 |
 |
| Korean J Intern Med > Volume 38(3); 2023 > Article |
|
Abstract
Background/Aims
Although a management fee for hospitalist service was established in Korea, the number of hospitalists required for the system to run remains outmatched.
Methods
In January 2020 and February 2022, before and after the establishment of the hospitalist fee system respectively, cross-sectional online surveys were conducted among internal medicine board-certified hospitalists.
Results
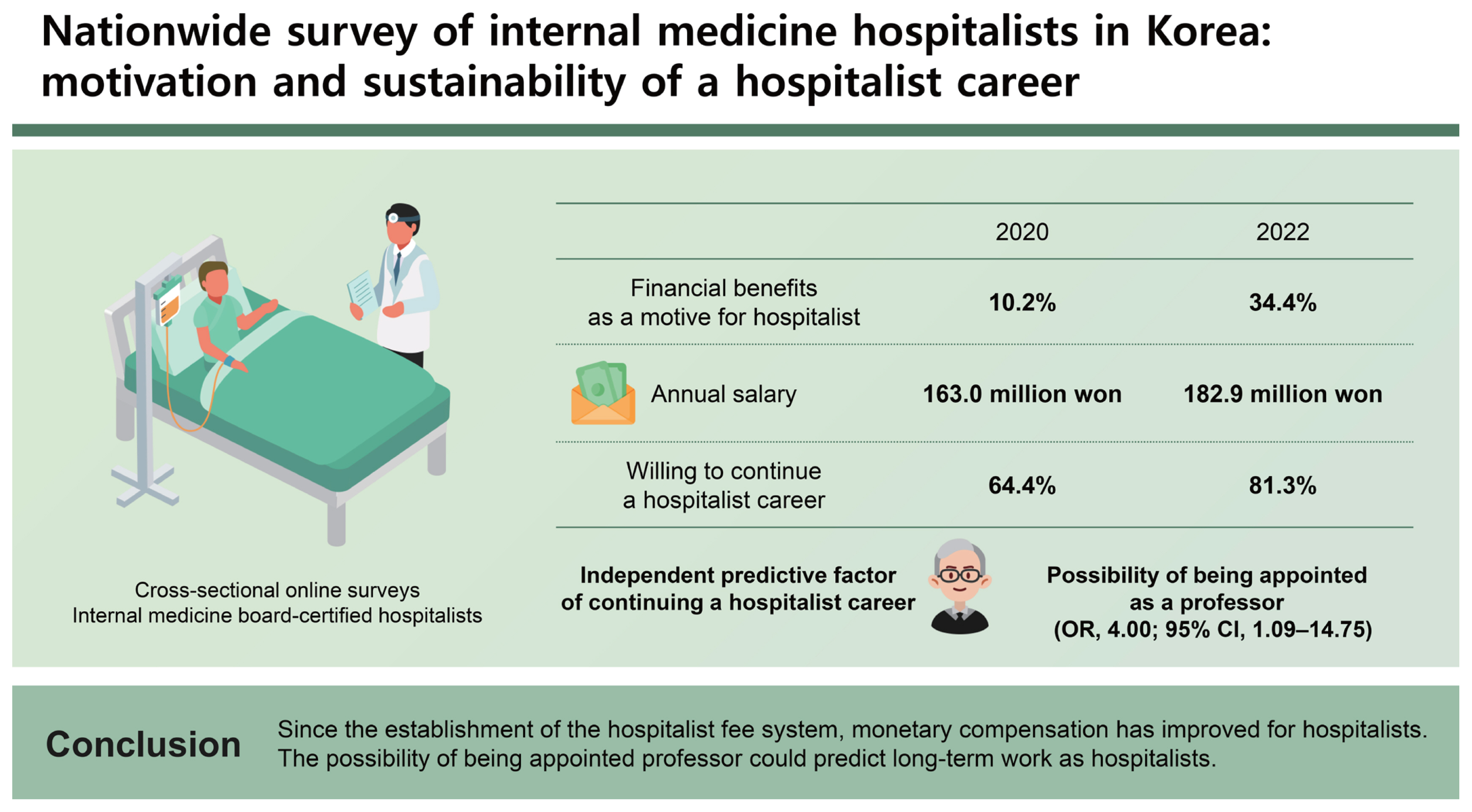
There were 59 and 64 respondents in the 2020 and 2022 surveys, respectively. The percentage of respondents who cited financial benefits as a motive for becoming a hospitalist was higher in the 2022 survey than in the 2020 survey (34.4% vs. 10.2%; p = 0.001). The annual salary of respondents was also higher in the 2022 survey than in the 2020 survey (mean, 182.9 vs. 163.0 million in South Korean Won; p = 0.006). A total of 81.3% of the respondents were willing to continue a hospitalist career in the 2022 survey. In multivariate regression analysis, the possibility of being appointed as a professor was found to be an independent predictive factor of continuing a hospitalist career (odds ratio, 4.00; 95% confidence interval, 1.09ŌĆō14.75; p = 0.037).
In the United States, hospitalists were first introduced in the 1990s to address the efficiency and safety issues of inpatient care [1]. The hospitalist system was already known to improve indicators such as duration of hospital stay, medical costs, patient satisfaction, and even mortality, and has become a larger field than any other division of internal medicine [2ŌĆō5]. Overall, the number of physicians caring for inpatients shrank significantly as a consequence of shortened residency durations from 4 years to 3 years in internal medicine and general surgery, as well as the legislation of resident work hour restriction. To address these issues, the need for the hospitalist system was raised, and in November 2015, a hospitalist pilot program began [6ŌĆō8]. Studies on the pilot program in Korea revealed that patients and nursing staff were highly satisfied with the hospitalist system [9,10]. In addition to the pilot study, studies based on data of Korean hospitals showed that the hospitalist system effectively reduces the duration of stay in the emergency room and that of multimorbid patients with pneumonia or urinary tract infections [11,12]. Differences in clinical results according to the working hours of hospitalists have also been revealed [13].
The hospitalist pilot program ended in January 2021, and a management fee for hospitalist service was established. In other words, the hospitalist system officially took its first official step in Korea. By September 2021, 276 hospitalists were registered nationwide, and this number is expected to increase. However, the number of hospitalists required nationwide was estimated between 2,000 to 6,000, and the number of hospitalists required remains outmatched [14,15]. To expand the hospitalist system, it was necessary to collect and share information on hospitalistsŌĆÖ working conditions. Thus, countrywide surveys were conducted among currently employed hospitalists on behalf of the Korean Society of Hospital Medicine (KSHM).
In January 2020 and February 2022, before and after the establishment of the hospitalist fee system respectively, cross-sectional online surveys were conducted among internal medicine board-certified hospitalists based on the address book of the KSHM. KSHM is an organization established for research and educational activities in the field of hospital medicine with the support of the Korean Association of Internal Medicine. When setting up a new hospitalist model, benchmarking from an already operating hospitalist model is necessary. Most of these processes have been conducted through KSHM members. Membership in KSHM is not compulsory for hospitalists, but the number of members is increasing when fulfilling the aforementioned roles. These surveys were conducted to collect opinions on hospitalist policies among members of the KSHM and to make suggestions to the relevant ministries. At the time of the surveys, only the members working as hospitalists were sent the questionnaire. The surveys included a variety of information, such as age, sex, work experience, hospital location, working hours, the presence of night shifts, contract terms, job satisfaction, and future plans.
