A 68-year-old woman, who had a 5-year history of end-stage renal disease on hemodialysis through a tunneled hemodialysis catheter (Permcath), was referred to our clinic for aggravating dyspnea and generalized edema. Her Permcath has been replaced several times due to recurrent intraluminal thrombus before admission to our clinic. Last Permcath replacement was performed 2 weeks before admission.
Her blood pressure was 115/90 mmHg, pulse rate 100 beats/minute, respiratory rate 16 breaths/minute, and body temperature 36.5°C. Arterial blood gas analysis results were pH 7.496, pO2 66.6 mmHg, pCO2 32.8 mmHg, and bicarbonate 24.8 mmol/L. Chest radiography showed massive pleural effusion and marked cardiomegaly (Fig. 1A). Echocardiogram revealed large amount of pericardial effusion with diastolic collapse of right ventricle (Fig. 1B). The percutaneous catheter drainage of pleural effusion and pericardiocentesis were performed for symptom relief and fluid analysis. Both drained pleural fluid and pericardial fluid showed milky appearance (Fig. 1C) with elevated triglyceride (1,064 and 1,337 mg/dL, respectively), suggesting chylothorax and chylopericardium.
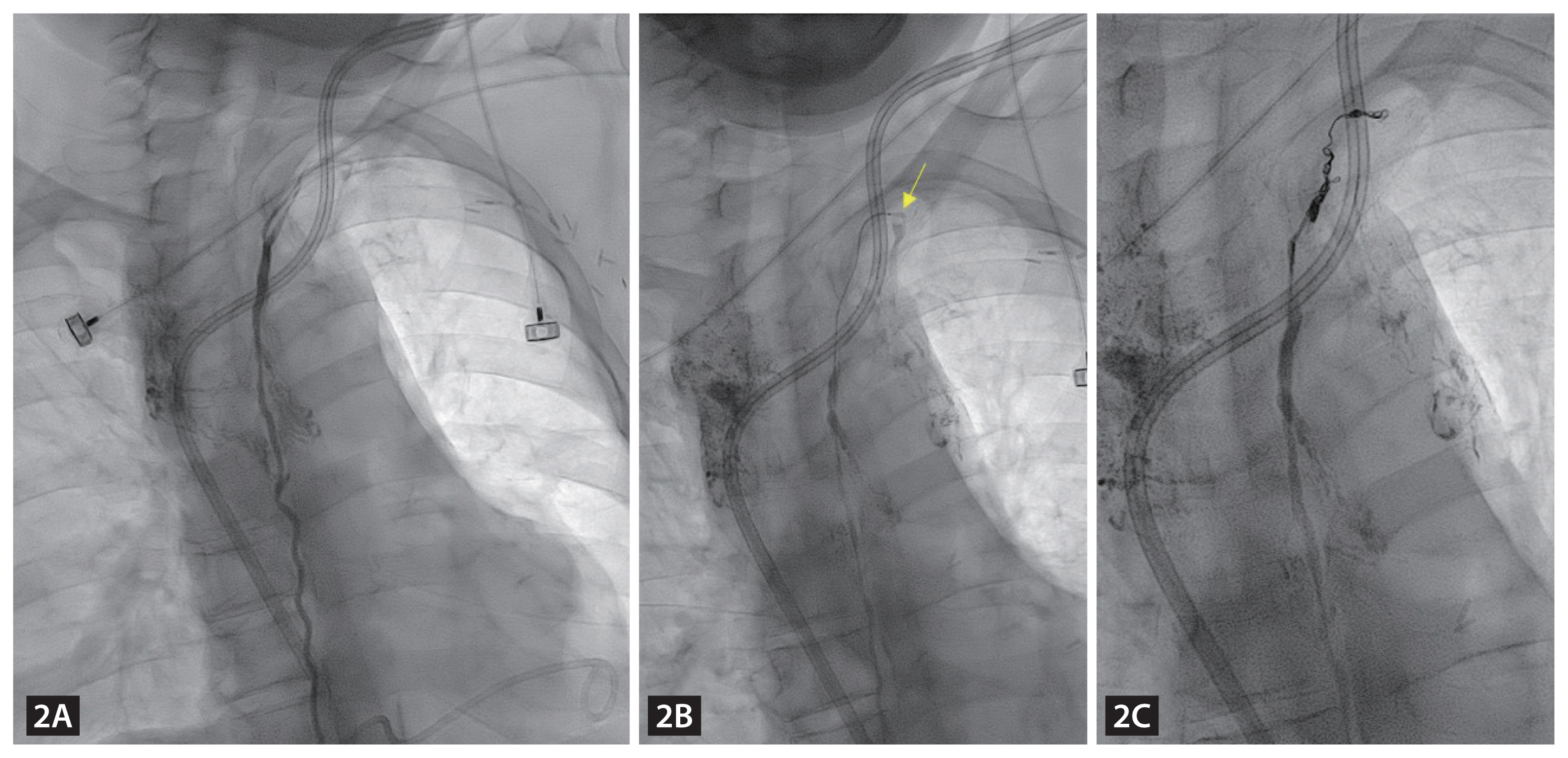
As her symptom aggravated after last Permcath replacement, recurrent Permcath replacement might cause lymphatic injury resulting in chylothorax and chylopericardium. Lymphangiography showed delayed filling of the terminal thoracic duct draining into the left subclavian vein (Fig. 2A, B), suggesting iatrogenic lymphatic injury. After percutaneous catheterization and embolization of thoracic duct using microcoils and glue (Fig. 2B, C), pleural and pericardial fluid turned serous and resolved (Fig. 1D, E).
The development of chylothorax and chylopericardium secondary to iatrogenic lymphatic injury is an extremely rare condition. In the present case, iatrogenic lymphatic injury was successfully resolved by percutaneous catheterization and embolization of the thoracic duct. As central venous access catheters are increasingly used, clinicians should be aware that the development of chylothorax and chylopericardium is a rare but potential complication of central access venous catheters.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





