 |
 |
| Korean J Intern Med > Volume 38(5); 2023 > Article |
|
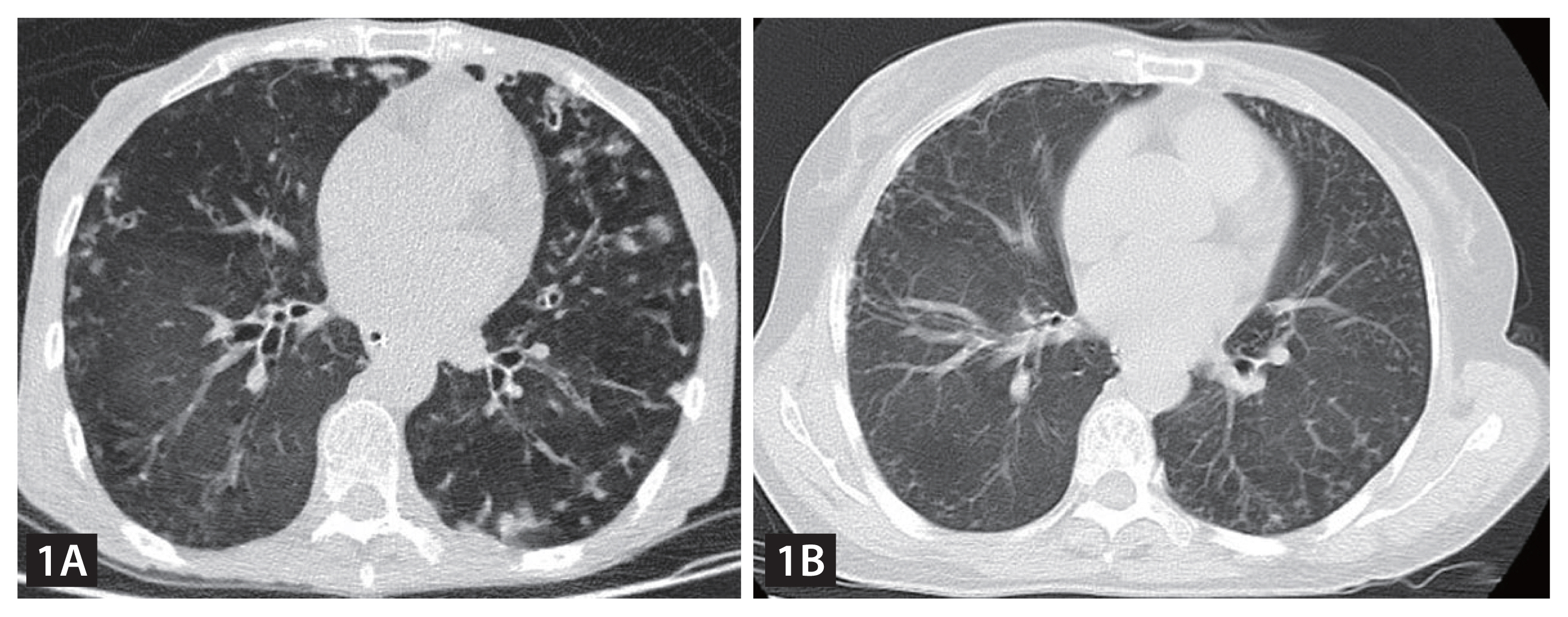
A 62-year-old woman presented with a 3-year history of recurrent wheezing, coughing, sputum production, and 10-kg weight loss. Before this hospitalization, she has had repeated hospital admissions due to the above-mentioned complaint. Skin examination revealed no abnormalities. Pulmonary auscultation revealed bilateral wet rales in the lower lung fields. Laboratory values disclosed neutrophilia (10,610/╬╝L), normocytic anemia (7.9 g/dL), hypoalbuminemia (27.4 g/L) and elevated inflammatory markers (C-reactive protein of 41.98 mg/L), without eosinophilia (390/╬╝L). Chest computed tomography (CT) indicated diffuse lung inflammation (Fig. 1A). She was started on antibiotic therapy, but the condition didnŌĆÖt improve. Due to the history of recurrent unexplained pneumonia and poor response to antibiotic therapy, parasitic infections were suspected. Hence, multiple stool parasite examinations were performed and revealed nematode larvae (Fig. 2A). We also detected nematode larvae in sputum (Fig. 2B, Gram staining) and vomitus specimens (video). Subsequently, strongyloides ELISA blood test was executed and the result was positive. Based on the above findings, the patient was diagnosed with Strongyloides stercoralis hyperinfection syndrome. She was initiated on oral ivermectin at 200 ╬╝g/kg once daily for 6 weeks. Fortunately, her condition gradually improved over the following month. A follow-up chest CT scan showed significant improvement of the lesions (Fig. 1B). No recurrences have been observed during 2 years of follow-up.
Strongyloides stercoralis has the unique ability to replicate within the human host, resulting in a subclinical autoinfection cycle that can persist for decades after exposure [1]. Under some immunocompromised conditions including human immunodeficiency virus infection, immunosuppressive drug, renal transplantations and malnutrition, this can lead to hyperinfection that is characterized by marked increment in the number of worms as well as detection of worms in extraintestinal sites, especially the lungsŌĆöhyperinfection syndrome [2], as seen in our case.
Notes
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 457 View
- 143 Download
- Related articles
-
An unusual cause of a huge abscess in the thigh2024 May;39(3)
An unusual cause of a bronchopleural fistula2023 July;38(4)
A Case of Hyperinfection with Strongyloides Stercoralis in an Immunosuppressed Patient1989 July;4(2)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement video 1
Supplement video 1 Print
Print


