INTRODUCTION
Vibrio vulnificus is a halophilic, gram-negative bacterium belonging to the Vibrio genus and Vibrionaceae family. Other members of this family include Vibrio cholera and Vibrio parahaemolyticus, both of which cause acute gastrointestinal symptoms. However, unlike other species of this family, V. vulnificus can cause serious and fatal infections [1,2], such as gastroenteritis, skin and soft tissue infections, and primary sepsis that may progress to necrotizing fasciitis and death [1,2].
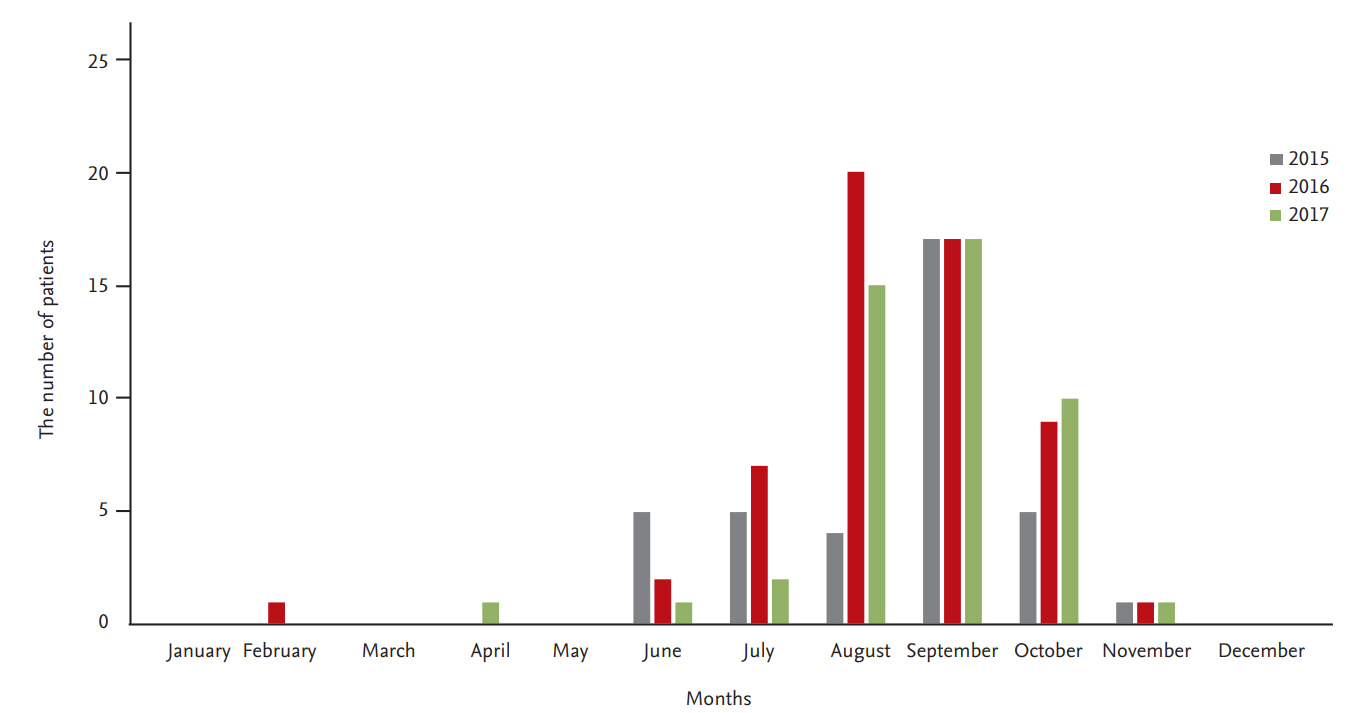
EPIDEMIOLOGY
V. vulnificus is a potentially fatal foodborne pathogen [2,3]. The Centers for Disease Control and Prevention (CDC) estimate that the average annual incidence of all V. vunlificus infections increased by 41% between 1996 and 2005 in the United States [2,3]. In Taiwan, the number of cases attributed to V. vulnificus has increased since 1985, when the first case was reported [4].
