 |
 |
| Korean J Intern Med > Volume 30(4); 2015 > Article |
|
See the editorial "Hyponatremia in acute heart failure: a marker of poor condition or a mediator of poor outcome?" on page 450.
Abstract
Background/Aims
Hyponatremia is a well-known risk factor for poor outcomes in Western studies of heart failure (HF) patients. We evaluated the predictive value of hyponatremia in hospitalized Asian HF patients.
Methods
The Clinical Characteristics and Outcomes in the Relation with Serum Sodium Level in Asian Patients Hospitalized for Heart Failure (the COAST) study enrolled hospitalized patients with systolic HF (ejection fraction < 45%) at eight centers in South Korea, Taiwan, and China. The relationship between admission sodium level and clinical outcomes was analyzed in 1,470 patients.
Results
The mean admission sodium level was 138 ┬▒ 4.7 mmol/L, and 247 patients (16.8%) had hyponatremia defined as Na+ < 135 mmol/L. The 12-month mortality was higher in hyponatremic patients (27.9% vs. 14.6%, p < 0.001), and hyponatremia was an independent predictor of 12-month mortality (hazard ratio, 1.72; 95% confidence interval, 1.12 to 2.65). During hospital admission, 57% of hyponatremic patients showed improvement without improvement in their clinical outcomes (p = 0.620). The proportion of patients with optimal medical treatment was only 26.5% and 44.2% at admission and discharge, respectively, defined as the combined use of angiotensin-converting-enzyme inhibitor/angiotensin receptor blocker and ╬▓-blocker. Underuse of optimal medical treatment was more pronounced in hyponatremic patients.
Hospitalized heart failure (HF) patients require more advanced medical care [1]. However, data on the clinical characteristics of these patients are scarce because studies in the past 30 years have focused on non-hospitalized HF patients. Hyponatremia is a common phenomenon that correlates with HF outcomes and has been identified as a prognostic factor in chronic HF patients in Western studies [23], although the prognostic value of hyponatremia in hospitalized HF patients remains to be established, particularly in Asian HF patients. In addition, the adherence to evidence-based therapy in hospitalized Asian HF patients is unknown.
The aim of the present multinational, multicenter study was to evaluate the prognostic value of hyponatremia and the adherence to evidence-based therapy in hospitalized Asian patients with systolic HF.
The present study was approved by the Institutional Review Board (IRB) or Ethics Committee of Seoul National University Bundang Hospital, Severance Hospital, Wonju Christian Hospital, National Taiwan University Hospital, Taipei Veterans General Hospital, Chang Gung Memorial Hospital, Fuwai Hospital, and Zhong Shan Hospital. Informed consent was waived by the IRB of each participating center that complied with the Declaration of Helsinki.
The study on the Clinical Outcomes in Relation with Serum Sodium Level in Asian Patients Hospitalized for Heart Failure (COAST) was a multinational, multicenter registry involving eight centers in South Korea, Taiwan, and China. The study population included all adult patients Ōēź 18 years of age who were hospitalized for HF and left ventricular ejection fraction < 45% at admission since January 2009. HF was diagnosed with at least one of the pre-defined International Classification of Diseases 9 (ICD9)/ICD10 HF-related diseases, or with any disease corresponding to the codes. In total, 550 consecutive patients per region were scheduled to enroll for a sum of 1,650 patients. Index admission, discharge, and 1-year follow-up data were collected from each patient.
