 |
 |
| Korean J Intern Med > Volume 37(4); 2022 > Article |
|
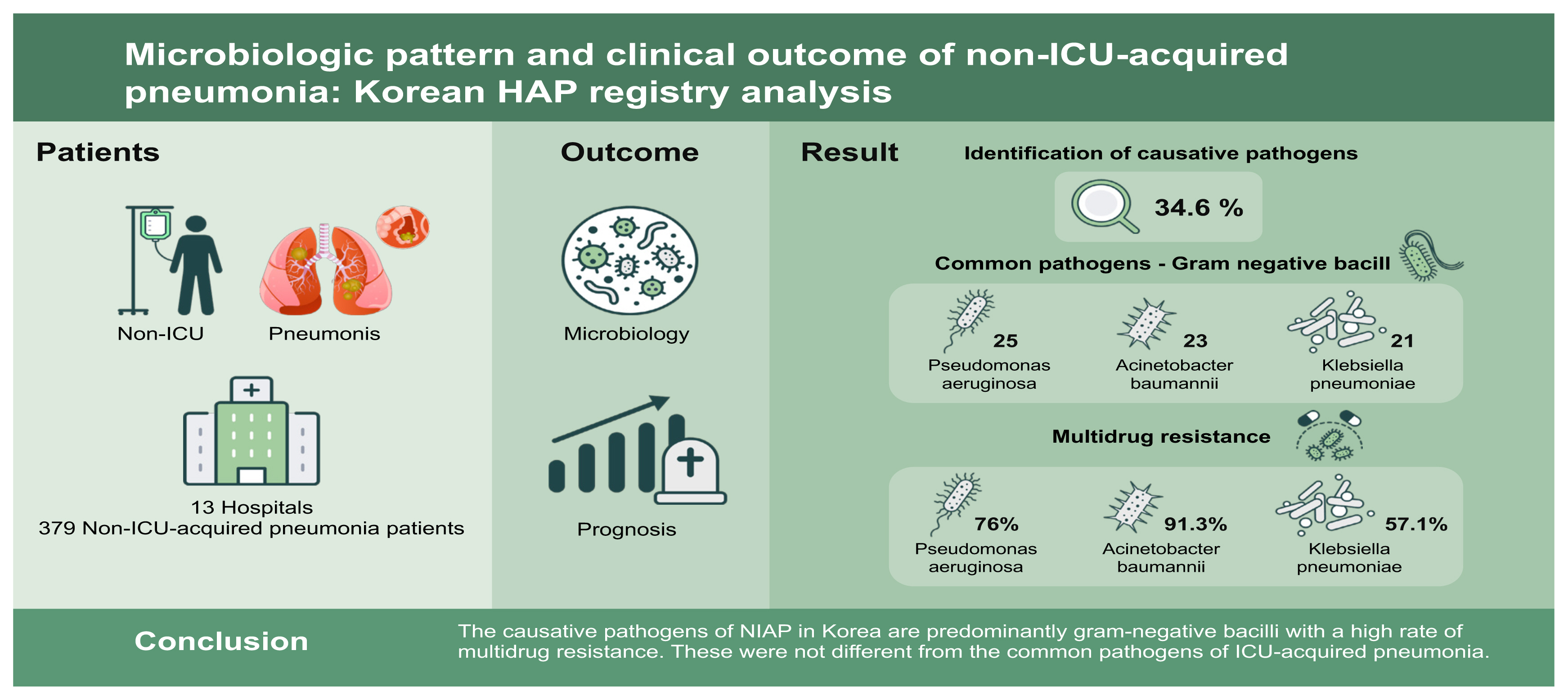
Abstract
Background/Aims
Methods
Results
Acknowledgments
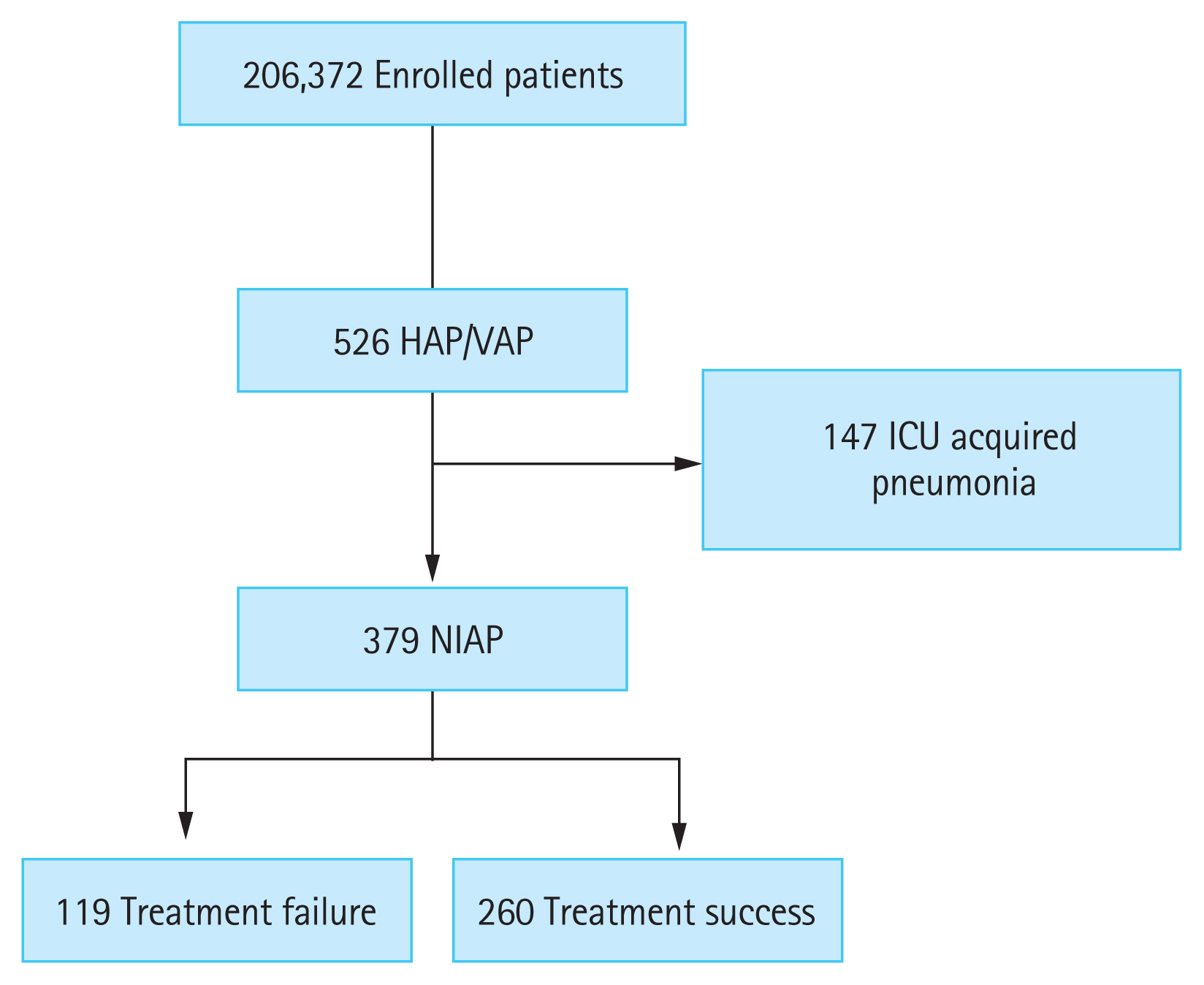
Figure┬Ā1
Table┬Ā1
| Variable | Overall (n = 379) | Treatment failure (n = 119) | Treatment success (n = 260) |
|---|---|---|---|
| Age, yr | 71.0 ┬▒ 12.6 | 72.0 ┬▒ 13.1 | 70.5 ┬▒ 12.3 |
| Male sex | 267 (70.4) | 84 (70.6) | 183 (70.4) |
| BMI, kg/m2 | 21.9 ┬▒ 3.8 | 21.9 ┬▒ 3.7 | 21.9 ┬▒ 3.9 |
| Initial SOFA score | 4.0 ┬▒ 3.3 | 5.7 ┬▒ 3.5c | 3.2 ┬▒ 2.8 |
| ŌĆāCharlson comorbidity index | 5.0 ┬▒ 2.6 | 5.6 ┬▒ 2.3c | 4.7 ┬▒2.6 |
| ŌĆāComorbidities | |||
| ŌĆāCardiovascular disease | 65 (17.2) | 19 (16.0) | 46 (17.7) |
| ŌĆāChronic lung disease | 63 (16.6) | 19 (16.0) | 44 (16.9) |
| ŌĆāChronic neurological disease | 97 (25.6) | 33 (27.7) | 64 (24.6) |
| ŌĆāChronic kidney disease | 47 (12.4) | 18 (15.1) | 29 (11.2) |
| ŌĆāChronic liver disease | 21 (5.5) | 6 (5.0) | 15 (5.8) |
| ŌĆāDiabetes mellitus | 112 (29.6) | 32 (26.9) | 80 (30.8) |
| ŌĆāConnective tissue disease | 6 (1.6) | 2 (1.7) | 4 (1.5) |
| ŌĆāImmunocompromisedd | 20 (5.3) | 12 (10.1) | 8 (3.1)b |
| ŌĆāHematological malignancies | 36 (9.5) | 22 (18.5) | 14 (5.4)c |
| ŌĆāSolid malignant tumors | 159 (42.0) | 55 (46.2) | 104 (40.0) |
| ŌĆāHigh-dose or long-term corticosteroid usee | 22 (5.8) | 11 (9.2) | 11 (4.2) |
| Presence of artificial airwayf | 41 (10.8) | 8 (6.7) | 33 (12.7) |
| Risk of aspirationg | 199 (52.5) | 72 (60.5) | 127 (48.8)a |
| Sepsis | 219 (57.8) | 86 (72.3) | 133 (51.2)c |
| Septic shock | 25 (6.6) | 15 (12.6) | 10 (3.8)b |
| Prior IV antibiotics use within 90 days | 260 (68.6) | 92 (77.3) | 168 (65.6)b |
| Reason for admissionb | |||
