 |
 |
| Korean J Intern Med > Volume 39(1); 2024 > Article |
|
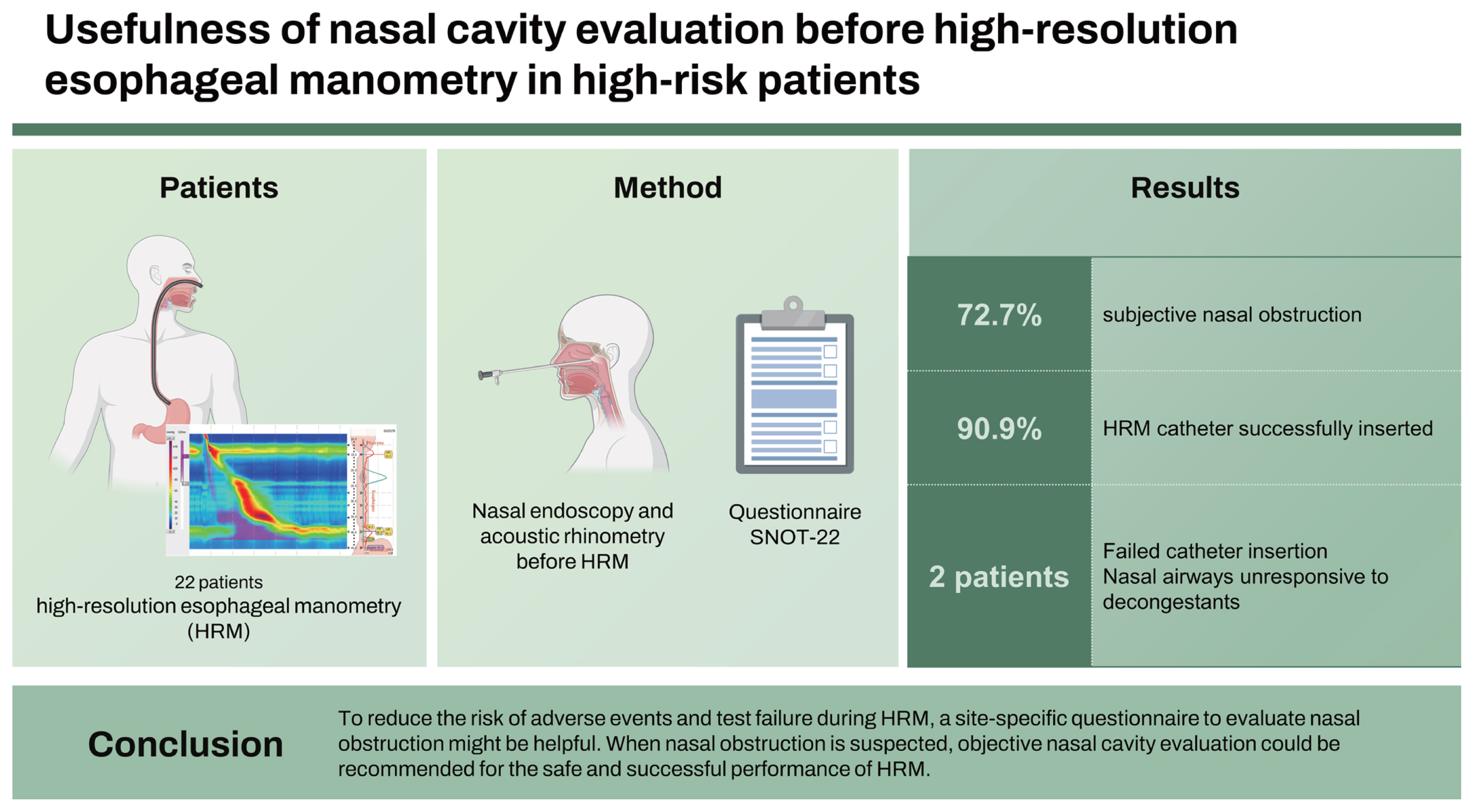
Abstract
Background/Aims
A catheter is inserted through the nasal cavity during high-resolution esophageal manometry (HRM), which may cause adverse events such as pain or epistaxis. Despite these possible safety considerations, studies on this subject are very limited. We aimed to investigate the usefulness of nasal cavity evaluation before HRM to reduce the risk of adverse events and test failure.
Methods
Patients who underwent HRM after consultation with the ear-nose-throat department for nasal evaluation were retrospectively enrolled between December 2021 and May 2022. The included patients had a previous history of sinonasal disease or surgery or had subjective nasal discomfort. All patients answered the Sino-Nasal Outcome Test (SNOT-22) questionnaire, and subjective nasal discomfort was scored using a visual analog scale. Nasal endoscopy and acoustic rhinometry were performed for disease evaluation and volumetric assessment.
Results
The analysis included 22 patients with a mean age of 58.9 years. The mean SNOT-22 score was 24.2, and 16 patients (72.7%) complained of subjective nasal obstruction. The HRM catheter was successfully inserted in 20 patients (90.9%), without any significant adverse events. The objective measurement outcomes of acoustic rhinometry and sinus endoscopy did not always correspond to subjective symptoms. Narrowed nasal airways unresponsive to decongestants were observed in two patients with failed catheter insertion.
Esophageal manometry is used to evaluate the motor function and coordinated muscle movement of the esophagus. This technique plays a pivotal role in investigating the presence of major esophageal motility disorders in patients with dysphagia or non-cardiac chest pain and in excluding major motor dysfunction in the diagnosis of functional esophageal disorders [1,2]. Guidelines also recommend esophageal manometry before antireflux surgery for gastroesophageal reflux disease (GERD) [3,4].
High-resolution esophageal manometry (HRM) is a recently developed technology that enables dynamic and comprehensive evaluation of esophageal motility. Multichannel pressure sensors closely arranged in the HRM catheter visualize continuous pressure topography, thereby yielding a number of advantages such as simple implementation, a short examination time, standardized data acquisition, and high reproducibility [5]. This catheter is introduced into the patientŌĆÖs esophagus through the nostril in a blind manner to evaluate esophageal movement.
Anatomically, the nasal cavity is divided into two spaces by the nasal septum, and turbinate structures are located in each nasal cavity. Deviation of the nasal septum or hypertrophy of the inferior turbinates decreases the diameter and volume of the nasal cavity [6]. The presence of chronic rhinosinusitis with nasal polyps (CRSwNP) could also decrease the diameter and volume of the nasal cavity, narrowing the normal nasal airway passage. If patients with underlying conditions such as deviation of the nasal septum with/without inferior turbinate hypertrophy or CRSwNP, transnasal catheter insertion could induce complications such as discomfort or nasal mucosal damage inducing epistaxis [7]. Although these complications are usually considered minor, they may affect the tolerability of the procedure and impede successful performance of HRM. However, subjective nasal discomfort does not correspond to the objective condition of the nasal cavity [8]. For example, approximately 30% of patients with nasal septum deviation reportedly had no complaint of nasal obstruction [9].
Despite these concerns, there are few reports on the complications, side effects, and tolerability of catheter placement during HRM [10]. Although it seems that preprocedural evaluation of the nasal cavity before HRM could reduce such problems and facilitate a safe and easy examination process, nasal inspection prior to HRM is not commonly considered or recommended in real clinical practice. Therefore, in this study, we examined the usefulness of evaluation of the nasal cavity before HRM.