Patient demographic and baseline characteristics, underlying diseases, clinical presentation, causes of HF, treatment strategy (diuretics, nitrate, inotropes, anti-arrhythmics, anticoagulants, antiplatelet agents, blood transfusion), laboratory tests (serum sodium, potassium, creatinine, creatinine clearance, blood urea nitrogen), and outcomes during admission and after discharge were recorded. Data were collected at each site by trained study coordinators using a standardized case report form, and were entered into the COAST Registry database via a web-based electronic data capture system. Data collection and audits were performed by the COAST Registry Steering Committee.
The primary endpoint was the 12-month mortality from the index hospitalization for decompensated HF according to the serum sodium levels. Hyponatremia was defined as serum Na+ < 135 mmol/L. The secondary endpoints included the mortality rate at index-admission, 12-month rehospitalization rate, the composite of mortality and/or rehospitalization and 12-month mortality rate according to changes in serum sodium status during the hospital stay, and adherence to the evidence-based therapy according to serum sodium level.
Based on the EuroHeart Failure Survey study, the 12-month mortality rate among hospitalized HF patients was assumed to be 29.5% and 18.9% for hyponatremic and normonatremic patients, respectively [4]. Thus, a total of 1,650 patients were needed to detect a significant difference in 12-month mortality rate between the normonatremia and hyponatremia groups with a power of 0.80 and at a two-sided ╬▒ level of 0.05.
Data are presented as numbers and frequencies for categorical variables and as mean ┬▒ standard deviation (SD) for continuous variables. For comparison between groups, the chi-square test (or Fisher exact test when any expected cell count was < 5 for a 2 ├Ś 2 table) and McNemar tests were used for categorical variables, and the Mann-Whitney U tests were applied for continuous variables. The Kruskal-Wallis test and Wilcoxon ranksum test were used for comparisons of serum sodium with continuous measures, multilevel nominal measures, and dichotomous measures, respectively. A propensity score matching age, gender, region, left ventricle ejection fraction, systolic blood pressure (BP), serum potassium, serum creatinine, medical history, and basal metabolic index (BMI) was also performed between the normonatremia and hyponatremia groups. The variables were incorporated as predictors in a non-parsimonious logistic regression model with the presence of hyponatremia as the outcome. The propensity score was defined as the conditional probability of being a hyponatremic patient given the covariates listed above. Caliper matching was used to pair the hyponatremic patients to similar patients with normal sodium levels, as it was considered the most transparent method. This one-to-one match was performed without replacement. Multivariable models of 12-month mortality, in-hospital death, and length of hospital stay were developed to allow for assessing associations of these outcomes with other patient and clinical variables with consistent covariate