The results of the surveys were analyzed and compared according to survey year and willingness to continue a hospitalist career. PearsonŌĆÖs chi-square test or FisherŌĆÖs exact test was used to compare categorical variables, and the Mann-Whitney U test was used to compare all continuous variables that did not follow normal distribution. Backward stepwise regression analysis with a p value threshold of 0.20 was used to identify the predictive factors of willingness to continue a hospitalist career. For statistical analysis, IBM SPSS Statistics for Windows (version 27.0; IBM Corp., Armonk, NY, USA) was used, and p values less than 0.05 were deemed significant.
This study was conducted with the information shared through anonymized online surveys. It did not include information that can identify research subjects, and we did not collect any sensitive information. This study was submitted to the Institutional Review Board of Seoul National University Hospital for review and exempted from approval (E-2209-022-1354).
In 2020 and 2022, 59 and 64 currently working hospitalists, respectively, responded to the survey. The respondentsŌĆÖ age and sex ratios were similar between the two surveys. The length of hospitalist career was significantly longer in the 2022 survey (mean, 2.9 years vs. 2.2 years; p = 0.038). The percentage of people working in the Seoul metropolitan area (including Gyeonggi-do and Incheon) was approximately 75% in both surveys (Table 1).
Some changes were reported in terms of previous careers and motives for becoming hospitalists between the two surveys. The most common occupation, prior to working as a hospitalist, was physicians employed by non-teaching hospitals (30.5%), followed by clinical fellowship training (27.1%) and resident training (16.9%) in the 2020 survey. However, clinical fellowships were the highest previous occupations (29.7%), followed by resident training (23.4%), and specialist staff at teaching hospitals (20.3%) in the 2022 survey. In the 2020 survey, majority of the respondents cited worklife balance as the main motive for becoming a hospitalist (78.0%), followed by social needs for hospitalists (49.2%). The 2022 survey also showed that the majority of the participants cited work-life balance (75.0%), however, only 7.8% cited social needs for hospitalists as the main motive for becoming a hospitalist. The percentage of respondents citing financial benefits as a motive for becoming hospitalists was significantly higher in the 2022 survey than in the 2020 survey (34.4% vs. 10.2%; p = 0.001) (Table 1).
There was a difference in the affiliation of respondents between the two surveys. The proportion of respondents belonging to independent hospitalist departments such as the division of integrated medicine or hospital medicine center increased from 47.5% in 2020 to 60.9% in 2022. As primary care physicians, 49.2% and 64.1% of the respondents had full clinical autonomy in the 2020 and 2022 surveys, respectively. Less than 20% depended on the prescriptions of the existing specialist staff as trainees. Most respondents worked solely during the daytime on weekdays, and the proportion of hospitalists practicing 24/7 was similar in both surveys. The mean working hours of the respondents were 44.2 hours per week in 2020 and 43.0 hours per week in 2022. The majority of the respondents treated 16ŌĆō25 inpatients daily. The proportion of respondents responsible for more than 25 inpatients decreased from 11.9% in 2020 to 3.1% in 2022 (Table 2).