Data from patients who underwent HRM after visiting the gastroenterology department and had a consultation with the ear-nose-throat (ENT) department at Chung-Ang University Hospital from December 2021 to May 2022 were retrospectively reviewed. Patients who had undergone previous sinonasal surgery such as septoplasty with/without turbinoplasty or endoscopic sinus surgery, those who were previously diagnosed with septal deviation or rhinosinusitis, and those who had subjective nasal discomfort underwent consultation with the ENT department for nasal airway evaluation. This study was approved by the Institutional Review Board of Chung-Ang University Hospital (2210-004-19439) and conducted in accordance with the Declaration of Helsinki. Due to the retrospective nature of this study, patient consent was waived.
All patients answered the Sino-Nasal Outcome Test (SNOT-22) questionnaire regarding sinonasal quality of life [11], and subjective nasal discomfort of the left and right nasal cavities was scored using a visual analog scale (VAS) score using a 10-cm VAS ruler (0 cm [no symptoms] to 10 cm [most troublesome]). For the evaluation of nasal airway patency as well as the presence and extent of nasal disease, a comprehensive assessment of the septum and turbinate is necessary. Since anterior rhinoscopy alone cannot diagnose posterior septal deviation, nasal endoscopy was performed, and this was done by one skilled ENT physician. To further perform a volumetric assessment of nasal airway dimensions, acoustic rhinometry (Acoustic rhinometer A1; GM instruments Ltd, Kilwinning, UK) was performed. Acoustic rhinometry was performed both before and 15 minutes after decongestion with 1% ephedrine solution-soaked cotton. All procedures were performed by the same technician in the same room and in the same air conditions throughout the study. The parameters of acoustic rhinometry were as follows: (1) minimal cross-sectional area (MCA) of the nasal cavity, (2) distance from the nostril to the point of the MCA, and (3) nasal volume (NV) recorded between 0 and 4 cm [12]. Based on endoscopic and acoustic rhinometry findings, the ENT physician recommended the best site for the HRM procedure. In patients whose nasal airway was thought to be too narrow for passage of the HRM catheter, 1% ephedrine solution-soaked cotton was applied 15 minutes before the HRM procedure.
The InSight Ultima system (Diversatek Healthcare, Highlands Ranch, CO, USA) was used to perform HRM in our study. This high-resolution impedance manometry system included a 12-French solid-state manometry catheter with 32 circumferential pressure sensors spaced 1 cm apart and 16 impedance sensors spaced at 2-cm intervals. The catheter was calibrated for pressure according to the manufacturersŌĆÖ instructions before the test. The patients were instructed to stop medications affecting gastrointestinal motility for at least 48 hours and to fast for eight hours prior to the examination. Prior to insertion, a water-soluble lubricant gel was applied to lubricate the manometry catheter. Then, the catheter was advanced through one nostril according to the recommendations from the ENT department after consultation, and it was positioned in the stomach with approximately three intragastric sensors in an upright position. Pressure data were then acquired in a supine position after fixing the catheter to the patientŌĆÖs nose. After recording the basal sphincter pressure for at least 30 seconds, patients were asked to swallow 5 mL of room temperature water 10 times at an interval of 20ŌĆō30 seconds.
The recorded HRM metrics included the length and basal pressure of the lower esophageal sphincter, basal and residual pressure of the upper esophageal sphincter, contractile front velocity, distal wave amplitude, and mean wave duration. The esophagogastric junction (EGJ) morphology and integrated relaxation pressure were evaluated to assess the structure and function of the EGJ. Parameters such as the distal latency (DL), distal contractile integral, and peristaltic integrity were also evaluated to assess the esophageal contractile function. Manometry profiles were analyzed, and the pressure data were displayed using the Zvu Advanced GI Diagnostic Software version 3.0 (Diversatek Healthcare). The data were interpreted according to the Chicago Classification version 3.0 [13].