V. vulnificus infection in Korea peaks in September and is prevalent between June and November every year (Fig. 1), the period during which seawater temperature increases. Most cases occur in areas close to the coastline in South Jeolla and South Gyeongsang provinces. This infection is most prevalent when the seawater temperature is ≥ 18°C to 20°C and the salinity is approximately 25‰.
V. vulnificus can be transmitted through two channels: one is the consumption of contaminated fish and shellfish, and the other is skin exposure to contaminated seawater [5]. The sensitivity of the host is crucial for the development of V. vulnificus infection, which commonly occurs in patients with chronic liver diseases, such as alcoholic liver disease, liver cirrhosis, and chronic hepatitis B or C, or who suffer from alcohol abuse without documented liver disease. Moreover, patients with chronic diseases such as diabetes mellitus, end-stage renal disease, rheumatoid arthritis, and hemochromatosis are at high risk for serious V. vulnificus infection [6,7].
Cirrhotic patients often have immune system dysfunction, decreased complement levels and reduced phagocytic and chemotaxis capacity; therefore, the virulence of V. vulnificus is difficult to counter in these patients [5,8]. Furthermore, V. vulnificus may directly enter the portal system, bypassing the hepatic reticuloendothelial system, in patients with portal hypertension [5,8]. According to a report on V. vulnificus sepsis in Korea, > 90% of patients with V. vulnificus sepsis had some form of chronic disease, which included 66% with liver disease (43% with liver cirrhosis) and 75% with alcoholism (at least 1 oz of alcoholic beverage consumed every day) [9].
Iron levels are frequently elevated in patients with chronic liver disease and hemochromatosis, which creates a predisposition to invasive V. vulnificus infections, because this microorganism uses iron stores for bacterial overgrowth [5,8]. Wright et al. [10] reported that V. vulnificus cannot proliferate in normal human serum; they directly correlated its virulence with host iron availability based on their observation that iron injection in mouse models resulted in a reduction in 50% lethal dose. Therefore, patients with hemochromatosis are known to be susceptible to V. vulnificus infection. Some cases of V. vulnificus sepsis occurred in patients with hemochromatosis. Deferoxamine, a standard iron chelation agent widely used in treating patients with iron overload, is a type of hydroxamate siderophore of the Streptomyces species; in vitro experiments have reported that deferoxamine facilitates the proliferation of ferophilic organisms, such as V. vulnificus, Yersinia enterocolitica, and members of the order Mucorales [11]. In contrast, administration of other iron-chelation agents that are not siderophores, such as deferiprone or deferasirox, is reported to have an inhibitory effect on the growth of V. vulnificus [12]. Therefore, when V. vulnificus sepsis occurs in a patient with hemochromatosis who may require iron chelation, using deferiprone or deferasirox may be more appropriate than deferoxamine.
Interestingly, men appear to have a much higher risk for serious infection than women [13,14]. In South Korea, 506 and 82 out of 588 V. vulnificus infection cases were men (86.1%) and women (13.9%), respectively, from 2001 to 2010 [13]. In a study in Taiwan, the rates of V. vulnificus infection were also higher in men than women [4]. The reason behind this difference in susceptibility is unclear. A study involving rats showed that after the administration of V. vulnificus lipopolysaccharide extracts, the 24-hour mortality rate was 82% in male rats and 21% in female rats. However, the mortality rate of female rats without ovaries increased to nearly 75%; subsequent estrogen administration reduced the mortality rate to 38%. This demonstrates that estrogen has protective effects against V. vulnificus sepsis [15].
CLINICAL MANIFESTATIONS
V. vulnificus causes three distinct syndromes: gastrointestinal tract limited infections, wound infections, and primary septicemia [5,16]. Septicemia is one of the most common clinical problems. It is often accompanied by skin and soft tissue infections and has a > 50% mortality rate [16-18]. Atypical manifestations of V. vulnificus infection include pneumonia, meningoencephalitis, peritonitis, and pyogenic spondylitis [9,19,20].
Watery diarrhea, abdominal pain, nausea, vomiting, fever, and chills without skin and soft tissue lesions are the symptoms associated with gastrointestinal tract limited infections caused by V. vulnificus, which may occur in immunocompetent individuals; however, death due to gastrointestinal tract limited infections is rare [5]. Moreover, gastrointestinal symptoms such as nausea, vomiting, and abdominal pain are often preceded by primary septicemia with skin and soft tissue infections [2,21]. Therefore, distinguishing between simple gastrointestinal symptoms and premonitory symptoms that can worsen to septicemia is important, especially in individuals at high risk for V. vulnificus infection [22].