More than 60% of the respondents were 1-year contract workers in both the surveys. The mean annual salary of the respondents was 182.9 million South Korean Won (KRW) in 2022, which was significantly higher than the 163.0 million KRW in 2020 (p = 0.006). The percentage of respondents eligible for salary increases and promotions at the time of contract renewal was significantly higher in the 2022 survey than in the 2020 survey (40.6% vs. 20.3%, p = 0.015; 21.9% vs. 5.1%; p = 0.007, respectively). There were no other significant differences in terms of compensation between the two surveys (Table 3).
In the 2022 survey, the percentage of respondents who played the role of clinician educators was 82.8%, which was significantly higher than 62.7% in the 2020 survey (p = 0.012). More respondents in the 2022 survey (56.3%) than in the 2020 survey (40.7%) tended to be satisfied with the profession of a hospitalist (Table 3).
Regarding their future plans (their plans for the following year), 76.6% respondents of the 2022 survey said that they would continue to work at the same hospital and 4.7% said they would work as a hospitalist in a different hospital. In conclusion, 81.3% of the respondents in the 2022 survey were willing to continue their hospitalist jobs, which was higher than 64.4% in the 2020 survey (p = 0.043) (Table 3).
Among the 90 respondents of both surveys who were willing to continue a hospitalist career, compared to the 33 who were not, the proportion of respondents in the Seoul metropolitan area tended to be higher, and the length of hospitalist careers was significantly longer. The percentage of respondents who answered that they had extra pay for night shifts (37.8% vs. 15.2%, p = 0.017) and private office spaces (70.0% vs. 45.5%, p = 0.012) were significantly higher in the group intending to pursue a hospitalist career. The percentage of respondents who answered that they were enrolled in teachersŌĆÖ pensions (54.4% vs. 27.3%, p = 0.007), had the possibility of being appointed as professors (37.8% vs. 9.1%, p = 0.002), and were serving as clinician educators (80.0% vs. 54.5%, p = 0.005) also were significantly higher in the group that intended to continue their careers as hospitalists. Contrarily, there were no differences regarding age, sex, salary, or work schedule between the two groups (Table 4).
In the unadjusted model, the number of working years as a hospitalist, whether they worked at a hospital in the Seoul metropolitan area, if they received extra pay for night shifts, if they had private office space provision, if they were enrollment in teachersŌĆÖ pension, their possibility of being appointed as a professor, and if they were clinician educators were found to be significant variables. After adjusting for age, sex, and all the variables showing significance in the unadjusted model, the possibility of being appointed as a professor (odds ratio, 4.00; 95% confidence interval, 1.09ŌĆō14.75; p = 0.037) was an independent predictor of continuing a hospitalist career (Table 5).
This is the first survey study conducted on hospitalists in Korea. This study included highly realistic and detailed information about hospitalist compensation and workload, similar to previous studies [16,17]. Because the Korean hospitalist model still has difficulties in recruiting and retaining hospitalists, motivation for choosing a hospitalist job and predictors of hospitalist retention were analyzed.
This study identified differences in responses to various questions depending on the respondentŌĆÖs condition, especially the survey year; that is, whether the hospitalist fee system was settled. In the 2020 survey, before establishing a management fee system for hospitalists, many respondents had worked at a non-teaching local hospitals before choosing a hospitalist career. However, after establishing a hospitalist fee system, there was a marked change in the respondentsŌĆÖ work experience. More doctors chose to have a hospitalist career immediately after residency or fellowship training. It is also worth noting that the proportion of hospitalists who transferred from an academic faculty specialist position rose to 20.3% in the 2022 survey. These changes may be because the settlement of the hospitalist fee system gives applicants a sense of security in their hospitalist careers.