A total of 22 patients were reviewed in this study, including 10 male and 12 female patients (Table 1). The mean age was 58.9 years. The most common indications for HRM were to determine the refractoriness of typical symptoms of GERD, namely heartburn or reflux, to perform a preoperative evaluation, and to evaluate dysphagia. The mean SNOT-22 score was 24.2, and the number of patients who had subjective nasal obstruction was 16 (72.7%). Two patients had a previous history of sinonasal surgery. The HRM catheter was successfully inserted in 20 patients (90.9%).
HRM was completed in 19 patients, except for one patient who wanted to stop in the middle of the test after successful insertion of the catheter. The results of HRM are summarized in Supplementary Table 1. There were seven patients with disorders with EGJ outflow obstruction and three patients with minor motility disorders including ineffective esophageal motility and fragmented peristalsis. The remaining nine patients showed normal esophageal motility. There were no significant adverse events related to HRM.
The results of acoustic rhinometry are summarized in Table 2. The increased ratio of the MCA after decongestion was 40.90 ┬▒ 40.50% and 86.46 ┬▒ 213.18% in the left and right nasal airways, respectively. The increased ratio of the mean NV after decongestion was 42.80 ┬▒ 37.03% and 36.59 ┬▒ 25.37% in the left and right nasal airways, respectively (Table 2).
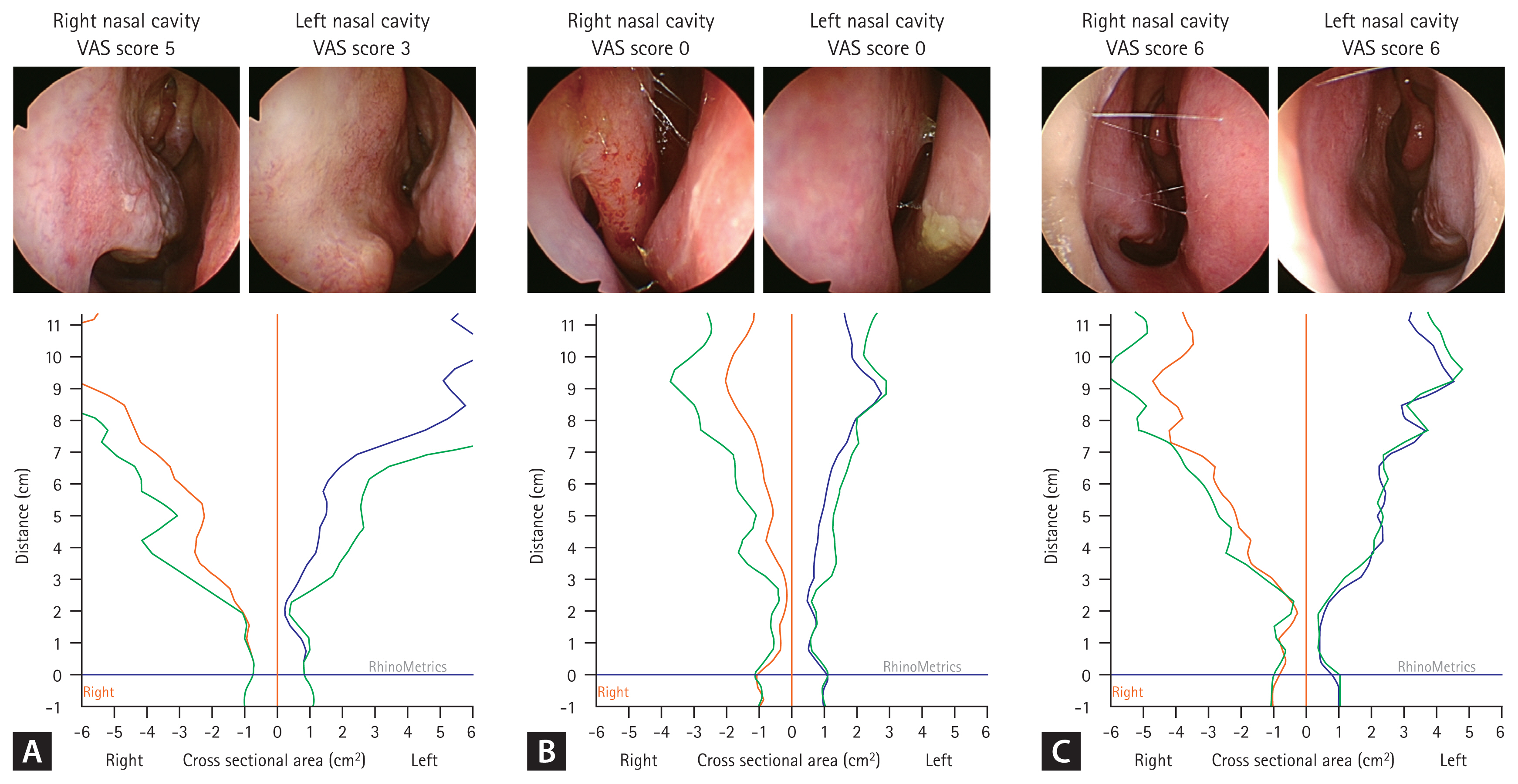
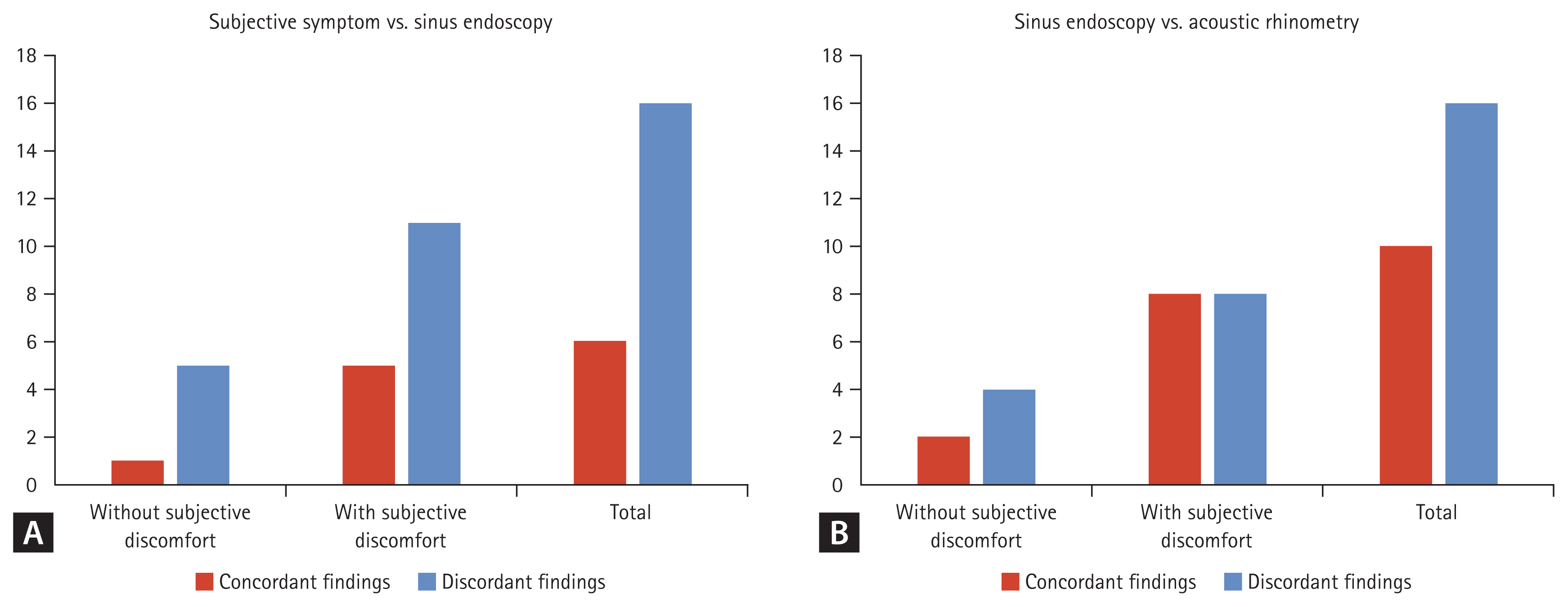
We compared the objective measurement outcomes of acoustic rhinometry and sinus endoscopy with patient discomfort as demonstrated by the VAS score to reveal that they are not always correlated. For example, one patient who had considerable subjective discomfort in the right nasal cavity was found to have septal deviation to the left and narrowing of the left nasal cavity on sinus endoscopy and acoustic rhinometry (Fig. 1A). Another patient without subjective nasal discomfort was demonstrated to have severely narrowed nasal airways on both sides on sinus endoscopy and acoustic rhinometry (Fig. 1B). Yet another patient complained of subjective nasal obstruction in both nasal airways; however, both nasal airways were patent on sinus endoscopy (Fig. 1C). Therefore, as a first step, we evaluated the relationship between patientsŌĆÖ subjective recognition of nasal discomfort and sinus endoscopic findings. We found that 27.3% (6 of 22 patients) had no subjective discomfort, and 72.7% (16 of 22 patients) had subjective nasal discomfort. Among patients without subjective symptoms, only 16.7% (1 of 6 patients) of patients were diagnosed with patent both nasal airways on sinus endoscopy, which corresponded with their subjective symptoms. In patients with subjective discomfort, 31.3% (5 of 16 patients) were diagnosed with narrowed nasal airways on sinus endoscopy, which corresponded with their subjective symptoms (Fig. 2A). In the next step, we evaluated and compared the results of sinus endoscopy and the measurement outcomes of acoustic rhinometry according to subjective symptoms. In six patients without subjective discomfort, the sinus endoscopic findings and measurement outcomes of acoustic rhinometry demonstrated the same findings regarding a suitable site for HRM catheter insertion in 33.3% of patients (2 of 6 patients) and did not in 66.7% of patients (4 of 6 patients). In 16 patients with subjective nasal discomfort, the sinus endoscopic findings and measurement outcomes of acoustic rhinometry demonstrated the same findings regarding a suitable site for HRM catheter insertion in 50.0% of patients (8 of 16 patients) and did not in 50.0% of patients (8 of 16 patients) (Fig. 2B).
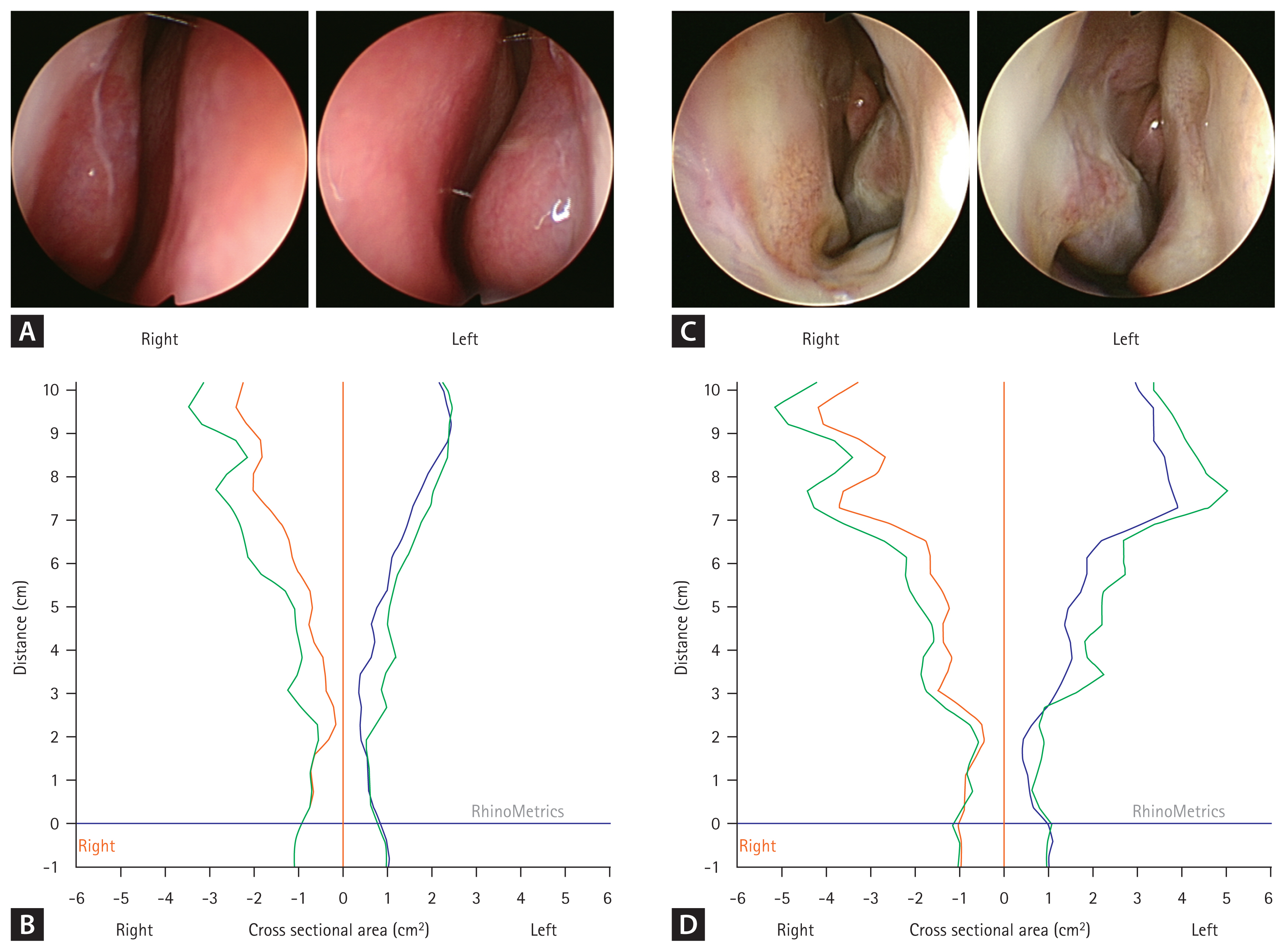