| ŌĆāMedical for diagnostic work up | 42 (11.1) | 11 (9.2) | 31 (11.9) |
| ŌĆāMedical disease treatment | 223 (58.8) | 86 (72.3) | 137 (52.7) |
| ŌĆāSurgical for elective operation | 86 (22.7) | 13 (10.9) | 73 (28.1) |
| ŌĆāSurgical for emergency operation | 18 (4.7) | 5 (4.2) | 13 (5.0) |
| ŌĆāSurgical for other reasons than operation | 10 (2.6) | 4 (3.4) | 6 (2.3) |
Table┬Ā2
| Causative pathogens | Overall (n = 379) | Treatment failure (n = 119) | Treatment success (n = 260) |
|---|---|---|---|
| Unknown | 248 (65.4) | 61 (51.3) | 187 (71.9)c |
| Bacteria | 113 (29.8) | 49 (41.2) | 64 (24.6)c |
| ŌĆāEnterobacteriaceaed | 44 (11.6) | 20 (16.8) | 24 (9.2)a |
| ŌĆāŌĆāEscherichia coli | 6 (1.6) | 3 (2.5) | 3 (1.2) |
| ŌĆāŌĆāKlebsiella pneumoniae | 21 (5.5) | 11 (9.2) | 10 (3.8)a |
| ŌĆāŌĆāMDR Enterobacteriaceae | 18 (4.7) | 7 (5.9) | 11 (4.2) |
| ŌĆāAcinetobacter baumannii | 23 (6.1) | 13 (10.9) | 10 (3.8)b |
| ŌĆāŌĆāMDR Acinetobacter spp. | 21 (5.5) | 11 (9.2) | 10 (3.8)a |
| ŌĆāPseudomonas aeruginosa | 25 (6.6) | 7 (5.9) | 18 (6.9) |
| ŌĆāŌĆāMDR P. aeruginosa | 19 (5.0) | 6 (5.0) | 13 (5.0) |
| ŌĆāStaphylococcus aureus | 14 (3.7) | 5 (4.2) | 9 (3.5) |
| ŌĆāŌĆāMRSA | 11 (2.9) | 4 (3.4) | 7 (2.7) |
| ŌĆāEnterococcus spp. | 4 (1.1) | 2 (1.7) | 2 (0.8) |
| ŌĆāŌĆāMDR Enterococcus spp. | 3 (0.8) | 1 (0.8) | 2 (0.8) |
| ŌĆāOther bacteriae | 27 (7.1) | 8 (6.7) | 19 (7.3) |
| ŌĆāPolymicrobial infection | 19 (5.0) | 4 (3.4) | 15 (5.8) |
| Detection of RV by PCR | 20 (5.3) | 12 (10.1) | 8 (3.1)b |
| ŌĆāParainfluenza virus | 8 (2.1) | 5 (4.2) | 3 (1.2) |
| ŌĆāHuman coronavirus OC43 | 2 (0.5) | 1 (0.8) | 1 (0.4) |
| ŌĆāInfluenza A virus | 3 (0.8) | 1 (0.8) | 2 (0.8) |
| ŌĆāAdenovirus | 3 (0.8) | 2 (1.7) | 1 (0.4) |
