A 72-year-old male, who had a 10-year history of end-stage renal disease on hemodialysis, was referred to our clinic due to a migrated stent. In another clinic, percutaneous stenting for central venous occlusion was attempted, but the stent migrated into the right atrium (RA) during the procedure. This case was approved by the Institutional Review Board as exempt (AJOUIRB-EX-2023-302).
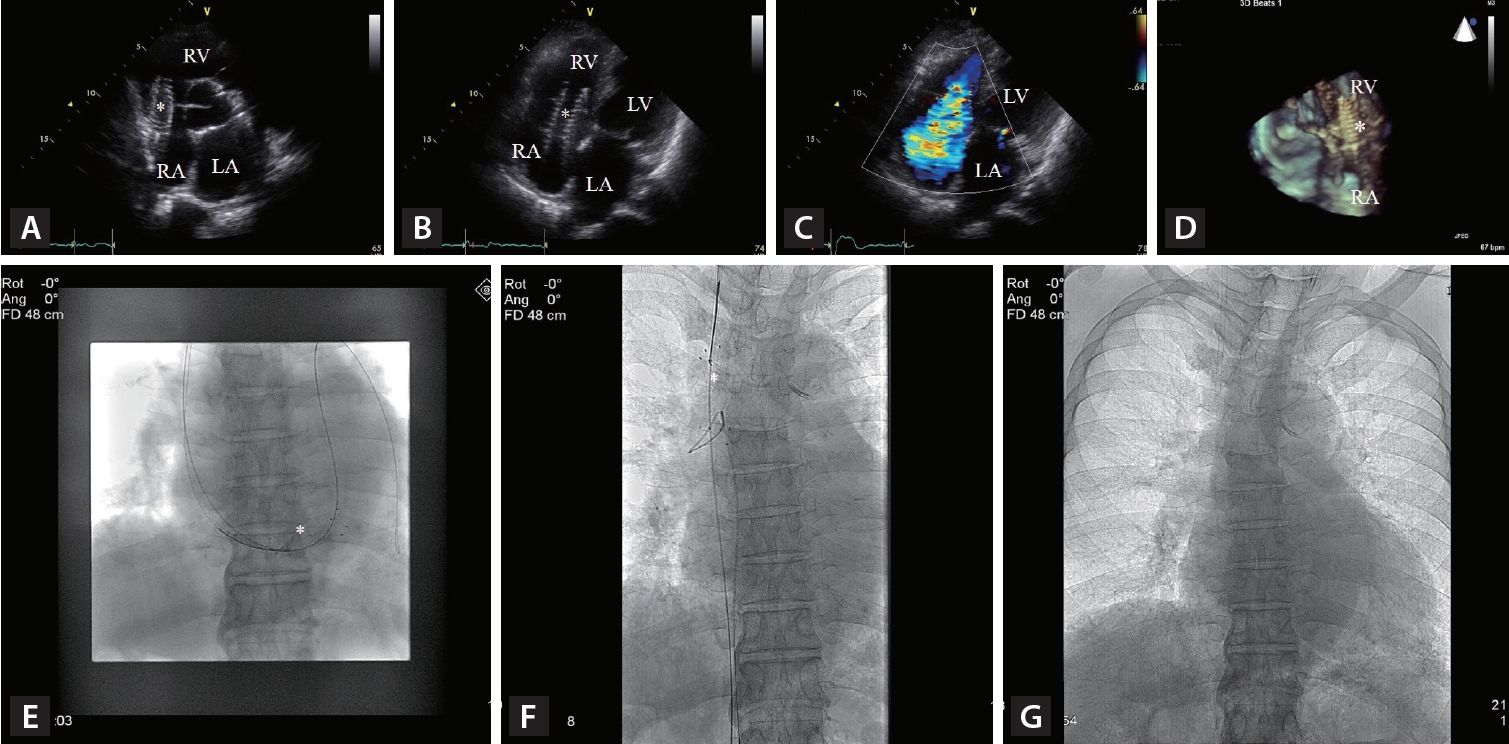
Transthoracic echocardiography revealed that a stent was placed in right heart between RA and right ventricle (Fig. 1A, B). The presence of the stent caused severe functional tricuspid regurgitation (Fig. 1C). The real time three-dimensional echocardiography confirmed the migration of the stent (Fig. 1D).
Percutaneously, an attempt was made to remove the stent. A snare loop was used from right interval jugular vein to capture the stent (Fig. 1E) and pull it out into the superior vena cava (SVC) (Fig. 1F). The stent in the SVC was captured with another snare loop form the right femoral vein and evacuated (Fig. 1F, G). After removal of the stent, transthoracic echocardiography revealed no tricuspid regurgitation or tricuspid valve dysfunction.
Central venous occlusion is a frequent complication in hemodialysis patients [1]. Percutaneous stent placement is known as effective and safe in cases of central venous occlusion [2]. Although stent migration is an extremely rare complication during procedure of percutaneous stent placement, it could result in serious consequences including cardiac perforation, pericardial tamponade, pulmonary embolism, tricuspid regurgitation, and heart failure [3]. In the literature, surgical removal of migrated stent was suggested as the first option for most cases. In the present case, central venous stent migration was successfully resolved by percutaneous stent removal using a snare loop.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