The sinus endoscopic findings and results of acoustic rhinometry of two cases of failed catheter insertion were reviewed. In one patient, both nasal airways were severely narrowed on sinus endoscopy (Fig. 3A), and this did not improve after treatment with a decongestant (Fig. 3B). In another patient, although the anterior lower nasal airways were narrowed due to septal bony deviation on both sides, the upper nasal airways were patent (Fig. 3C). The acoustic rhinometry results demonstrated that the narrowed anterior lower nasal airways did not improve after treatment with a decongestant (Fig. 3D).
In the field of gastroenterology, HRM is frequently performed in patients complaining of relevant esophageal symptoms. This technique is especially essential in confirming or excluding the presence of major motility abnormalities in the esophagus [1]. Although HRM is considered a relatively safe procedure, adverse events or severe discomfort can sometimes occur during catheter placement, leading to poor patient compliance, suboptimal test performance, inaccurate test results, or even test failure. Therefore, we evaluated the usefulness of nasal cavity evaluation before HRM.
In this study, an ENT physician evaluated subjective symptoms as well as the objective nasal cavity patency of both sides and recommended the best suitable site for HRM catheter insertion in patients with a previous history of sinonasal surgery or nasal discomfort. Subjective symptoms were present in approximately 3/4 of the study participants. To systematically assess subjective discomfort in patients, we utilized the SNOT-22 system, which has been proven to reflect the severity of sinonasal symptoms and the health-related quality of life in chronic rhinosinusitis patients [14]. Previous studies have also demonstrated the usefulness of this evaluation system in laryngopharyngeal reflux disease. Although there is no clear consensus on severity group classification based on scores, a previous meta-analysis reported a median value of approximately 11 in normal controls, and another study suggested cutoff values of ŌĆ£mildŌĆØ as 8ŌĆō20, ŌĆ£moderateŌĆØ as > 20ŌĆō50, and ŌĆ£severeŌĆØ as > 50 [15,16]. The mean SNOT-22 score in our study for the enrolled patients was 24.2 points. Considering that 56.3% of patients experiencing subjective symptoms had scores exceeding 20, it can be inferred that more than half of symptomatic patients experienced symptoms of at least a moderate severity level. In our study, most of the enrolled patients with a potential risk of difficult catheter insertion underwent HRM successfully without serious adverse events. We found that subjective patient discomfort did not correspond with the objective nasal airway patency assessed by sinus endoscopy in 72.7% of cases. Furthermore, in 88.2% of patients who had narrow airways observed on sinus endoscopy, the nasal airways could be widened with decongestants, and this was objectively measured by acoustic rhinometry.
The safety of flexible endoscopy via a transnasal route has been reported in previous studies. In a previous study, mild epistaxis occurred only in 1.1% of enrolled patients, and most of the patients were willing to undergo the test again [17]. Similarly, another study that included a large population of 500 patients reported that the prevalence of upper airway complications such as epistaxis or airway compromise was very rare, and 81% of patients reported no discomfort or mild discomfort as a result of the examination [18]. However, these prior studies were performed in an otolaryngology setting and involved a general population. If the subjects are presumably high-risk patients and the test is not performed in an otolaryngology setting, the risk of complications such as epistaxis or pain could be much higher. Although epistaxis is generally well controlled by conservative management in healthy subjects, severe nasal bleeding can occur in patients taking anticoagulants or in those with anatomic abnormalities and may even require surgical intervention. In the current study, no patient reported serious upper airway complications or airway problems after HRM or needed medical or surgical intervention. Since HRM procedures are not usually performed in an otolaryngology setting, evaluation of nasal airway patency before HRM could minimize the risk of potential upper airway complications, especially in patients expected to be at high risk of nasal obstruction.