| ŌĆāRespiratory syncytial virus | 2 (0.5) | 1 (0.8) | 1 (0.4) |
| ŌĆāRhinovirus | 3 (0.8) | 3 (2.5) | 0a |
| ŌĆāHuman bocavirus | 1 (0.3) | 0 | 1 (0.4) |
| Serologic tests for atypical pathogens | 7 (1.8) | 5 (4.2) | 2 (0.8) |
| ŌĆāCytomegalovirus | 1 (0.3) | 1 (0.8) | 0 |
| ŌĆāAspergillus spp. | 2 (0.5) | 1 (0.8) | 1 (0.4) |
| ŌĆāMycoplasma pneumoniae | 1 (0.3) | 1 (0.8) | 0 |
| ŌĆāPneumocystis jirovecii | 3 (0.8) | 2 (1.7) | 1 (0.4) |
Values are presented as number (%). MDR pathogens are defined as microorganisms that are resistant to agents from three or more antimicrobial categories.
ICU, intensive care unit; MDR, multi-drug resistant; MRSA, methicillin-resistant Staphylococcus aureus; RV, respiratory virus; PCR, polymerase chain reaction.
Table┬Ā3
| Initial empiric antibiotics for NIAP | Overall (n = 379) | Treatment failure (n = 119) | Treatment success (n = 260) |
|---|---|---|---|
| Monotherapy | 192 (50.7) | 53 (44.5) | 139 (53.5) |
| ŌĆāB-lactam antibiotics | 177 (46.7) | 50 (42.0) | 127 (48.8) |
| ŌĆāFluoroquinolones | 6 (1.6) | 0 | 6 (1.6) |
| ŌĆāGlycopeptides | 1 (0.3) | 0 | 1 (0.4) |
| ŌĆāAminoglycosides | 2 (0.5) | 0 | 2 (0.8) |
| ŌĆāMiscellaneous | 6 (1.6) | 3 (2.5) | 3 (1.2) |
| Dual combination therapy | 161 (42.5) | 52 (43.7) | 109 (41.9) |
| ŌĆāB-lactam + Fluoroquinolones | 114 (30.1) | 29 (24.4) | 85 (32.7) |
| ŌĆāB-lactam + Glycopeptides | 28 (7.4) | 13 (10.9) | 15 (5.8) |
| ŌĆāB-lactam + Aminoglycosides | 5 (1.3) | 3 (2.5) | 2 (0.8) |
| ŌĆāB-lactam + Nitroimidazoles | 5 (1.3) | 3 (2.5) | 2 (0.8) |
| ŌĆāB-lactam + Macrolides | 7 (1.8) | 2 (1.7) | 5 (1.9) |
| ŌĆāMiscellaneous | 4 (1.1) | 2 (1.7) | 2 (0.8) |
| Triple combination therapy | 21 (5.5) | 11 (9.2)a | 10 (3.8) |