adjustment. The following variables associated with 12-month mortality with p < 0.05 were included: age in decade, current smoking, BMI, diabetes mellitus, hypertension, glomerular filtration rate (GFR) mL/min/1.73 m2, coronary artery disease, stroke, chronic obstructive pulmonary disease (COPD), New York Heart Association (NYHA) Functional Class, hyponatremia, diastolic BP, serum potassium and use of angiotensin converting enzyme inhibitor (ACEi), angiotensin receptor blocker (ARB), ╬▓-blocker, calcium channel blocker (CCB), oral furosemide, spironolactone, or dobutamine. All of the data were analyzed using SAS version 9 (SAS Institute, Cary, NC, USA) by a professional statistician.
A total of 1,653 patients were initially assessed. In total, seven patients were not eligible due to violation of inclusion criteria, 17 patients had missing serum sodium levels, and 159 patients were lost to follow-up. Thus, 1,470 patients were available for the final analysis. The mean age was 66 years, and 67% of the patients were men, 32% had diabetes mellitus, 51% had hypertension, 49% had chronic kidney disease defined as GFR < 60 mL/min/1.73 m2, and 45% had ischemic cardiomyopathy as the cause for HF.
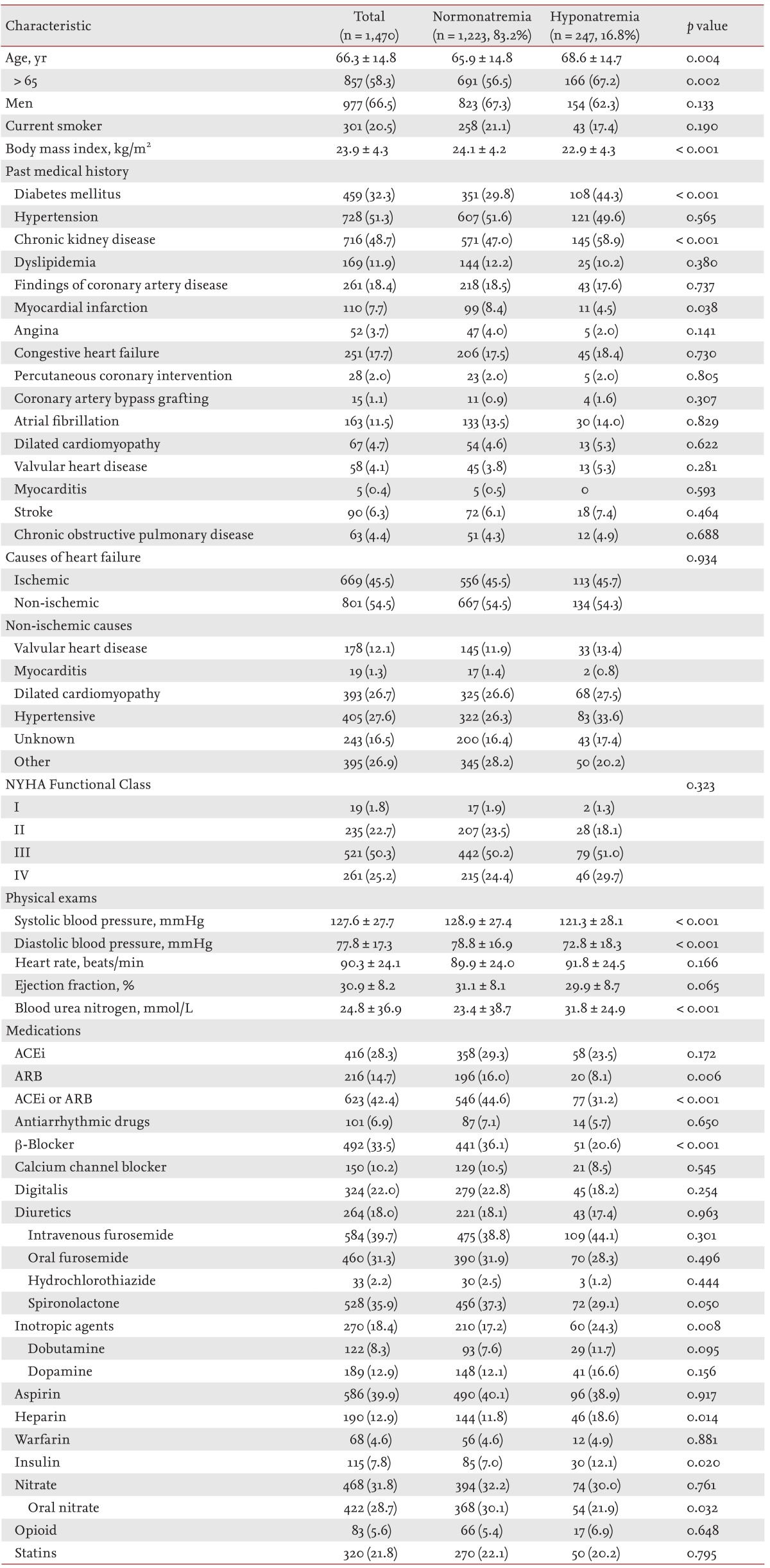
The mean admission sodium level was 138 ┬▒ 4.7 mmol/L and showed a unimodal distribution. Two hundred forty-seven patients (16.8%) had hyponatremia at hospital admission. Hyponatremic patients had more adverse baseline characteristics including older age (68.6 ┬▒ 14.7 years vs. 65.9 ┬▒ 14.8 years, p = 0.004), and a higher frequency of chronic kidney disease (58.9% vs. 47.0%, p < 0.001). They also had a lower frequency of myocardial infarction history (4.5% vs. 8.4%, p = 0.038), use of ACEi/ARBs (31.2 vs. 44.6%, p < 0.001), ╬▓-blocker (20.6% vs. 36.1%, p < 0.001), or spironolactone (29.1% vs. 37.3%, p = 0.050) (Table 1). In addition, on physical examination, hyponatremic patients had lower BP (systolic BP, 121.3 ┬▒ 28.1 mmHg vs. 129 ┬▒ 27.4 mmHg, p < 0.001; diastolic BP, 72.8 ┬▒ 18.3 mmHg vs. 78.8 ┬▒ 16.9 mmHg, p < 0.001). NYHA class did not differ between both groups (p = 0.323). The diuretic dose also did not differ between normonatremia and hyponatremia groups (intravenous furosemide: 34 ┬▒ 28.7 mg vs. 36.5 ┬▒ 34.3 mg, p = 0.569; oral furosemide: 30.6 ┬▒ 21.8 mg vs. 36.4 ┬▒ 30.7 mg, p = 0.287; thiazide 18 ┬▒ 9.8 mg vs. 13.8 ┬▒ 10.6 mg, p = 0.500; spironolactone 26.4 ┬▒ 16.3 mg vs. 26.3 ┬▒ 15.2 mg, p = 0.583).
Two hundred forty-seven patients (16.8%) died in the first 12 months. The patients who died were older (71.9 ┬▒ 14.3 years vs. 65.2 ┬▒ 14.6 years, p < 0.001), had a lower BMI (22.2 ┬▒ 3.6 kg/m2 vs. 24.2 ┬▒ 4.3 kg/m2, p < 0.001), were less likely to be current smoker (13.8% vs. 21.8%, p = 0.004), and were more likely to have diabetes mellitus (40.8% vs. 30.6%, p = 0.002), hypertension (57.6% vs. 50.0%, p = 0.031), chronic kidney disease (20.4% vs.10.6%, p < 0.001), coronary artery disease (22.9% vs. 17.4%, p = 0.047), a previous history of stroke (9.8% vs. 5.6%, p = 0.015), COPD (6.9% vs. 3.9%, p = 0.037), and more advanced NYHA class (p < 0.001). They also had lower systolic BP (122.8 ┬▒ 28.9 mmHg vs. 128.6 ┬▒ 27.3 mmHg, p = 0.004), lower serum sodium level (136.7 ┬▒ 5.7 mmol/L vs. 138.6 ┬▒ 4.3 mmol/L), higher potassium level (4.4 ┬▒ 0.8 mmol/L vs. 4.3 ┬▒ 0.6 mmol/L, p = 0.017) and lower GFR (52.8 ┬▒ 29.1 mL/min/1.73 m2 vs. 65.9 ┬▒ 26.8 mL/min/1.73 m2) (Supplementary Table 1). Patients who died received less ACEi or ARB (30.0% vs. 44.9%, p < 0.001), ╬▓-blocker (25.9% vs. 35.0%, p = 0.007), CCB (6.9% vs. 10.9%, p = 0.026), or oral furosemide (26.3% vs. 32.3%, p = 0.028), but received more dobutamine (13.4% vs. 7.3%, p = 0.002).