In this study, we performed sinus endoscopy and acoustic rhinometry in combination with subjective discomfort questionnaires. Acoustic rhinometry is an assessment tool that measures sound waves that are reflected after being emitted into the nasal cavity. The sound waves reflected off the evaluated intranasal structures are collected via a microphone and converted into electrical impulses [12]. Subjective recognition of a nasal obstruction is often a complex clinical condition involving mucosal, structural, and even psychological factors. There were discrepancies between the objective test results of the nasal airway evaluation and patientsŌĆÖ subjective symptom complaints. In a previous systematic review, the correlation between the objective measurement outcomes of acoustic rhinometry or rhinomanometry and an individualŌĆÖs subjective sensation of nasal patency remained uncertain [8]. However, in cases of a bilateral assessment, a correlation was found much more often than in a unilateral assessment cases [8]. Therefore, we recommend performing a bilateral nasal assessment including objective measurements such as acoustic rhinometry and sinus endoscopy before performing HRM, regardless of the presence of subjective nasal discomfort in patients with a previous history of sinonasal surgery or nasal disorders. Furthermore, it has been reported that the nasal cavity volumes increase with age, and the nasal cavity volume could be larger in males [12]. Therefore, large population-based studies are warranted to suggest more specific guidance in terms of age and sex for nasal airway evaluation before HRM.
We experienced two cases of failed catheter insertion. In one patient, both nasal airways were severely narrowed on sinus endoscopic evaluation, which did not improve much after treatment with a decongestant. In particular, the anterior nasal airway up to 2 cm from the nostril was fixed in a narrowed condition after treatment with a decongestant. In another patient, the lower nasal bony septum was hypertrophied and deviated on both sides, narrowing the lower anterior nasal airways. Sinus endoscopy demonstrated that although the upper nasal airways were patent on both sides, the lower anterior nasal airway up to 2 cm from the nostril was fixed in a narrowed condition after treatment with a decongestant. The HRM catheter is often inserted and advanced along the nasal floor, which could result in severe patient discomfort. Based on these two cases of failure, we found that fixed narrowed airways up to 2 cm from the nostril could make catheter insertion difficult and result in failure of the procedure.
The risk of adverse events or failure of HRM may be particularly increased in patients with a history of nasal surgery, septal deviation, rhinitis, or obstructive symptoms. As nasal endoscopy is known to be useful in diagnosing and assessing the extent of disease and anatomy of nasal cavity [19], performance of a nasal endoscopic examination might be beneficial in decreasing complications and increasing the satisfaction rate and tolerability of transnasal HRM catheter insertion. To optimize the HRM test, physicians and medical personnel performing HRM should be aware of this potential risk and attempt to minimize it by considering nasal cavity abnormalities.
To our knowledge, this is the first study to evaluate the usefulness of nasal evaluation and pretreatment before HRM. We have suggested the potential usefulness of nasal cavity evaluation in patients presumed to be at high risk of nasal obstruction, such as those with a previous history of nasal surgery or those complaining of subjective nasal discomfort. Catheter insertion was well-tolerated and successful in over 90% of the patients after nasal cavity evaluation and pretreatment and did not cause severe adverse events.