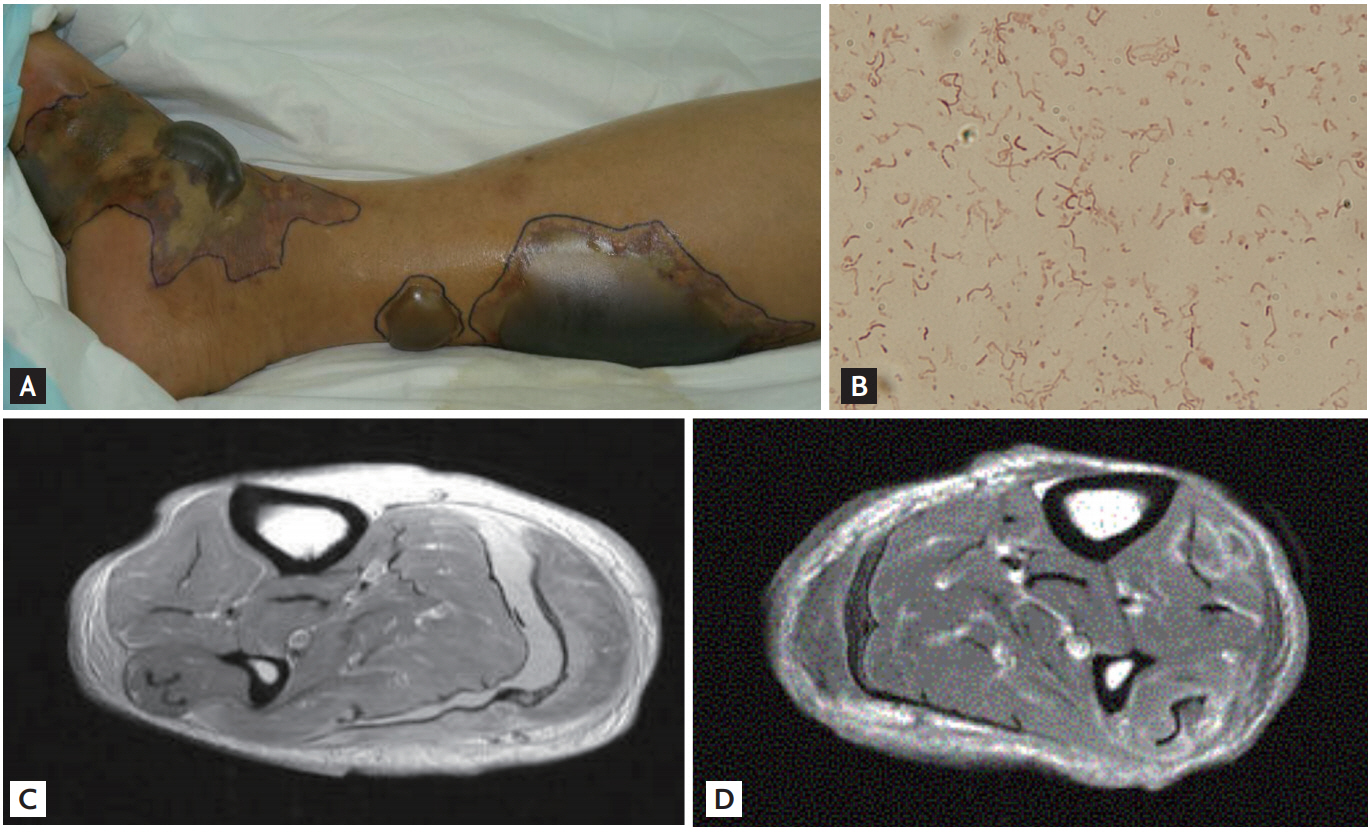
Patients with primary septicemia caused by V. vulnificus infection require hospitalization and are typically in septic shock upon admission to the emergency room. Primary septicemia is a bacteremia that usually has no definite route of infection, with the portal of entry presumably either at the small intestine or the proximal colon [16,23]. It typically begins with an abrupt fever, chills, and gastrointestinal symptoms; metastatic infection appears as skin lesions that usually occur in the lower extremities with bullae, ecchymosis, or maculopapular rash. Skin lesions are aggravated by necrotic ulcer, necrotizing fasciitis or myonecrosis (Fig. 2) [2,16,24,25].
