INTRODUCTION
Community-acquired pneumonia (CAP) is a common and potentially serious illness. It is associated with considerable morbidity and mortality, particularly in elderly patients and those with significant underlying diseases [
1,
2]. Some studies have indicated that the incidence of CAP increases substantially with age, and patients > 60 years account for 81.2% of all cases [
3,
4,
5]. Furthermore, the hospitalization rate due to CAP increases with every decade of life until the eighth decade [
3,
4,
5]. The overall annual incidence of CAP in adults also increases with age (14 per 1,000 person-year in adults age Ōēź 65 years) [
6]. Additionally, age is an independent risk factor for pneumonia, after controlling for confounding variables, such as underlying disease conditions, immobility, and use of tranquilizers [
7,
8]. Moreover, the elderly are more susceptible to pneumonia due to the anatomical and physiological changes that occur in the lungs with age [
7,
8].
A study conducted in Denmark demonstrated that the incidence of pneumonia requiring hospitalization increased by 50% from 1994 to 2004, and reported a persistently high mortality rate [
9]. A Korean study of the pneumonia burden in 764 inpatients with CAP (age, Ōēź 50 years) revealed that 3.2% patients died during treatment [
10]. Mortality occurs primarily in the elderly and is frequently associated with underlying diseases. Moreover, CAP is not only an increasing mortality factor in these patients but is associated with a significant economic burden in the Asia-Pacific region [
10,
11].
Although many Korean studies have reported the incidence of CAP and its associated risk factors, there is a lack of information regarding the elderly, the group that most frequently experiences severe illness and underlying disease [
10,
11,