There were some limitations in our study. First, this was a pilot study that included only a small number of subjects, and a comparison with a control group was not conducted. Although we compared the differences in the findings of acoustic rhinometry before and after pretreatment to objectively measure the degree of obstruction, this limits the generalizability of the results of this study. Therefore, the results of this study should be interpreted carefully, and further research is needed to complement these points. Second, we could not clearly suggest risk factors for difficult catheter insertion or determine which patient group requires nasal cavity evaluation before HRM. However, considering that patient-centered care and safety have recently become more important issues, our clinical practice seems to harbor clear implications. It would be not only reasonable but also critical to meticulously evaluate patientsŌĆÖ obstructive symptoms or previous medical histories and to conduct a detailed evaluation before performing a potentially invasive procedure.
In conclusion, to reduce patient discomfort and the risk of adverse events during HRM, a site-specific questionnaire to evaluate for nasal obstruction might be helpful. When subjective discomfort, known nasal structure abnormalities, or a previous history of nasal surgery is confirmed, objective nasal cavity evaluation could be recommended. This practice might enable safe and successful performance of HRM as well as accurate test results; however, this needs to be further verified through a well-designed prospective study in the future.
1. It was useful to use a site-specific questionnaire prior to insertion of HRM catheter, to reduce the risk of adverse events and test failure during HRM.
2. When nasal obstruction is suspected, objective nasal cavity evaluation and decongestant apply could be recommended for the safe and successful execution of HRM.
3. Narrowed nasal airways unresponsive to decongestants could make insertion of the HRM catheter challenging, potentially leading to insertion failure.
Notes
CRedit authorship contributions
Hyun Jin Min: conceptualization, methodology, investigation, data curation, formal analysis, software, writing - original draft, visualization, funding acquisition; Jae Yong Park: conceptualization, methodology, resources, investigation, data curation, writing - original draft, writing - review & editing, supervision, project administration
Figure┬Ā1
Representative findings of sinus endoscopy and acoustic rhinometry in patients with symptom-structure discrepancies. (A) Although subjective nasal discomfort was severe in the right nasal airway, the sinus endoscopy and acoustic rhinometry results showed a narrowed left nasal cavity. It was recommended that the high-resolution esophageal manometry catheter be inserted into the right nasal cavity. (B) Although there was no subjective nasal discomfort, both nasal airways were narrowed based on sinus endoscopy and acoustic rhinometry measurements. (C) Despite moderate nasal discomfort in both nasal airways, both nasal airways were patent based on sinus endoscopy and acoustic rhinometry measurements. VAS, visual analog scale.
Figure┬Ā2
Discrepancy among the results of subjective questionnaires, sinus endoscopy, and acoustic rhinometry. (A) Discrepancy between the results of subjective questionnaires and sinus endoscopy. (B) Discrepancy between the results of sinus endoscopy and acoustic rhinometry.
Figure┬Ā3
Findings of nasal evaluation in two cases of failed catheter insertion. The findings of sinus endoscopy (A) and acoustic rhinometry (B) in a patient with fixed narrowed anterior nasal airways are shown. The findings of sinus endoscopy (C) and acoustic rhinometry (D) in a patient with narrowed lower anterior nasal airways are also shown.
Table┬Ā1
Baseline clinical characteristics of the enrolled patients (n = 22)
Table┬Ā2
Measurement outcomes of acoustic rhinometry
REFERENCES
1. Savarino E, Marabotto E, Bodini G, et al. Advancements in the use of manometry and impedance testing for esophageal functional disorders. Expert Rev Gastroenterol Hepatol 2019;13:425ŌĆō435.