The motives for becoming a hospitalist also differed according to the survey year. In the 2022 survey, after the establishment of a management fee system for hospitalists, 34.4% of respondents cited financial benefits, which was higher than the 10.2% in the 2020 survey. There have been significant changes in terms of monetary compensation between the two survey years. Annual salaries were significantly higher in the 2022 survey than in the 2020 survey. Additionally, the proportion of respondents who could receive a salary increase upon renewing their contract was higher in the 2022 survey. It is known that economic factors are important in the selection of medical specialty [18,19]. The establishment of a fee system for hospitalists encourages hospitals to provide more financial benefits to applicants, and this seems to be a factor that attracts new hospitalists. Also, since the fee system limits working hours and the number of patients, there were a few notable differences between the two survey years.
Regarding non-monetary rewards, the opposite was observed, although it was statistically non-significant. In the 2022 survey, the proportion of respondents who had multiyear contracts, academic attendance expense support, education or research fund support, and the possibility of being appointed as professors tended to be lower than in the 2020 survey. Monetary compensation was not a significant factor for the decision of continuing hospitalist career. It might be because they had started the job after accepting the salary. This study showed that the possibility of being appointed as a professor could predict long-term work as hospitalists. The conditions for a sustainable hospitalist career identified in this study might not be applicable to all hospitalists considering that monetary compensation was cited as an important motive. However, in order for hospitalists to take on an important part of the inpatient care area and to operate stably for a long time, hospitalists that commit to developing educational roles and leadership are needed [20ŌĆō22]. Previous reports suggested that hospitalist clinician educators were helpful not only for clinical outcomes but also for resident education and for the maintenance of a hospitalist career [23,24]. Some studies suggested that hospitalists can be better educators than traditional physicians [25,26]. It is also noteworthy that the proportion of respondents who had full clinical autonomy and independent hospitalist departments tended to show higher interest in the continuing their hospitalist career. In the United States, where the hospitalist system is well established, a report showed that the proportion of hospitalists with clinical autonomy reached 97.1% [27].
The establishment of the hospitalist fee system has forced many hospitals to hire hospitalists, meanwhile financial benefits are becoming the main motivation for choosing a hospitalist career. However, with this trend, the executives of hospitals expect hospitalists to handle the maximum workload based on their pay. This perception may adversely affect the hospitalists in establishing well-functioning positions in hospitals. Hospitalists who want to work for a long time do not earn a higher salary, but rather serve educational roles and prepare for appointments as professors. From a longterm perspective, hospitalists should not be a high-paying job that takes the place of resident doctors. Instead, they must become experts in inpatient care and clinical education. Considering that most hospitalists are currently working in tertiary general hospitals in educational roles, it can be said that this may not apply to most hospitalists in the future. However, for the hospitalist model to spread to local secondary hospitals in need, it is necessary to motivate those who were committed in the early stages of the hospitalist system introduction to become pioneers.