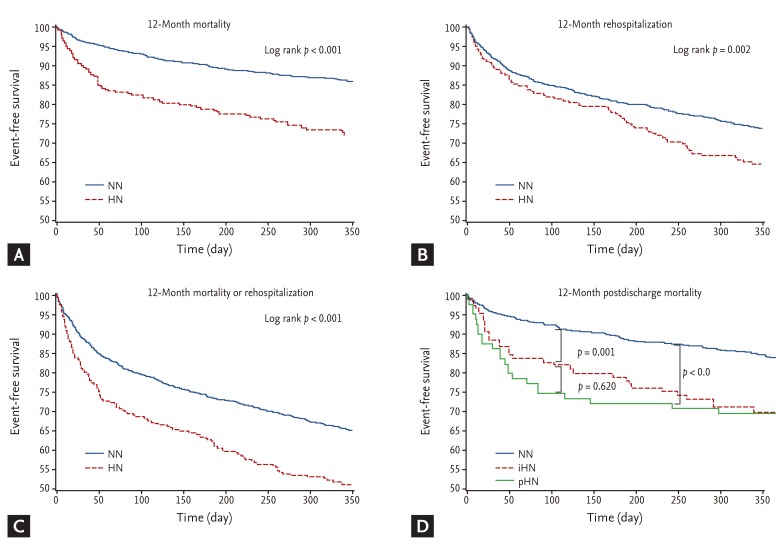
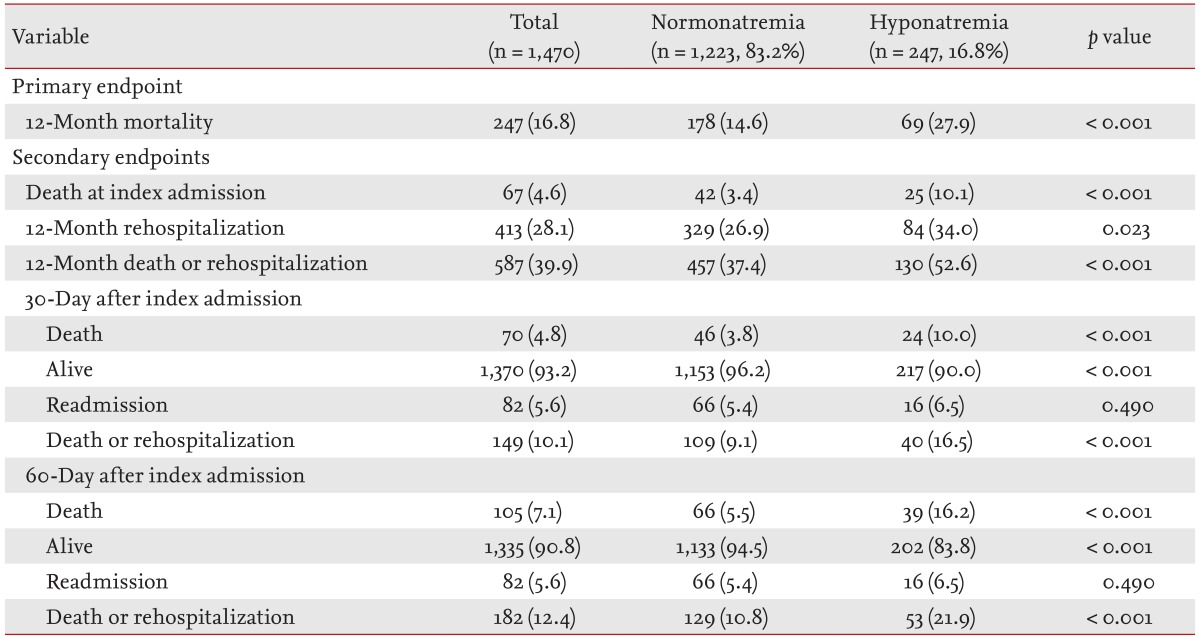
There was a "J-curve" relationship between the serum sodium level and 12-month mortality; patients with a serum sodium level of 140 mmol/L had the lowest 12-month mortality rate, and the mortality increased in both directions away from 140 mmol/L (Supplementary Fig. 1). The 12-month mortality rate was higher in the hyponatremia group than normonatremia group (27.9% vs. 14.6%, log-rank p < 0.001) (Fig. 1A). When analyzing the secondary endpoints, patients with hyponatremia had a higher 12-month rehospitalization rate (34.0% vs. 26.9%, log-rank p = 0.002) (Fig. 1B), and higher composite of 12-month death or rehospitalization (52.6% vs. 37.4%, log-rank p < 0.001) (Table 2, Fig. 1C).
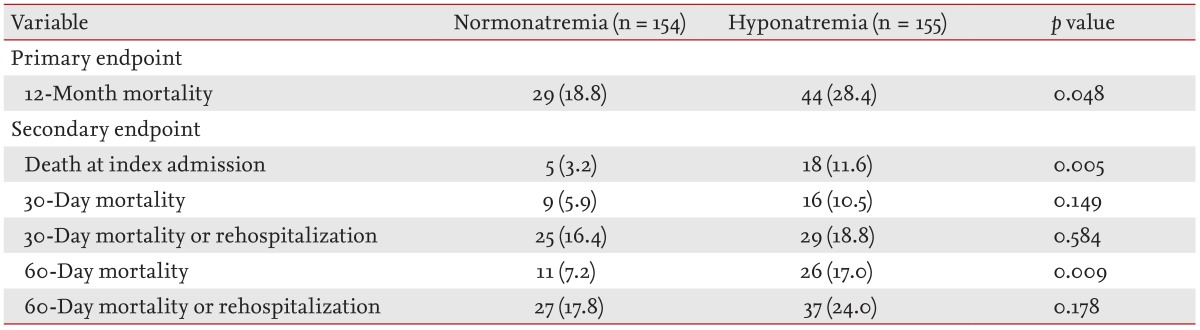
In the Cox proportional-hazards regression model, hyponatremia was an independent predictor of 12-month mortality with 72% increase in mortality (hazard ratio, 1.72; 95% confidence interval, 1.12 to 2.65), along with current smoking, BMI, GFR, NYHA Functional Class, and diastolic BP (Table 3). With regard to the relationship between 12-month mortality and clinical outcome, the mortality rate was lowest in patients with a serum sodium level of 140 mmol/L and increased with distance from 140 mmol/L. After propensity score matching for baseline characteristics, the data of 155 patients in each group were available. The primary endpoint was higher in the hyponatremia group than in the normonatremia group (28.4% vs. 18.8%, p = 0.048) (Table 4).
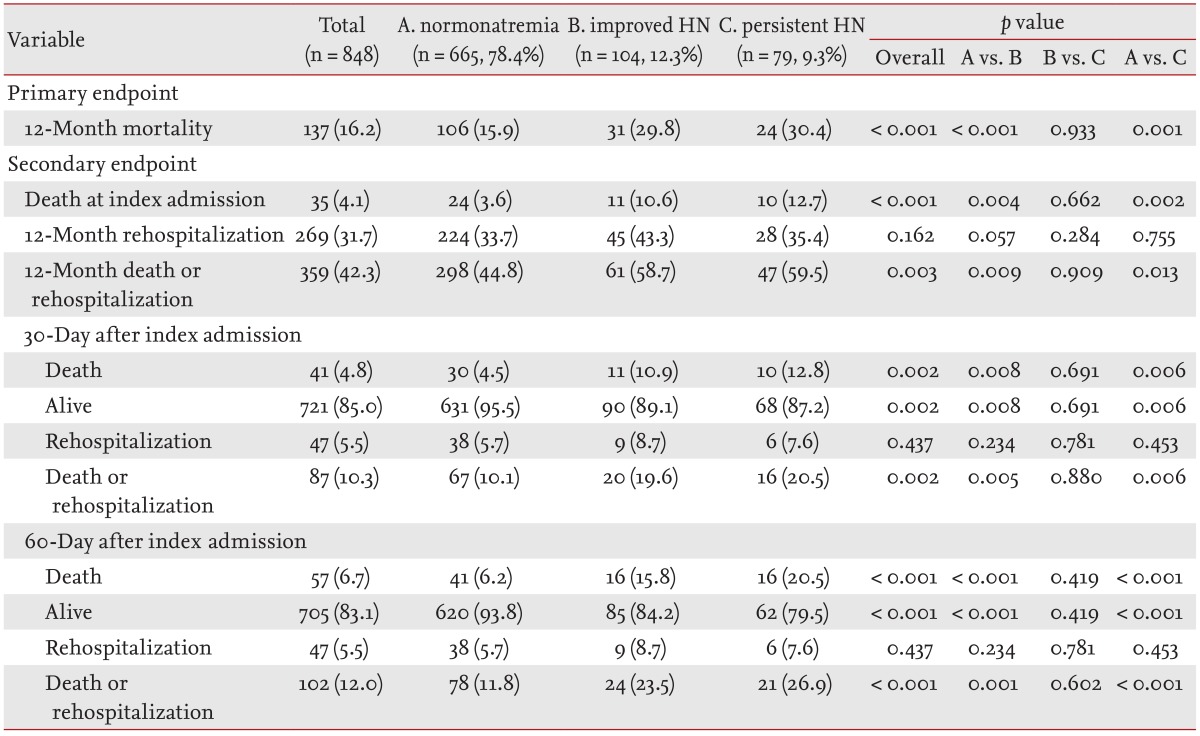
One hundred eighty-three patients with hyponatremia survived the discharge. Among those, 56.8% showed improvement of hyponatremia (improved HN) at the hospital discharge, whereas 43.2% showed persistent hyponatremia (persistent HN). Change in hyponatremia status was not associated with improvement in clinical outcome (Table 5, Fig. 1D).
By defining optimal medical treatment (OMT) as the combined use of ACEi/ARB, ╬▓-blocker, and/or aldosterone antagonists, the proportion of patients on OMT was only 12.8% in hyponatremia patients and 26.5% in normonatremia patients (p < 0.001) at index admission. At discharge, 33.5% of the hyponatremia patients and 44.2% of the normonatremia patients received OMT (p < 0.001), demonstrating that hyponatremic patients received less OMT compared to the normonatremic patients (Supplementary Table 2).
In the present multinational, multicenter study, we showed that hyponatremia at admission was common in hospitalized Asian HF patients and was an independent predictor of poor clinical outcomes. The correction of hyponatremia during hospital stay was not associated with improved outcomes, and adherence to OMT was lower in hyponatremia HF group compared to the normonatremia group. To the best of our knowledge, this is the first study to investigate the prognostic effect of hyponatremia and adherence to OMT in hospitalized HF-patients from three East-Asian countries.