2. Jung HK, Hong SJ, Lee OY, et al.; Korean Society of Neurogastroenterology and Motility. 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil 2020;26:180ŌĆō203.



3. Pauwels A, Boecxstaens V, Andrews CN, et al. How to select patients for antireflux surgery? The ICARUS guidelines (international consensus regarding preoperative examinations and clinical characteristics assessment to select adult patients for antireflux surgery). Gut 2019;68:1928ŌĆō1941.


4. Seo HS, Choi M, Son SY, Kim MG, Han DS, Lee HH. Evidence-based practice guideline for surgical treatment of gastroesophageal reflux disease 2018. J Gastric Cancer 2018;18:313ŌĆō327.




5. van Hoeij FB, Bredenoord AJ. Clinical application of esophageal high-resolution manometry in the diagnosis of esophageal motility disorders. J Neurogastroenterol Motil 2016;22:6ŌĆō13.



6. Carmel Neiderman NN, Eisenberg N, Caspi I, et al. The effect of septal deviation on postoperative quality of life in patients undergoing radiofrequency-assisted turbinate reduction. Laryngoscope Investig Otolaryngol 2022;7:325ŌĆō334.




7. Bredenoord AJ, Hebbard GS. Technical aspects of clinical high-resolution manometry studies. Neurogastroenterol Motil 2012;24:Suppl 1. 5ŌĆō10.