There are some limitations to this study. First, the number of participants was small. It was difficult to secure a larger number of respondents due to the small population of hospitalists in Korea and to the voluntary participation to the surveys. Thus, these results might not fully reflect the opinions of all hospitalists in Korea. Second, because the surveys were conducted with a small pool of respondents, it is possible that the same person was included in the two surveys. However, even the same person may have responded differently in the two surveys, considering that most of respondents were 1-year contract workers. It is also meaningful to show the changes before and after the establishment of the hospitalist fee system, even for the same person. Third, only internal medicine hospitalists were included in the surveys. The authors believe that there could be considerable differences in the settings and attitudes toward the hospitalist system by department. Large-scale studies including other specialty hospitalists or in-depth qualitative researches should be undertaken in future.
Since the establishment of the hospitalist fee system, monetary compensation has improved for hospitalists. The possibility of being appointed as a professor was an independent predictor of continuing a hospitalist career. We hope that this study will facilitate the recruitment and retention of hospitalists, lead to the expansion of the hospitalist system, and ultimately serve as a reference for policies regarding hospitalists.
1. Hospitalists of the recent survey tend to value financial benefits.
2. Since the official establishment of hospitalist fee system, monetary compensation has improved for hospitalists.
3. The possibility of being appointed as a professor was an independent predictor of continuing a hospitalist career.
Notes
CRedit authorship contributions
Seung Jun Han: conceptualization, formal analysis, methodology, writing - original draft; Dong-Ho Shin: funding acquisition, methodology, writing - original draft, writing - review & editing; Nak-Hyun Kim: writing - original draft, writing - review & editing; Eun Sun Kim: data curation, formal analysis; Junhwan Kim: conceptualization, data curation; Hye Won Kim: data curation, formal analysis; Sung do Moon: conceptualization, data curation; Sang Wook Park: data curation, formal analysis; Jung Hun Ohn: conceptualization, methodology; Chang-Yun Woo: data curation, visualization; Ki Byung Lee: data curation, methodology; Jae Hyun Lee: data curation, formal analysis; Han Sung Lee: data curation, funding acquisition; Yejee Lim: conceptualization, funding acquisition; Seungha Hwang: conceptualization, project administration
Table┬Ā1
Comparison of basic information by survey year
| Variable | 2020 respondents (n = 59) | 2022 respondents (n = 64) | p value |
|---|---|---|---|
| Age, yr | 39 (37ŌĆō42) | 39.5 (36ŌĆō42) | 0.749 |
| Male | 29 (49.2) | 34 (53.1) | 0.660 |
| Length of hospitalist career, yr | 2.2 ┬▒ 1.3 | 2.9 ┬▒ 1.8 | 0.038 |
| Hospital at Seoul metropolitan area | 44 (74.5) | 51 (79.7) | 0.499 |
| Practicing at the previously trained hospital | 39 (66.1) | 39 (60.9) | 0.552 |
| Career before current hospitalist job | 0.237 | ||
| ŌĆāPhysicians at a non-teaching hospital | 18 (30.5) | 10 (15.6) | |
| ŌĆāClinical fellowship training | 16 (27.1) | 19 (29.7) | |
| ŌĆāResident training | 10 (16.9) | 15 (23.4) | |
| ŌĆāSpecialist staff at a teaching hospital | 11 (18.6) | 13 (20.3) | |
| ŌĆāOthers | 4 (6.8) | 2 (3.2) | |
| ŌĆāHospitalist at a different hospital | 0 (0) | 5 (7.8) | |
| Motives for becoming a hospitalist; multiple selection up to three answers | |||
| ŌĆāWork-life balance | 46 (78.0) | 48 (75.0) | 0.699 |
| ŌĆāSocial needs for the hospitalist | 29 (49.2) | 5 (7.8) | < 0.001 |
| ŌĆāProviding the best patients-centered care | 24 (40.7) | 28 (43.8) | 0.730 |
| ŌĆāManagementŌĆÖs commitment to the hospitalist system | 18 (30.5) | 15 (23.4) | 0.377 |
| ŌĆāLight burden of medical revenue | 9 (15.3) | 20 (31.3) | 0.055a |
| ŌĆāRecognition of social status | 6 (10.2) | 12 (18.8) | 0.179 |
| ŌĆāFinancial benefits | 6 (10.2) | 22 (34.4) | 0.001 |
| ŌĆāResearch or educational opportunity | 4 (6.8) | 4 (6.3) | 0.905 |
Table┬Ā2
Comparison of the hospitalist operating model by survey year
Table┬Ā3
Comparison of contract conditions, job satisfaction and future plans by survey year