12]. Furthermore, no comparative information is available on disease burden in those patients. To better understand the influence of age and underlying disease, we focused on the disease burden of inpatients with CAP according to aging factors and the presence of underlying diseases. Furthermore, we analyzed the variables associated with disease severity, cost, and outcome.
DISCUSSION
This study involved a subgroup analysis, which was first conducted by Yoo et al. [
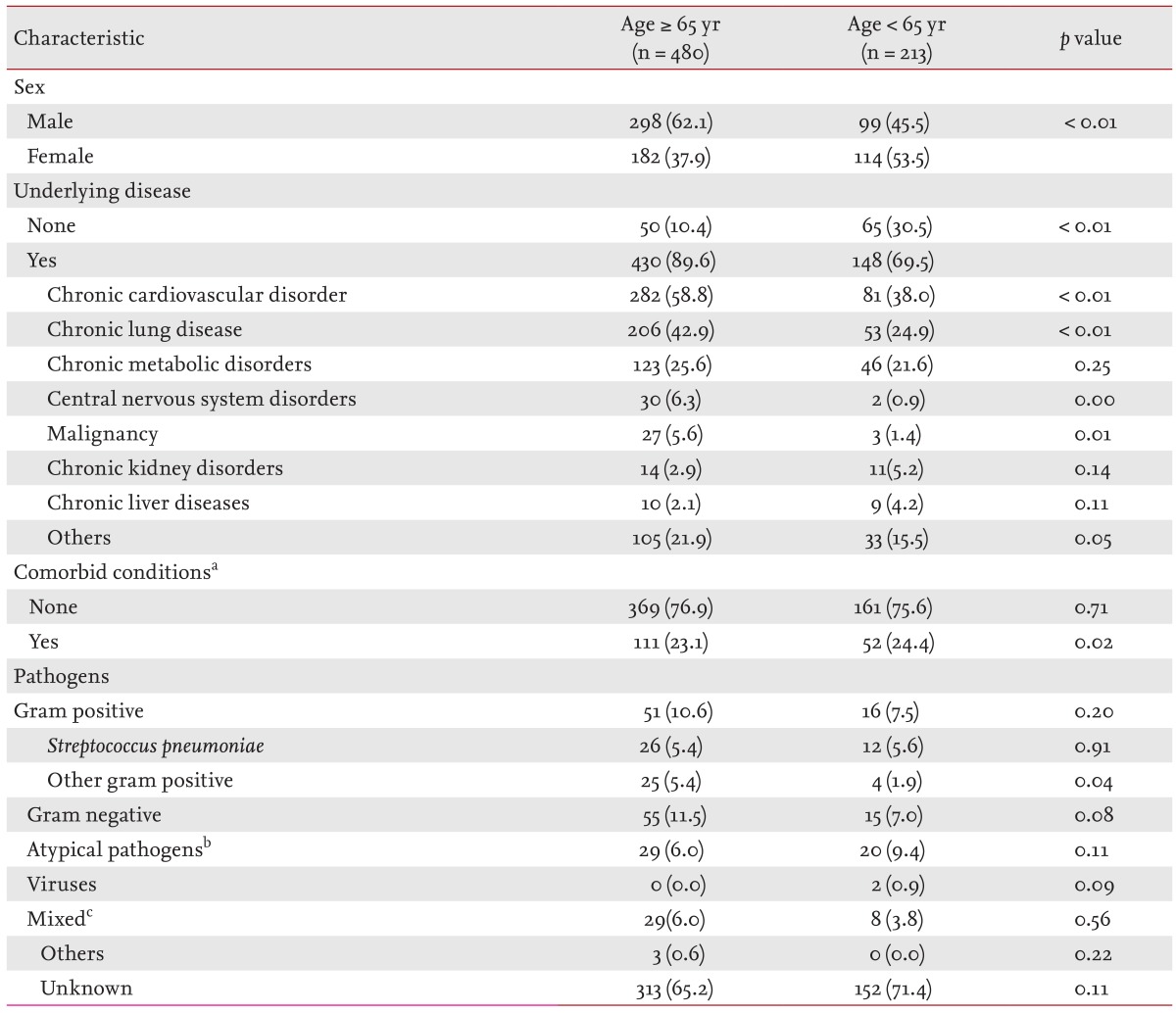
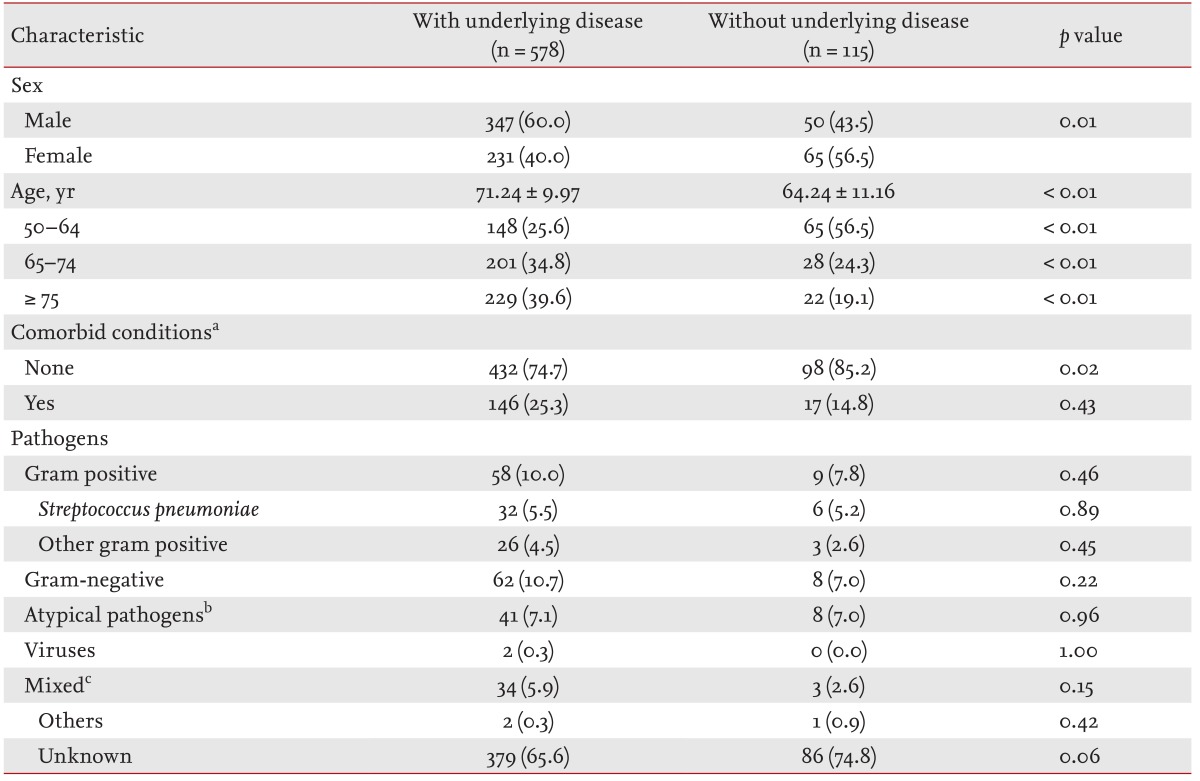
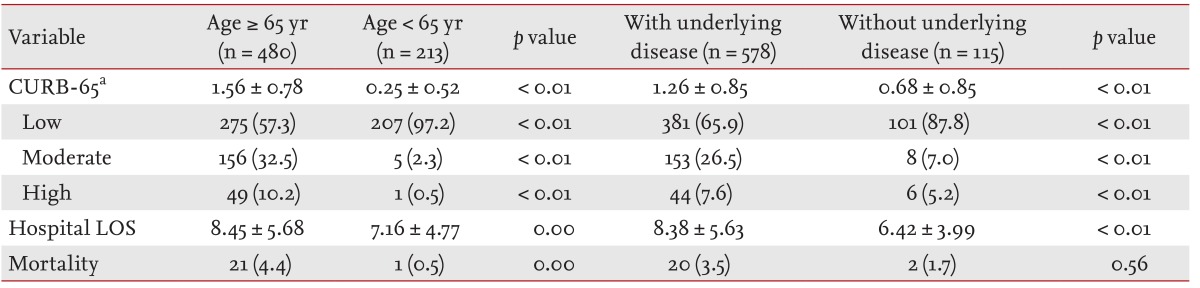
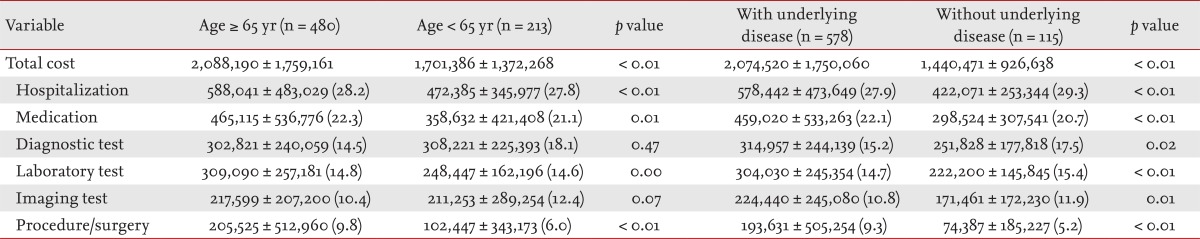
10]. In the current study, we focused on disease burden measured by total per-capita medical fees, severity (CURB-65), hospital LOS, and mortality, according to age and underlying diseases. Our findings demonstrated that disease burden was higher in the elderly (Ōēź 65 years) and in patients with an underlying disease compared to those aged 50 to 64 years or without an underlying disease.
A cost analysis for pneumonia across studies is challenging due to differences in coding and data sources for the definition of pneumonia as well as the analytical methods used to calculate costs [
1,
5,
13,
14,
15,
16]. According to a US pneumonia burden study, the mean LOS per hospital admission was 7.6 days, with a mean cost of US $6,949 per person (1997 value) [
5]. This is consistent with the results of the retrospective analysis by Niederman et al. [
16], who reported that mean hospital LOS and cost were 7.8 days and US $7,166 per person (1995 value) in patients > 65 years of age [
16]. The overall annual hospital cost for CAP in elderly patients in the US is $4.4 billion to $4.8 billion [
5,