Hyponatremia was observed in 17% of the hospitalized HF patients. The rate was comparable that observed in other studies of acute decompensated HF [567]. Hyponatremic patients had unfavorable baseline characteristics, were less likely to receive OMT, and had worse clinical outcomes. The primary endpoint of 12-month mortality was 2-fold higher in the hyponatremia group than in the normonatremia group, and hyponatremia was associated with worse short-term, mid-term, and long-term outcomes. In the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) [8] and the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) [7], and sodium (per 3-mEq/L decrease from 140 mEq/L), there was an OR of 1.25, 1.18, and 1.10 for in-hospital mortality, 60-day mortality, and 60 to 90 day mortality, respectively. In our study, hyponatremia was associated with a 72% increased risk for 12-month mortality.
Hyponatremia develops slowly, paralleling the rate of progression of heart disease. The mechanistic explanation for the development of hyponatremia in HF patients is as follows: in HF patients, the low cardiac output and BP lead to (1) an increase in sympathetic tone; (2) activation of the renin-angiotensin-aldosterone system; and (3) non-osmotic release of vasopressin to preserve arterial blood volume and pressure [910]. Increased angiotensin II and aldosterone levels lead to decreased sodium and water delivery to the collecting duct, and result in impairment of free-water excretion and hyponatremia [9]. Furthermore, angiotensin II is a potent thirst stimulator and releases arginine vasopressin from neurohypophysis promoting free water intake and retention by increasing the number of aquaporin in the collecting duct [1112]. Finally, the concomitant use of diuretics in HF patients also contributes to hyponatremia. Because these neurohumoral changes are related to the severity of HF, hyponatremia identifies a group of HF patients in more advanced stages, explaining the worse clinical outcomes.
The treatment strategy of hyponatremia in HF patients includes improvement of hemodynamics, fluid restriction, and the recent use of vasopressin receptor antagonists [5131415]. ACEi and ARBs reduce the afterload and improve the hemodynamics [1617], cardiac output, neurohumoral parameters [18], serum sodium levels, and survival [161719].
The American College of Cardiology/American Heart Association guideline recommends prescription of ACEi/ARB and ╬▓-blockers in all patients and aldosterone antagonists in selected HF patients [20]. The proportion of HF patients on OMT was only 26.5% at the index hospital admission, which reflects a low adherence to recommended treatment guidelines in "real world practice" in Asian HF-patients. The proportion of patients on OMT significantly increased to 44.2% at hospital discharge, which was lower than the rate observed in the OPTIMIZE-HF registry where > 80% of patients received ACEi/ARBs and ╬▓-blockers. It is important to note that more than half of the eligible Asian patients remained untreated with evidence-based therapies at hospital discharge. Furthermore, the underuse was more pronounced in hyponatremic patients. It is not clear whether the low adherence to OMT in hyponatremic patient can account for poorer clinical outcomes in hyponatremic patients, or whether OMT was withheld from hyponatremic patients because they had unfavorable clinical presentation. Hyponatremic HF patients are more susceptible to the hypotensive and azotemic effects of ACEi, possibly because they are more dependent on neurohormones to sustain BP. Therefore the initiation or up-titration of ACEi is particularly difficult in these patients [17]. However, hyponatremia identifies a high-risk population that may benefit from intensive medical treatment, and every effort should be made to ensure that all eligible patients receive evidence-based therapy.
