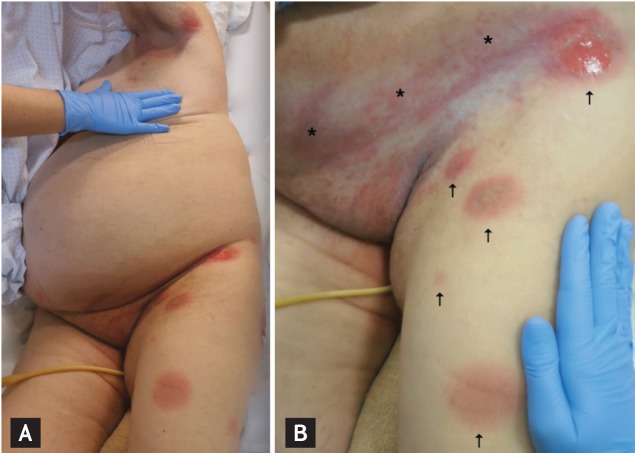
An 81-year-old obese woman was admitted due to decompensated diabetes and a lower urinary tract infection. She was started on empirical antibiotic therapy with ciprofloxacin (750 mg twice daily) and insulin. Dermatological observation was required 48 hours later due to a rash that had been evolving for 24 hours. Physical examination revealed a bilateral and grossly symmetric dermatosis involving the trunk and proximal limbs, comprising a few, round, sharply demarcated erythematous plaques, some of them with a dusky, violaceous hue, central blisters, and a detached epidermis (Figs. 1 and 2). With the exception of flexural superficial candidiasis on the axillary and inguinal folds, no other cutaneous or mucosal lesions were found. The patient recalled a previous similar rash after taking an oral antibiotic (unable to specify which antibiotic), emphasizing that some lesions recurred at the same locations. Admitting the diagnosis of a bullous fixed drug eruption (FDE) to ciprofloxacin, the drug was withdrawn and the lesions resolved with residual grayish hyperpigmentation within 2 weeks. Histopathological examination confirmed the diagnosis, revealing interface dermatitis, epidermal necrosis, scarce neutrophilic pustules, and a perivascular inflammatory infiltrate with eosinophils on the superficial dermis.
FDE usually appears as solitary lesions on the genitalia and acral sites. Commonly implicated drugs include ibuprofen, naproxen, sulfonamides, and tetracyclines. The present case describes a generalized FDE, which is a less common presentation, due to ciprofloxacin, a drug rarely reported to cause FDE. The skin reaction scored 8 points on the Naranjo scale. The absence of mucosal involvement and other symptoms/signs allowed for the exclusion of erythema multiforme and Stevens-Johnson syndrome.
A careful clinical history and skin examination, particularly the pattern of recurrence, are the most valuable clues to diagnose FDE. It is usually a nonserious adverse drug reaction, stopping the offending drug will result in full clinical resolution, and immunosuppressive drugs should generally be avoided. Although FDE is a T-cell-mediated drug hypersensitivity, its pathophysiology is still not fully explained (does not completely fit any of the drug reaction types proposed by World Health Organization).
The typical clinical history, time course, skin findings, and histopathological aspects of the present case made rechallenge an unwise option. Patch testing in a previously involved site may be useful in confirming the responsible drug. Although planned, this was not performed because the patient was lost to follow-up.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