| ŌĆāB-lactam + Fluoroquinolones + Glycopeptides | 10 (2.6) | 6 (5.0) | 4 (1.5) |
| ŌĆāB-lactam + Fluoroquinolones + Nitroimidazoles | 2 (0.5) | 1 (0.8) | 1 (0.4) |
| ŌĆāB-lactam + Aminoglycosides + Glycopeptides | 1 (0.3) | 1 (0.8) | 0 |
| ŌĆāB-lactam + Aminoglycosides + Nitroimidazoles | 1 (0.3) | 0 | 1 (0.4) |
| ŌĆāMiscellaneous | 7 (1.8) | 3 (2.5) | 4 (1.5) |
| Duration of antibiotics, day | 12 (7ŌĆō24) | 10 (5ŌĆō25) | 12 (7ŌĆō22) |
| Adequacy of initial antibioticsc | 57 (55.9) | 25 (55.6) | 32 (56.1) |
| Change of antibiotics after pathogen confirm | 132 (34.8) | 51 (42.9)a | 81 (31.2) |
| ŌĆāEscalation of antibiotics | 75 (56.4) | 33 (63.5) | 42 (51.9) |
| ŌĆāDe-escalation of antibiotics | 24 (18.0) | 6 (11.5) | 18 (22.2) |
| Adjunctive corticosteroid treatment | 63 (16.6) | 29 (24.4) | 34 (13.1)b |
Table┬Ā4
| Variable | Overall (n = 379) | Treatment failure (n = 119) | Treatment success (n = 260) |
|---|---|---|---|
| Microbiologic responsec | |||
| ŌĆāEradicationd | 56 (14.8) | 15 (35.7) | 41 (80.4)b |
| ŌĆāColonizatione | 7 (1.8) | 0 | 7 (13.7)a |
| ŌĆāFailuref | 29 (7.7) | 26 (61.9) | 3 (5.9)b |
| ŌĆāRecurrenceg | 1 (2.6) | 1 (2.4) | 0 |
| Hospital length of stay, day | 29 (17ŌĆō51) | 32 (18ŌĆō63) | 28 (16ŌĆō47) |
| Additional ICU admission associated with HAP | 107 (28.2) | 60 (50.4) | 47 (18.1)b |
| Survival discharge | 276 (72.8) | 25 (21.0) | 251 (96.5)b |
| ŌĆāHome discharge | 170 (44.9) | 6 (24.0) | 164 (65.3)b |
| ŌĆāStep down referral | 97 (25.6) | 16 (64.0) | 81 (32.3) |
| ŌĆāStep up referral | 9 (2.4) | 3 (12.0) | 6 (2.4) |
Table┬Ā5
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Initial SOFA score | 1.27 (1.18ŌĆō1.36) | < 0.001 | 1.24 (1.14ŌĆō1.34) | < 0.001 |