It is not clear, whether hyponatremia is a marker or mediator. In the present study, the improvement of hyponatremia was observed in 57% of hyponatremic patients during hospital stay. However, the postdischarge clinical outcomes of patients with improved hyponatremia did not differ from those with persistent hyponatremia. This result was similar to that of Lee et al. [21], who also showed that the improvement of hyponatremia during hospitalization was not associated with a lower incidence of composite endpoint of death or rehospitalization. These results indicate that short-term improvement of hyponatremia cannot be associated with improved prognosis. The post hoc analysis of the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) trial demonstrated that correction of hyponatremia with tolvaptan improved outcomes [15]. Whether long-term improvement of hyponatremia is associated with better outcomes needs to be evaluated in further studies.
There were several limitations in this study. Most importantly, the COAST study was not a prospective, randomized trial. Although we tried to adjust for significant clinical variables and performed propensity score matching for the analysis, unmeasured confounding factors may have biased the study result. Second, the COAST hospitals included nine self-selected centers in three nations. Therefore, the patients' management in each site may not be entirely representative of national care patterns of the participating nations and especially, each site or location may have a different socioeconomic background, medical resources, and trend for treatment.
In conclusion, in the present multinational, multicenter analysis, hyponatremia is common in a representative population of hospitalized HF-patients and serum sodium levels on admission is an important predictor of clinical outcomes, irrespective of whether hyponatremia improves during hospital stay. Furthermore, the adherence to evidence-based HF treatment is low in hospitalized Asian HF patients, and this observation suggests that additional strategies are needed to encourage physicians to prescribe the necessary medications in eligible HF patients.
1. Hyponatremia is common in among hospitalized Asian heart failure (HF) patients from South Korea, China, and Taiwan, and is associated with a 72% increased risk of 12-month mortality.
2. Hyponatremia is an important predictor of clinical outcomes, irrespective of whether hyponatremia improves during hospital stay.
3. The adherence to evidence-based HF treatment is low in hospitalized Asian HF patients, especially in those with hyponatremia.
Conflict of Interest
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Supplementary Material
Supplementary Table 2
Optimal medical treatment according to serum sodium level
Supplementary Figure 1
12-Month mortality according to serum sodium level in bar graph (A) and restrictive cubic spline transformation (B).
References
1. Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA 2003;290:2581ŌĆō2587PMID : 14625335.