16]. A US pneumonia cost analysis of hospital-treated pneumonia as a primary diagnosis in the elderly population in 2010, reported a conservative estimate of > US $7 billion, or US $9,749 per person (2005 to 2007 value); this imposes a tremendous burden on the US healthcare system [
14]. However, those studies relied on Medicare administrative claims for the cost analysis, and the subjects selected may not have provided the actual costs of care. Additionally, limited clinical details of each individual were provided. This suggests the costs may have been overestimated as a result of inclusion of treatments unrelated to pneumonia or unobserved morbidities. In contrast, the costs in our study included both insured and uninsured charges for each medical resource item. Furthermore, we consistently applied the actual cost case by case when a difference existed between hospitals, particularly for uninsured charges. In contrast to these previous studies, which used only the International Classification of Diseases code to select subjects, the definition of pneumonia in our study was clear due to the diagnosis being confirmed by pulmonary specialists in tertiary teaching hospitals. In support of these results, another US study reported that the mortality rate can change according to the pneumonia disease coding used [
17]. Few studies in Asia have determined whether the CAP economic burden can be compared with that of other regions. In Taiwan, the cost of one hospital admission and the total cost for CAP in the elderly were approximately US $3,221 and US $1,897,137, respectively [
18]. Among all age groups in rural Thailand, the cost of hospitalization for an episode of pneumonia ranges from US $490.80 to US $628.60 [
19]. However, the Thai study used national health insurance claims data only; therefore, selection bias may have existed. Furthermore, the case definition for the inclusion criteria and the cost analysis method were unclear.
