 |
 |
| Korean J Intern Med > Volume 39(5); 2024 > Article |
|
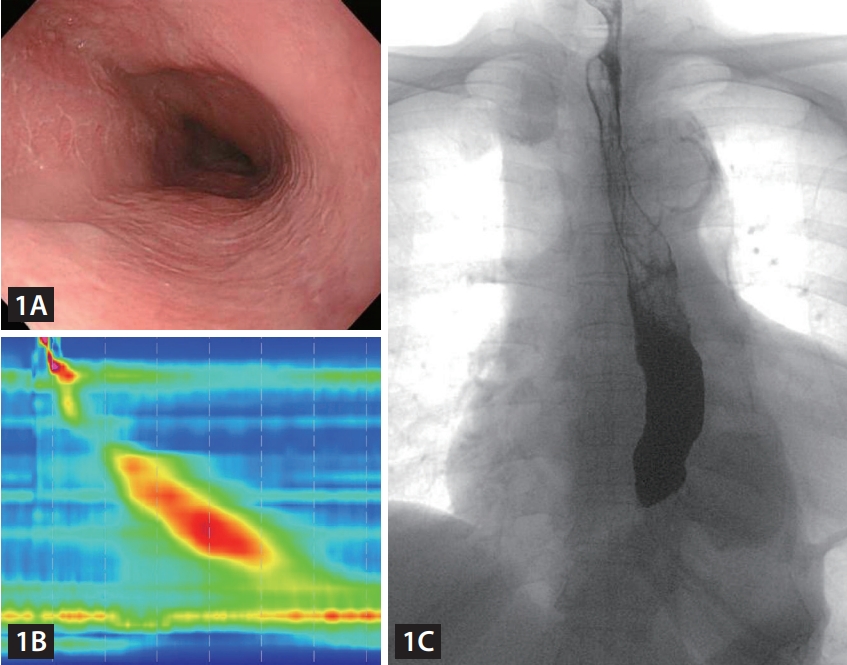
An 80-year-old woman presented to the hospital with symptoms of difficulty in swallowing both solids and liquids as well as vomiting, which she had been experiencing for 6 months. In the patientŌĆÖs medical history, she had long experienced a lump in the upper abdomen. She also had a history of diabetes, hyperlipidemia, and hypertension. Upper endoscopy revealed a widened esophageal lumen with fluid retention (Fig. 1A). Subsequent high-resolution manometry showed high integrated relaxation pressures of 43 mmHg (supine) and 60 mmHg (erect), with no evidence of disordered peristalsis (Fig. 1B). Esophagography findings included a narrow esophagogastric junction and delayed emptying of barium (Fig. 1C).
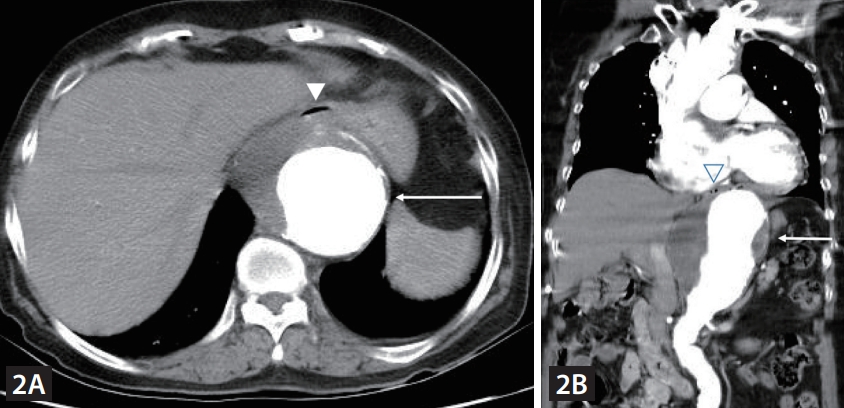
Chest computed tomography revealed an aortic aneurysm, with a maximum diameter of 9.5 cm, extending from the descending thoracic aorta to the upper abdominal aorta. The aneurysm was pressing the lower esophagus anteriorly (Fig. 2A, B). Consequently, the patientŌĆÖs dysphagia was determined to be an esophagogastric junctional outlet obstruction secondary to compression from an aortic aneurysm. Vascular treatment was recommended; however, the patient was transferred to another hospital to explore treatment alternatives besides surgery.
Dysphagia aortica, a rare cause of secondary esophagogastric junction outlet obstruction, occurs when an aortic aneurysm externally compresses the esophagus against the left atrium [1,2]. This mechanical obstruction hinders the downward movement of the food bolus. This condition is typically associated with certain risk factors, including female sex, elderly age, hypertension, short stature, and kyphoscoliosis [3,4]. Although dysphagia aortica is uncommon, it is critical to consider it in the differential diagnosis of secondary esophagogastric junctional outflow obstruction or achalasia because of the urgent need for rapid diagnosis and effective treatment, given its association with severe complications from aortic aneurysms.
Notes
REFERENCES
1. Kim JH, Jang SW, Kim DB, et al. A patient with dysphagia due to an aortic aneurysm. Korean Circ J 2009;39:258ŌĆō260.



2. Choi SHJ, Yang GK, Gagnon J. Dysphagia aortica secondary to thoracoabdominal aortic aneurysm resolved after endograft placement. J Vasc Surg Cases Innov Tech 2019;5:501ŌĆō505.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