2. Kearney MT, Fox KA, Lee AJ, et al. Predicting death due to progressive heart failure in patients with mild-to-moderate chronic heart failure. J Am Coll Cardiol 2002;40:1801ŌĆō1808PMID : 12446064.


3. Senni M, De Maria R, Gregori D, et al. Temporal trends in survival and hospitalizations in outpatients with chronic systolic heart failure in 1995 and 1999. J Card Fail 2005;11:270ŌĆō278PMID : 15880335.


4. Harjola VP, Follath F, Nieminen MS, et al. Characteristics, outcomes, and predictors of mortality at 3 months and 1 year in patients hospitalized for acute heart failure. Eur J Heart Fail 2010;12:239ŌĆō248PMID : 20156940.


5. Gheorghiade M, Gattis WA, O'Connor CM, et al. Effects of tolvaptan, a vasopressin antagonist, in patients hospitalized with worsening heart failure: a randomized controlled trial. JAMA 2004;291:1963ŌĆō1971PMID : 15113814.


6. Gheorghiade M, Abraham WT, Albert NM, et al. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J 2007;28:980ŌĆō988PMID : 17309900.


7. Klein L, O'Connor CM, Leimberger JD, et al. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation 2005;111:2454ŌĆō2460PMID : 15867182.


8. Abraham WT, Fonarow GC, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol 2008;52:347ŌĆō356PMID : 18652942.


9. Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med 1999;341:577ŌĆō585PMID : 10451464.