| Variable | 2020 respondents (n = 59) | 2022 respondents (n = 64) | p value |
|---|---|---|---|
| Contract conditions | |||
| ŌĆāContract period, yr | 0.647 | ||
| ŌĆāŌĆā1 | 36 (61.0) | 44 (68.8) | |
| ŌĆāŌĆā2 | 18 (30.5) | 15 (23.4) | |
| ŌĆāŌĆāMore than 2 | 5 (8.5) | 10 (8.1) | |
| ŌĆāAnnual salary, million in South Korean Won | 163.0 ┬▒ 28.3 | 182.9 ┬▒ 39.4 | 0.006 |
| ŌĆāSalary increase at a renewal of contract | 12 (20.3) | 26 (40.6) | 0.015 |
| ŌĆāPromotion system | 3 (5.1) | 14 (21.9) | 0.007 |
| ŌĆāExtra pay for night shift | 14 (23.7) | 25 (39.1) | 0.068 |
| ŌĆāIncentive compensation | 12 (20.3) | 20 (31.3) | 0.168 |
| ŌĆāAcademic attendance expenses support | 36 (61.0) | 34 (53.1) | 0.377 |
| ŌĆāEducation or research fund support | 26 (44.1) | 18 (28.1) | 0.065 |
| ŌĆāPrivate office space provision | 37 (62.7) | 41 (64.1) | 0.877 |
| ŌĆāBeing enrolled in teachersŌĆÖ pension | 25 (42.4) | 33 (51.6) | 0.308 |
| ŌĆāPossibility of being appointed as a professor | 19 (32.2) | 18 (28.1) | 0.622 |
| Job satisfaction | |||
| ŌĆāOpportunity to be educated | 28 (47.5) | 21 (32.8) | 0.097 |
| ŌĆāRole as a clinician educator for | 37 (62.7) | 53 (82.8) | 0.012 |
| ŌĆāŌĆāResident doctor | 23 (39.0) | 31 (48.4) | 0.291 |
| ŌĆāŌĆāIntern doctor | 14 (23.7) | 28 (43.8) | 0.019 |
| ŌĆāŌĆāStudent | 17 (28.8) | 16 (25.0) | 0.633 |
| ŌĆāŌĆāNurse | 22 (37.3) | 16 (25.0) | 0.141 |
| ŌĆāHope to be a clinician educator | 24 (40.7) | 32 (50.0) | 0.300 |
| ŌĆāSatisfaction with monetary compensation | 19 (32.2) | 18 (28.1) | 0.622 |
| ŌĆāSatisfaction with non-monetary compensation | 11 (18.6) | 15 (23.4) | 0.515 |
| ŌĆāOverall job satisfaction | 24 (40.7) | 36 (56.3) | 0.084 |
| Next year plan | |||
| ŌĆāContinue a hospitalist career | 38 (64.4) | 52 (81.3) | 0.043a |
| ŌĆāNo answer or quitting | 21 (35.6) | 12 (18.8) | |
Table┬Ā4
Comparison of variables according to willingness to continue a hospitalist career
| Variable | To continue (n = 90) | Not to continue (n = 33) | p value |
|---|---|---|---|
| Age, yr | 39.5 (36ŌĆō42) | 39 (37ŌĆō42) | 0.826 |
| Male | 47 (52.2) | 16 (48.5) | 0.713 |
| Length of hospitalist career | 2.8 ┬▒ 1.7 | 2.0 ┬▒ 1.3 | 0.032 |
| Hospital at Seoul metropolitan area | 74 (82.2) | 21 (63.6) | 0.050 |
| Practicing at the previously trained hospital | 57 (63.3) | 21 (63.6) | 0.975 |
| Independent hospitalist department | 54 (60.0) | 13 (39.4) | 0.065a |
| Full clinical autonomy | 56 (62.2) | 14 (42.4) | 0.065a |
| Working on only weekdays | 41 (45.6) | 19 (57.6) | 0.237 |
| Working day and night shifts (24/7 coverage) | 33 (36.7) | 8 (24.2) | 0.195 |
| Working hours per week, hours | 43.5 ┬▒ 7.2 | 43.7 ┬▒ 11.0 | 0.321 |
| More than 25 responsible patients | 6 (6.7) | 3 (9.1) | 0.054 |
| Coworkers in hospitalist unit | |||
| ŌĆāIntern doctors | 50 (55.6) | 13 (39.4) | 0.112 |
| ŌĆāResident doctors | 22 (24.4) | 10 (30.3) | 0.512 |
| ŌĆāPhysician assistants | 42 (46.7) | 16 (48.5) | 0.858 |
| Multi-year contract | 35 (38.9) | 8 (24.2) | 0.131 |
| Annual salary, million KRW | 174.8 ┬▒ 32.0 | 169.5 ┬▒ 45.4 | 0.250 |
| Salary increase at a renewal of contract | 30 (33.3) | 8 (24.2) | 0.334 |
| Promotion system | 14 (15.6) | 3 (9.1) | 0.357 |
| Extra pay for night shifts | 34 (37.8) | 5 (15.2) | 0.017 |
| Incentive compensation | 27 (30.0) | 5 (15.2) | 0.096 |
| Academic attendance expenses support | 56 (62.2) | 14 (42.4) | 0.065a |
| Education or research fund support | 34 (37.8) | 10 (30.3) | 0.444 |
| Private office space provision | 63 (70.0) | 15 (45.5) | 0.012 |
| Being enrolled in teachersŌĆÖ pension | 49 (54.4) | 9 (27.3) | 0.007 |
| Possibility of being appointed as a professor | 34 (37.8) | 3 (9.1) | 0.002 |
| Opportunity to be educated | 38 (42.2) | 11 (33.3) | 0.372 |
| Role as a clinician educator | 72 (80.0) | 18 (54.5) | 0.005 |
Table┬Ā5
Predictive factors for willingness to continue a hospitalist career
REFERENCES
2. Salim SA, Elmaraezy A, Pamarthy A, Thongprayoon C, Cheungpasitporn W, Palabindala V. Impact of hospitalists on the efficiency of inpatient care and patient satisfaction: a systematic review and meta-analysis. J Community Hosp Intern Med Perspect 2019;9:121ŌĆō134.



3. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med 2016;375:1009ŌĆō1011.


4. Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med 2007;357:2589ŌĆō2600.


5. Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med 2002;137:866ŌĆō874.


6. Jeon B, Kwon S. Health and long-term care systems for older people in the Republic of Korea: policy challenges and lessons. Health Syst Reform 2017;3:214ŌĆō223.



8. Jang SI, Jang SY, Park EC. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med 2015;89:1ŌĆō5.


9. Chae W, Choi DW, Park EC, Jang SI. Improved inpatient care through greater patient-doctor contact under the hospitalist management approach: a real-time assessment. Int J Environ Res Public Health 2021;18:5718.



10. Chae W, Kim J, Park EC, Jang SI. Comparison of patient satisfaction in inpatient care provided by hospitalists and nonhospitalists in South Korea. Int J Environ Res Public Health 2021;18:8101.



11. Lee JH, Kim AJ, Kyong TY, et al. Evaluating the outcome of multi-morbid patients cared for by hospitalists: a report of integrated medical model in Korea. J Korean Med Sci 2019;34:e179.




12. Ohn JH, Kim NH, Kim ES, et al. An acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci 2017;32:1917ŌĆō1920.




13. Han SJ, Jung HW, Oh DY, et al. Comparisons of clinical outcomes between weekday-only and full-time, 24-hour/7-day coverage hospitalist systems. J Korean Med Sci 2020;35:e117.




16. Michtalik HJ, Yeh HC, Pronovost PJ, Brotman DJ. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med 2013;173:375ŌĆō377.


17. Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med 1999;130:343ŌĆō349.


18. Thornton J, Esposto F. How important are economic factors in choice of medical specialty? Health Econ 2003;12:67ŌĆō73.


19. Thornton J. Physician choice of medical specialty: do economic incentives matter? Appl Econ 2000;32:1419ŌĆō1428.

21. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med 2011;6:5ŌĆō9.



22. Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med 2001;161:851ŌĆō858.


23. Natarajan P, Ranji SR, Auerbach AD, Hauer KE. Effect of hospitalist attending physicians on trainee educational experiences: a systematic review. J Hosp Med 2009;4:490ŌĆō498.



24. Kulaga ME, Charney P, OŌĆÖMahony SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med 2004;19:293ŌĆō301.



25. Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. Resident satisfaction on an academic hospitalist service: time to teach. Am J Med 2002;112:597ŌĆō601.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