In addition to the cost analysis method and disease coding, the population examined is an important factor for a cost analysis study. A multicenter, hospital-based study of the clinical and economic burden of invasive pneumococcal disease (IPD) reported mean direct medical costs of US $7,452 (mean, US $5,404 or US $8,756/case), and no difference between age and risk groups [
20]. Similarly, Weycker et al. [
13] reported that the direct medical cost per case did not differ significantly between risk and age groups (US $15,402 to US $31,849/case) [
13]. The former calculated direct medical costs by adding only IPD-related costs for each subject, whereas the latter involved data from the 2004 Healthcare Cost and Utilization Project Nationwide Inpatient Sample using mean age- and risk-specific charges [
13,
20]. Those results are in agreement with our findings. Total costs for CAP in our elderly and underlying disease groups were significantly higher than in the nonelderly and without underlying disease groups, suggesting that the initial disease severity is an important factor for the cost analysis, as are the cost analysis and disease coding methods. As only subjects with severe disease were included, selection bias could have existed in those studies. Moreover, those studies may have reported considerably higher costs because they did not include actual costs, such as uninsured charges, as in our study. Therefore, our data are more accurate and can be generalized to an inpatient CAP population.
CAP is one of the most common causes of death in the infectious diseases category in Korea, and mortality rates reach 12% to 14%, even with antibiotic use [
21]. A prospective surveillance study conducted in 14 tertiary hospitals in Asian countries (South Korea, China, Taiwan, Hong Kong, India, Singapore, Vietnam, and Philippines; Asian Network for Surveillance of Resistant Pathogens), showed that old age was a risk factor for mortality [
11]. In fact, when patients were stratified by age, the mean CURB-65 severity score increased gradually with age (50 to 54 years, 0.16; 55 to 59 years, 0.30; 60 to 64 years, 0.29; 65 to 70 years, 1.40; data not shown) as in our study. Furthermore, the percentage of patients with a high CURB-65 score also increased markedly starting at age 65 yr (50 to 54 years, n = 0 [0%]; 55 to 59 years, n = 0 [0%]; 60 to 64 years, n = 1 [1.3%]; 65 to 70 years, n = 7 [6.9%]; data not shown). This is possibly because the CURB-65 score includes age Ōēź 65 years as a factor in the severity scoring. We divided the patients into elderly (Ōēź 65 years) or nonelderly (50 to 64 years) groups. The elderly group developed a higher disease burden. However, age is itself an important risk or prognostic factor for pneumonia. Age was not a predictive factor for mortality in a Korean study conducted to determine predictors of in-hospital mortality in patients with severe CAP who required mechanical ventilation [
22]. Therefore, severity is more important than age in terms of mortality.