10. Schrier RW, Berl T. Mechanism of effect of alpha adrenergic stimulation with norepinephrine on renal water excretion. J Clin Invest 1973;52:502ŌĆō511PMID : 4683886.



11. Schrier RW, Berl T, Anderson RJ. Osmotic and nonosmotic control of vasopressin release. Am J Physiol 1979;236:F321ŌĆōF332PMID : 373467.


12. Goldsmith SR, Francis GS, Cowley AW Jr. Arginine vasopressin and the renal response to water loading in congestive heart failure. Am J Cardiol 1986;58:295ŌĆō299PMID : 3739918.


13. Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med 2006;355:2099ŌĆō2112PMID : 17105757.


14. Udelson JE, McGrew FA, Flores E, et al. Multicenter, randomized, double-blind, placebo-controlled study on the effect of oral tolvaptan on left ventricular dilation and function in patients with heart failure and systolic dysfunction. J Am Coll Cardiol 2007;49:2151ŌĆō2159PMID : 17543634.


15. Konstam MA, Gheorghiade M, Burnett JC Jr, et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA 2007;297:1319ŌĆō1331PMID : 17384437.


16. Lee WH, Packer M. Prognostic importance of serum sodium concentration and its modification by converting-enzyme inhibition in patients with severe chronic heart failure. Circulation 1986;73:257ŌĆō267PMID : 3002660.


17. Packer M, Medina N, Yushak M. Relation between serum sodium concentration and the hemodynamic and clinical responses to converting enzyme inhibition with captopril in severe heart failure. J Am Coll Cardiol 1984;3:1035ŌĆō1043PMID : 6323565.


18. Riegger GA, Kochsiek K. Vasopressin, renin and norepinephrine levels before and after captopril administration in patients with congestive heart failure due to idiopathic dilated cardiomyopathy. Am J Cardiol 1986;58:300ŌĆō303PMID : 3526857.


19. Packer M, Lee WH, Kessler PD, Medina N, Yushak M, Gottlieb SS. Identification of hyponatremia as a risk factor for the development of functional renal insufficiency during converting enzyme inhibition in severe chronic heart failure. J Am Coll Cardiol 1987;10:837ŌĆō844PMID : 2821091.


20. Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 2009;119:1977ŌĆō2016PMID : 19324967.


Figure┬Ā1
Clinical outcomes based on serum sodium levels. (A) Hospitalized hyponatremic patients had a higher 12-month mortality rate, (B) higher 12-month rehospitalization rate, and (C) higher composite 12-month mortality and rehospitalization rate. The distribution of patients with normonatremia (NN), improved hyponatremia (iHN), and persistent hyponatremia (pHN) was 78.4%, 12.3%, and 9.3%, respectively. The 12-month postdischarge mortality was lowest in the NN group (15.9%) compared to iHN (29.8%) and pHN groups (30.4%). (D) The outcome did not differ between iHN and pHN groups (p = 0.620), suggesting that short-term changes in HN status were not associated with improved clinical outcomes.
Table┬Ā3
Independent predictors of 12-month mortality
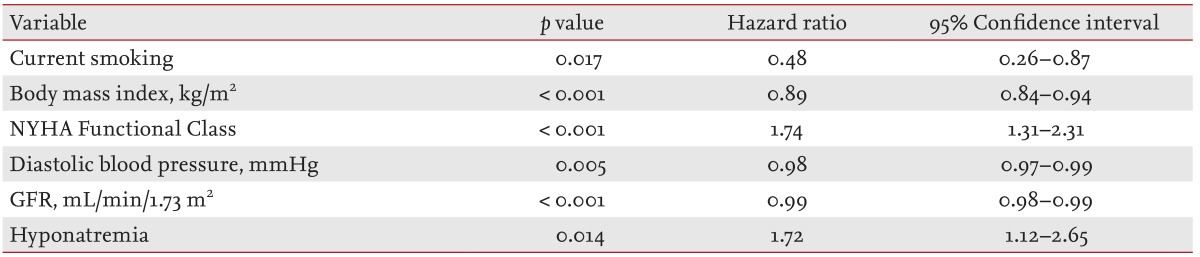
Cox-proportional hazard ratio, forward conditional. Variables associated with 12-month mortality with p < 0.05 were included: age in decade, current smoking, body mass index, diabetes mellitus, hypertension, (mL/min/1.73 m2), coronary artery disease, stroke, chronic obstructive pulmonary disease, NYHA Functional Class, hyponatremia, diastolic blood pressure, serum potassium and use of angiotensin converting enzyme inhibitor, angiotensin receptor blocker, ╬▓-blocker, calcium channel blocker, oral furosemide, spironolactone or dobutamine.
NYHA, New York Heart Association; GFR, glomerular filtration rate.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



