and pharmacobezoar on the basis of composition [1]. Phytobezoar-induced common bile duct obstruction and acute pancreatitis remains an uncommon diagnosis, suspected in patients with an increased risk of bezoars formation, which poses a diagnostic and management challenge. Abdominal computed tomography is the preferred diagnostic modality for phytobezoar-induced common bile duct obstruction. Treatments of phytobezoar include enzymatic dissolution therapy, endoscopic fragmentation and removal, and dissolution by Coca-Cola [2,3]. Migration of phytobezoar to duodenum are usually treated surgically. Excessive consumption of foods rich in vegetable fibers should be avoided to prevent phytobezoar. The postoperative period was uneventful. A follow-up abdominal radiography 7 days later no longer showed dilation of common bile duct. The patient was discharged 1 week later.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