Wound infections differ from primary septicemia because of its portal of entry in the skin; V. vulnificus enters through existing wounds or through areas of traumatic damage. The extent of wound infection with V. vulnificus varies from mild to severe. Wound infection can occur in immunocompetent individuals, such as those with simple gastroenteritis. However, in severe cases, more than half of patients suffer from severe cellulitis accompanied by bullae or ecchymosis within 24 hours of symptom onset. Skin lesions can worsen to necrotizing fasciitis or gangrene. In contrast to primary septicemia, skin lesions are limited to the areas where V. vulnificus is inoculated, and metastatic infections usually do not occur [2,5,16,24].
In a study on V. vulnificus infections in Florida from 1981 to 1987, 38 out of 62 patients had primary septicemia, 17 had wound infections, and seven had gastrointestinal illness without septicemia or wound infections [22]. A study of V. vulnificus infections in Taiwan investigated clinical and epidemiologic features from 1995 to 2000; among the 84 total patients, 20 had primary septicemia and 57 had wound infections. A similar previous study in Taiwan found that no patients had gastrointestinal illness [4,17]. Most patients with gastroenteritis or diarrheal illness in Taiwan do not seek care at the large teaching hospitals; they also do not usually have a stool culture, which might explain the lack of patients with gastrointestinal illness attributable to V. vulnificus [4,17]. A study on V. vulnificus infections in South Korea from 2000 to 2011 yielded clinical and epidemiological findings similar to the studies in Florida and Taiwan [18]. These three studies show a similar clinical profile, although they were conducted at different times and places (Table 1).
DIAGNOSIS
V. vulnificus infection is suspected based on clinical and epidemiological findings and is confirmed by bacteriological culture [16,26]. Because bacteremia is common, routine blood cultures should be performed when V. vulnificus infection is suspected. Gram stain and culture of a specimen obtained from skin lesions such as abscess or bullae is helpful to rapidly identify bacteria. Stool cultures are occasionally useful, requiring thiosulfate-citrate-bile salts-sucrose agar for isolation [16]. Culture tests using blood or skin lesion samples is the most important method for diagnosing V. vulnificus sepsis. However, since V. vulnificus is highly sensitive to antibiotic administration, it is necessary to check whether any antibiotic has been administered prior to performing the culture test.
Chart analysis of data from 23 patients with V. vulnificus subjected to blood culture tests, which were performed after admission to the researcher’s hospital, showed that even though the culture test was performed approximately 24 hours after antibiotic administration in eight patients, not even a single patient tested positive for V. vulnificus. Therefore, if a patient with suspected V. vulnificus sepsis undergoes a culture test after antibiotic administration, V. vulnificus sepsis may not be ruled out even if it is not detected [27].
Microbiological culture provides high specificity, but diagnosis takes a long time. Furthermore, V. vulnificus is susceptible to many antibiotics; therefore, infection in patients previously treated with antibiotics before culture is difficult to diagnose accurately [28]. Polymerase chain reaction (PCR) is also useful for early diagnosis of V. vulnificus infection, even in patients previously treated with antibiotics [28]. Using blood samples, the conventional PCR and nested PCR assays showed specificities of 100% and 73%, respectively. The real-time PCR assay had 100% sensitivity and specificity as a positive result using a cutoff value of < 38 cp [28]. The real-time PCR assay to detect V. vulnificus-specific genes is not only the most sensitive and specific diagnostic method but also the most rapid technique [28]. In a recent study, V. vulnificus DNA copy numbers were higher in tissue samples than in blood samples from V. vulnificus-infected patients, showing that skin lesions are more useful than blood samples for PCR-based diagnosis of V. vulnificus-infected patients [27]. Real-time PCR using serum samples collected from 14 patients at admission showed a median V. vulnificus DNA load of 638.5 copies/mL of blood (interquartile range [IQR], 37 to 3,225), while real-time PCR using the initial tissue specimen at admission showed a median of 16,650 copies/mL of tissue fluid (IQR, 4,419 to 832,500; p = 0.022). Compared with blood, DNA copies in tissue are less affected by short-term antibiotic administration, and the number of DNA copies actually increases in some patients after antibiotic administration. Therefore, there are typically a larger number of DNA copies in the tissues than in the blood of patients with V. vulnificus infection. In patients who are admitted after receiving antibiotics active against V. vulnificus, a PCR test using skin lesion specimens may be more useful than blood samples. Since studies have shown that the number of DNA copies is higher in the tissues than in the blood, the actual number of bacteria may be indirectly inferred to be higher in the tissues than in the blood. Thus, the rate of positive results in culture tests may be higher with tissue specimens of the lesion than with blood, which may require further studies [27].
