To the Editor,
Phenytoin is a commonly used antiepileptic drug despite its numerous adverse reactions, such as skin lesions, fever, and lymphadenopathy [1]. Most of the adverse reactions are extrapulmonary, and there have been few reports of acute pulmonary toxicity of the drug [2-4]. We present herein a case of acute bilateral pulmonary infiltration and respiratory failure due to phenytoin intoxication in a patient who attempted to commit suicide with about 50 phenytoin pills.
A 49-year-old man was transferred to the emergency room in a comatose state. He had a history of temporal lobe epilepsy, major depressive disorder with three suicide attempts, and acquired immune deficiency syndrome. He had been taking phenytoin for about 1 year for epilepsy, and the antiretrovirals zidovudine, lamivudine, lopinavir, and ritonavir for 3 months. His latest CD4 count was 461/┬ĄL. Notably, 3 days before the event, the zidovudine had been changed to abacavir because of severe anemia characterized by a hemoglobin concentration of 4.0 g/dL, which had been considered to be a side effect of zidovudine. Because the patient could not afford to be hospitalized, a short-term outpatient departmental follow-up was arranged along with the replacement of zidovudine by abacavir.
Despite the patient's comatose status, his vital signs were all normal on the day of admission. Initial laboratory results were all within the normal range, with the exception of the above-mentioned severe anemia. However, his serum level of phenytoin was higher than 40 ┬Ąg/mL (normal range, 10 to 18). Among the prescribed medications, namely lamivudine, abacavir, lopinavir, ritonavir, vitamin B, and vitamin C, there was no known drug interaction to blame for the increased level of serum phenytoin. As no abnormal findings were observed on a brain computed tomography scan, we suspected that his drowsiness was the result of phenytoin toxicity.
On the second day after admission, the patient presented with fever and developed bilateral pulmonary infiltrates and, subsequently, respiratory failure, which led to intubation and transfer to the intensive care unit. Both his blood pressure and electrocardiography findings remained normal. All microbiology results were negative, including gram staining and culture, acid-fast staining and culture, Mycobacterium tuberculosis polymerase chain reaction (PCR), Pneumocystis jirovecii PCR and direct fluorescence antibody test, and fungal staining and culture. The hepatic enzymes aspartate aminotransferase and alanine aminotransferase were elevated at 1,664 and 1,068 IU/L, respectively. All other biochemical parameters, including bilirubin and alkaline phosphatase, were within their normal ranges.
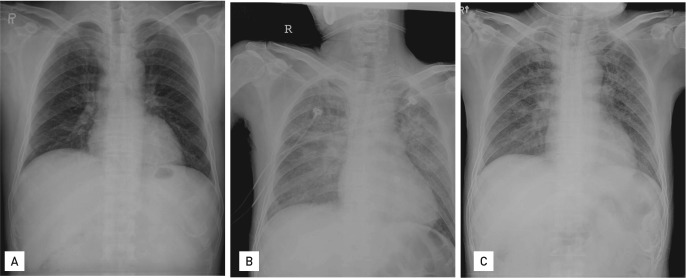
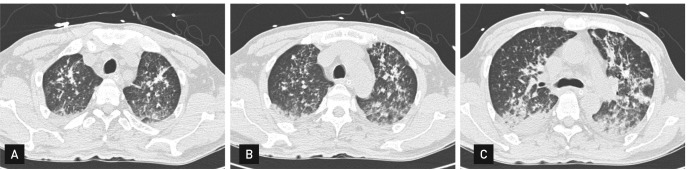
Cefotaxime and trimethoprim-sulfamethoxazole were empirically prescribed for possible pneumonia. Within a few days, the patient's pulmonary infiltrates, level of consciousness, and elevation of aminotransferases markedly improved (Figs. 1 and 2). The serum level of phenytoin remained well above the limit of 40 ┬Ąg/mL for the first 10 days of hospitalization, but declined thereafter. The patient confessed that he had taken about 50 phenytoin pills in a suicide attempt. He was successfully extubated and transferred to the general ward 5 days after admission. Antibiotics were discontinued, and lamivudine, abacavir, lopinavir, and ritonavir were resumed without recurrence of pulmonary infiltrates.
In this case, the initial differential diagnoses for acute bilateral pulmonary infiltrates were atypical pneumonia and aspiration pneumonia. However, the rapid worsening and resolution of the pulmonary infiltrates were not consistent with pneumonia. Indeed, the antibiotics were discontinued not only due to the unusual clinical course for pneumonia but also because all microbiologic tests were negative. Although abacavir hypersensitivity has also been reported to cause fever, pneumonitis, and hepatitis [5], there was no recurrence of symptoms after reintroduction of that drug. Furthermore, there was no known drug interaction promoting phenytoin toxicity.
In addition, the time course of the symptoms showed a close relationship with the serum levels of phenytoin. The pulmonary infiltrates, drowsiness, and elevated aminotransferases were all aggravated by the ingestion of a toxic dose of phenytoin and improved with its withdrawal. Although phenytoin was not unequivocally proven as the causal agent of the acute bilateral pulmonary infiltrates and respiratory failure, our evidence suggests that it is the most likely culprit in this case.
Adverse reactions to phenytoin have been described since the introduction of the drug in the 1930s. The reactions are mainly extrapulmonary and include gingival hypertrophy, cutaneous reactions such as Stevens-Johnson syndrome, lymphadenopathy, hepatitis, etc. [1]. However, there have been a few reports of pulmonary toxicity, including acute interstitial pneumonitis, lymphocytic interstitial pneumonia, pulmonary fibrosis, chronic eosinophilic pneumonia, bronchospasm, and abnormal pulmonary function [2-4]. Although systemic vasculitis and drug hypersensitivity have been proposed, the mechanism underlying the pulmonary toxicity of phenytoin remains uncertain [2,4].
It is noteworthy that most of the reported pulmonary adverse reactions did not cause acute respiratory failure and typically occurred months to years after starting the drug. There is one report of acute lung injury accompanied by renal failure after only 4 days of phenytoin treatment [4], but our case is unique because it shows that one phenytoin overdose can cause acute respiratory failure with bilateral pulmonary infiltration.
Due to the widespread use of phenytoin in the management of convulsions, clinicians should be aware of the possible development of acute bilateral pulmonary infiltrates and subsequent respiratory failure in response to phenytoin intoxication.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