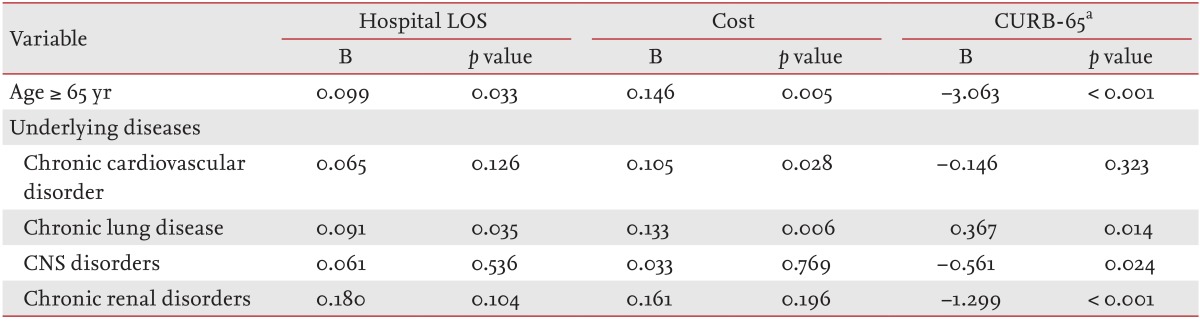
Because we defined the costs for disease burden, severity (CURB-65), hospital LOS, and mortality, we identified the variables associated with these factors. Cost and hospital LOS were significantly higher in the elderly and in patients with an underlying disease; however, no significant association with any variable was found in the multivariate analysis (data not shown). This might have been caused by a lower or slightly higher mortality rate in those with an underlying disease or the elderly. Although we cannot explain the low mortality, several factors are likely involved, such as the modest effect of higher pneumococcal vaccination rates on pneumonia risk; reduced smoking; and better treatment for chronic underlying disease; these are risk factors for pneumonia. Pooled data from observational studies have demonstrated the overall burden of CAP in patients with other medical conditions, such as chronic respiratory diseases, cardiovascular diseases, cerebrovascular diseases, dementia, and diabetes mellitus, which were the most frequent underlying diseases [
3,
23]. Up to two-thirds of patients had a chronic respiratory disease and almost half had a chronic cardiovascular disease [
3,
6,
23]. Our results also indicate that ~90% of those with an underlying disease had chronic cardiovascular disease (52.4%, n = 363) or chronic lung disease (37.4%, n = 259). Disease severity and frequency of an underlying condition affected the outcomes. Mortensen et al. reported that about half of deaths in patients with CAP were attributable to worsening of a pre-existing condition [
24]. Although we cannot explain these factors separately, we understand that age and underlying disease are important factors for predicting disease burden. An analysis of each individual patient with an underlying disease and a longitudinal assessment of outcomes are needed to better understand the associations between age and underlying disease, cost, disease severity, and hospital LOS. Some limitations of this investigation should be mentioned. As our study was performed in a tertiary referral center and did not include an outpatient population, in which CAP is treated more commonly, it is difficult to generalize our results. Another limitation of our study is that only subjects age Ōēź 50 years were included; thus, our results may not be representative of the entire population of pneumonia patients in Korea.
The strengths of this study are the accuracy of the cost analysis for inpatient CAP. Due to the lack of information about the most frequent independent risk factors (elderly, patients with underlying disease) in Korea, we analyzed these patients using accurate medical resources, including uninsured items, which had not been applied in previous studies. Insured items were adjusted for annual inflation by consistently applying the 2010 insurance fees for each insurance medical resources. Furthermore, the nursing (or intensive care unit nursing) personnel category was applied by identifying the actual status in each institution. An accurate economic burden for uninsured items was calculated by focusing on publicly available uninsured data, as disclosed on the website of each institution. Although this was a retrospective study, patients with pneumonia at each hospital were identified in reverse temporal order from the treatment completion date (December 31, 2010) and were extracted relatively randomly; hence, little bias existed according to disease severity, age, sex, or the presence of underlying disease. Third, the study was conducted mostly in the pulmonary divisions of university hospitals; thus, the diagnosis of pneumonia and assessment of underlying diseases were accurate. We identified pathogens more aggressively using every possible diagnostic tools such as bronchoscopy, thoracentesis, histology, etc., and assessed treatment outcomes in > 90% of all cases.
In summary, we report herein the characteristics and medical costs of Korean pneumonia patients aged Ōēź 50 years who received inpatient care. Patients were divided into elderly and non-elderly and those with and without an underlying disease. Total costs, hospital LOS, and disease severity were higher in the elderly and in those with an underlying disease than in the non-elderly and those without an underlying disease. Therefore, this disease imposes a considerable on both the individual, particularly the elderly and those with an underlying disease, and society in general. Furthermore, an actual cost analysis regarding all medical resources, including noninsurance charges, is essential; this should be based on an accurate disease diagnosis as well as on the presence of underlying disease, as discussed above. Given that being elderly and having chronic lung disease were associated with a higher disease burden, closer and more careful observations in these populations are essential to improve the outcomes of inpatient treatment of CAP.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