Among the various marine isolates, V. vulnificus and Vibrio cholerae characteristically show resistance against polymyxin B and colistin; thus, when susceptibility to colistin is reported, the possibility of false identification of V. vulnificus should be considered [29].
TREATMENT
Data on 62 cases of V. vulnificus infection reported by Florida health authorities showed that the mortality rate was 33% when antibiotics were administered within 24 hours after admission, but increased to 63% and 100% when antibiotic administration was delayed to 48 to 72 and > 72 hours post-admission, respectively [22]. These results demonstrate the importance of timely early antibiotic administration.
Case fatality rates for V. vulnificus infections have been shown to increase with delays between the onset of illness and administration of antibiotics. Therefore, if a patient is suspected to be infected with V. vulnificus, appropriate antibiotic treatment should be immediately administered [2,5,16]. Furthermore, in many patients with serious skin and soft tissue infections such as necrotizing fasciitis, surgical interventions such as debridement or fasciotomy are necessary in addition to antibiotics treatment to remove necrotic tissue and bacteria [2,30,31]. A retrospective study on necrotizing soft-tissue infections including V. vulnificus-related necrotizing fasciitis in 65 patients demonstrated the importance of early surgical intervention based on the time from admission to surgery (25 ± 39 hours in the survival group and 90 ± 95 hours in the mortality group) [32].
A retrospective Taiwanese study on V. vulnificus-related necrotizing fasciitis outcomes in 121 patients also reported on the importance of early surgical intervention: the group of patients who received surgical treatment within 12 hours from admission had a significantly lower mortality rate than patients who received similar treatment 12 to 24 and > 24 hours post-admission [33]. However, since these studies were retrospective, the possibility of selection bias may exist where surgeries were performed on patients with conditions mild enough to actually undergo surgery. Therefore, future prospective case-control studies are needed.
V. vulnificus is sensitive to most antibiotics in vitro, except for colistin; antibiotics that are effective against V. vulnificus in vitro are third-generation cephalosporins (ceftriaxone, cefotaxime, or ceftazidime), piperacillin-tazobactam, carbapenems (imipenem or meropenem), tetracyclines (doxycycline or tetracycline), aminoglycoside (gentamicin or amikacin), fluoroquinolones (ciprofloxacin, levofloxacin, or moxifloxacin), and sulfamethoxazole-trimethoprime [31,34]. In most in vitro or in vivo mouse model experiments on antibiotic susceptibility, tetracyclines are reported to have significantly higher efficacy than penicillin or cephalosporins. This has been attributed to the fact that the tetracycline class of antibiotics achieves better penetration into tissues with poor perfusion when V. vulnificus infection occurs, and has inhibitory effects against the synthesis of proteins, such as various toxins and enzymes produced by V. vulnificus [35].
A time-kill study on V. vulnificus demonstrated that cefotaxime and minocycline have synergistic effects, and a V. vulnificus mouse model experiment also reported that the combined administration of the two drugs showed statistically significant effects (p < 0.01) [36].
A study on the efficacy of quinolone also confirmed that it was as effective as cefotaxime and minocycline; quinolone was reported to be effective in mouse models, as its concentration was sufficiently maintained in the necrotized interstitial fluid or blister and thrombosis caused by V. vulnificus sepsis [37].