|
|
||||
| CCI | 1.15 (1.05ŌĆō1.25) | 0.002 | 1.12 (1.00ŌĆō1.24) | 0.036 |
|
|
||||
| Immunocompromiseda | 3.53 (1.40ŌĆō8.89) | 0.007 | ||
|
|
||||
| Hematologic malignancies | 3.99 (1.96ŌĆō8.11) | < 0.001 | 3.54 (1.57ŌĆō8.00) | 0.002 |
|
|
||||
| Risk of aspirationb | 1.60 (1.03ŌĆō2.49) | 0.036 | ||
|
|
||||
| Prior IV antibiotics use within 90 days | 1.79 (1.08ŌĆō2.94) | 0.023 | ||
|
|
||||
| Sepsis | 2.49 (1.56ŌĆō4.00) | < 0.001 | ||
|
|
||||
| Septic shock | 3.61 (1.57ŌĆō8.29) | 0.003 | ||
|
|
||||
| Klebsiella pneumoniae | 2.55 (1.05ŌĆō6.17) | 0.039 | 3.50 (1.35ŌĆō9.05) | 0.010 |
|
|
||||
| Acinetobacter baumannii | 3.07 (1.30ŌĆō7.21) | 0.010 | ||
|
|
||||
| Enterobacteiaceae spp.c | 2.00 (1.05ŌĆō3.76) | 0.035 | ||
|
|
||||
| Detection of RV by PCRd | 3.53 (1.40ŌĆō8.89) | 0.007 | 3.81(1.34ŌĆō10.82) | 0.012 |
|
|
||||
| Triple combination therapy | 2.55 (1.05ŌĆō6.17) | 0.039 | ||
|
|
||||
| Adjunctive corticosteroids treatment | 2.14 (1.23ŌĆō3.72) | 0.007 | 2.40 (1.27ŌĆō4.52) | 0.007 |
ICU, intensive care unit; OR, odds ratio; CI, confidence interval; SOFA, sequential organ failure assessment; CCI, Charlson comorbidity index; IV, intravenous; RV, respiratory virus; PCR, polymerase chain reaction.
a Human immunodeficiency virus-infected patients with CD4 counts less than 200 cells/mm3, neutrophils less than 1,000/mm3, or patients taking immunosuppressive drugs after organ transplantation.
b Impaired swallowing (esophageal disease, neurologic disease, recent extubation), impaired consciousness, increased chance of gastric contents reaching the lung (reflux, tubal feeding) and impaired cough reflex (medications, stroke, dementia).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