8. Andr├® RF, Vuyk HD, Ahmed A, Graamans K, Nolst Trenit├® GJ. Correlation between subjective and objective evaluation of the nasal airway. A systematic review of the highest level of evidence. Clin Otolaryngol 2009;34:518ŌĆō525.


9. Salihoglu M, Cekin E, Altundag A, Cesmeci E. Examination versus subjective nasal obstruction in the evaluation of the nasal septal deviation. Rhinology 2014;52:122ŌĆō126.


10. Knigge MA, Marvin S, Thibeault SL. Safety and tolerability of pharyngeal high-resolution manometry. Am J Speech Lang Pathol 2019;28:43ŌĆō52.


11. Noh Y, Choi JE, Lee KE, et al. A comparison of olfactory and sinonasal outcomes in endoscopic pituitary surgery performed by a single neurosurgeon or a collaborative team of surgeons. Clin Exp Otorhinolaryngol 2020;13:261ŌĆō267.




12. Krzych-Fa┼éta E, Szcz─Ösnowicz-D─ģbrowska P, Samoli┼äski B, Grzanka A, Wojas O. The normal ranges of selected acoustic rhinometry parameters depending on age and sex-component of standarization in nasal provocation test. Postepy Dermatol Alergol 2022;39:171ŌĆō181.



13. Kahrilas PJ, Bredenoord AJ, Fox M, et al.; International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160ŌĆō174.



14. Jung HJ, Kim JH, Kang MH, Lee DW. Effects of proton pump inhibitor for laryngopharyngeal reflux and comorbid chronic rhinosinusitis. Korean J Otorhinolaryngol-Head Neck Surg 2019;62:165ŌĆō170.


15. Farhood Z, Schlosser RJ, Pearse ME, Storck KA, Nguyen SA, Soler ZM. Twenty-two-item Sino-Nasal Outcome Test in a control population: a cross-sectional study and systematic review. Int Forum Allergy Rhinol 2016;6:271ŌĆō277.


16. Toma S, Hopkins C. Stratification of SNOT-22 scores into mild, moderate or severe and relationship with other subjective instruments. Rhinology 2016;54:129ŌĆō133.


17. Cohen MA, Setzen M, Perlman PW, Ditkoff M, Mattucci KF, Guss J. The safety of flexible endoscopic evaluation of swallowing with sensory testing in an outpatient otolaryngology setting. Laryngoscope 2003;113:21ŌĆō24.


- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print