A time-kill study on ciprofloxacin and cefotaxime confirmed their synergistic action, while an animal experiment confirmed that the combined administration of cefotaxime and ciprofloxacin offered greater survival benefits than a combination of cefotaxime and minocycline or cefotaxime alone [38,39].
The CDC recommends doxycycline 100 mg intravenously or orally twice a day plus ceftazidime (or any other third-generation cephalosporin) 1 to 2 g intravenously every 8 hours for the treatment of V. vulnificus infection [5,16,40]. In a retrospective study on 89 V. vulnificus-infected patients, a third-generation cephalosporin plus minocycline or ciprofloxacin with or without minocycline was found to be more effective than a third-generation cephalosporin alone [41]. An animal experiment suggested that the combination of ciprofloxacin and cefotaxime is an effective treatment option for V. vulnificus-infected people [39]. A recent study suggested that cefepime combined with doxycycline or ciprofloxacin should be initiated to cover gram-negative-resistant organisms and V. vulnificus while awaiting a microbiological diagnosis; once a diagnosis of V. vulnificus septicemia is confirmed, treatment can be safely changed to ceftriaxone combined with doxycycline or ciprofloxacin [42]. Another recent study suggested that tigecycline alone might be a better therapeutic option than a traditional combination regimen of ceftazidime plus doxycycline in patients with V. vulnificus infection [43,44].
PROGNOSIS
V. vulnificus infections are life-threatening, and favorable prognosis depends on early diagnosis and appropriate treatment. Several previous studies suggested a marker for predicting prognosis among patients with V. vulnificus infection. Acute Physiology And Chronic Health Evaluation II (APACHE II) and Mortality in Emergency Department Sepsis (MEDS) scores at hospital admission were suggested as useful prognostic indicators in primary septicemia or wound infections caused by V. vulnificus [31,45,46]. In another study, the level of V. vulnificus DNA loads were significantly correlated with mortality [47].
The median DNA copy upon admission was 2,300 copies/mL of blood (IQR, 558 to 11,350) in patients who died of V. vulnificus sepsis, which was significantly higher than 316.5 copies/mL of blood (IQR, 51 to 705) in those who survived (p = 0.011). When a patient is admitted for V. vulnificus sepsis, using real-time PCR for the identification of V. vulnificus DNA copies in the serum as an early prognostic indicator of mortality may be clinically useful [47].
The level of V. vulnificus DNA was shown to be substantially higher in nonsurvivors than in survivors of V. vulnificus septicemia, and the V. vulnificus DNA load correlated with the APACHE II score [18,47]. Notably, elevated tumor necrosis factor α (TNF-α) levels were found in patients with V. vulnificus sepsis compared to those in healthy individuals. The group of patients who died of V. vulnificus sepsis showed a median TNF-α level of 261.0 pg/mL (IQR, 101.0 to 376.0), which was significantly higher than 69.5 pg/mL (IQR, 17.5 to 103.5) in those who survived (p = 0.001). Such a difference was also found in the blood test results, which were evaluated 6 to 48 hours post-admission and antibiotic administration; the mortality group showed a significantly elevated TNF-α level (p = 0.044). This confirmed that checking the serum TNF-α level upon admission as an early prognostic factor of mortality may be clinically useful [48]. In a retrospective study in South Korea, approximately half of the patients with V. vulnificus infection died ≤ 72 hours after hospital admission [18]. In this study, patient survival differed significantly based on pH level at hospital admission; in predicting death, an optimal cutoff pH level of < 7.35 had a sensitivity of 100% and specificity of 83% [17]. This study showed that the initial pH level of patients was the simplest and the most accurate predictive marker of death [18].
CONCLUSIONS
V. vulnificus is capable of causing illness ranging from mild gastrointestinal tract-limited infections to severe septicemia with necrotizing fasciitis. Patients with a presumptive diagnosis of V. vulnificus infection should be immediately started on antibiotics therapy and surgical interventions if needed. The recommended antibiotics treatment regimen is ceftriaxone plus doxycycline or ceftriaxone plus ciprofloxacin. pH level upon admission, APACHE II score, and V. vulnificus DNA load can help predict the prognosis for patients with V. vulnificus infection.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





