 |
 |
| Korean J Intern Med > Volume 29(1); 2014 > Article |
|
Abstract
A 71-year-old male patient was readmitted to our hospital 1 month after discharge because of relapse of abdominal pain. He had been diagnosed with hepatocellular carcinoma (HCC) 1 year prior and had undergone repeated transcatheter arterial chemoembolization and radiotherapy. During the last hospitalization, he was diagnosed with a liver abscess complicated by previous treatments for HCC and was treated with intravenous antibiotics and abscess aspiration. Follow-up abdominal computed tomography revealed a liver abscess with a duodenal fistula, which was successfully treated with endoscopic Histoacryl injection into the fistula. Liver abscesses with duodenal fistulas rarely occur, but they are intractable and possibly fatal in patients with HCC. In the literature, they have frequently been managed only with abscess treatment without fistula management. We herein report the first case of a patient with a liver abscess complicated by a fistula between the duodenum and the abscess, which was treated with endoscopic Histoacryl injection.
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide, especially in Asian countries [1]. Although the mainstay of therapy is surgical resection, the majority of patients are not treated by surgery because of the tumor extent or underlying liver dysfunction [2]. Instead of surgical resection, several treatments have been developed, including radiofrequency ablation (RFA), transcatheter arterial chemoembolization (TACE), and radiation therapy (RT). TACE has become the main treatment modality, especially in cases of intermediate-stage HCC [2,3]. However, repeated TACE or combination therapy with RT is often needed to control tumor progression [2-4]. As TACE has become more widely used, many complications have occurred [3,5]. The most common complication is postembolization syndrome (60% to 80% of cases). Serious complications are acute liver failure (7.5%), acute renal failure (1.8%), encephalopathy (1.8%), ascites (8.3%), upper gastrointestinal bleeding (3.0%), and hepatic or splenic abscess formation (1.3%) [5]. Among these complications, hepatoduodenal fistula is a rare but serious problem that can occur after TACE. We describe herein a case of hepatoduodenal fistula caused by an abscess after repeated TACE combined with RT, which was successfully treated with endoscopic Histoacryl injection.
A 71-year-old male patient was readmitted to our hospital 1 month after discharge because of relapse of abdominal pain. One year prior, he had been diagnosed with HCC associated with chronic hepatitis B. He could not undergo surgical resection because of invasion of the hepatic and main portal veins. Therefore, he underwent TACE as a palliative treatment. Although he underwent five sessions of TACE over 10 months, newly viable HCC was found in the left lobe of the liver with thromboses of the portal vein, hepatic vein, and inferior vena cava. Palliative RT was administered to the HCC in the left lobe of the liver and area of left portal vein thrombosis using a dose of 33 Gy comprising daily doses of 3 Gy. He then underwent two additional TACE sessions. One month after the seventh TACE session, the patient presented to our institution with a complaint of persistent abdominal pain. He also had intermittent fever, chills, and weight loss. Abdominal computed tomography (CT) showed a gas-containing cavity suggestive of an abscess within a necrotic mass in the left lateral segment of the liver (Fig. 1A). He was hospitalized, received intravenous empirical antibiotics, and underwent ultrasound-guided abscess aspiration, which produced 0.5 mL of turbid yellowish fluid with a foul odor. Percutaneous drainage catheter insertion was difficult because of the small size of the abscess pocket. Prevotella oralis and Clostridium bifermentans/sporogenes were isolated from the aspirated specimen. The patient's symptoms, including abdominal pain, fever, and chills, resolved completely after 2 weeks of intravenous antibiotic therapy, and he was discharged with oral antibiotics. Although he continued to take oral antibiotics, his abdominal pain recurred only 2 weeks after discharge, and the frequency of abdominal pain gradually increased. He was readmitted to our hospital 1 month after discharge. He complained of persistent abdominal pain; however, other generalized symptoms, including fever and chills, did not reappear. On physical examination, right upper quadrant tenderness was observed, and his serum C-reactive protein level was higher than that during the previous hospitalization. Follow-up CT was performed. Although the abscess had decreased in size, we detected a new communication between the remaining abscess and the duodenal bulb (Fig. 1B). He received total parenteral nutrition and broad-spectrum antibiotics. Gastroduodenoscopy was performed to confirm the fistula through a 0.3-cm hole in the proximal portion of the duodenal bulb (Fig. 2A). At that time, endoscopic clipping was attempted to close the fistula opening. Follow-up endoscopy was performed 2 days after clipping; however, there was still a fistula opening beside the clips (Fig. 2B). The next approach to the fistula was by endoscopic retrograde cholangiopancreatography (ERCP). A ~1-cm fistulous tract was confirmed by guidewire insertion from the fistula hole of the duodenal lumen. A 1:3 mixture of Histoacryl and lipiodol solution (0.5 mL) was injected into the fistula. Follow-up endoscopy performed 2 days after this intervention revealed that the previous fistula orifice was filled with Histoacryl (Fig. 2C). The patient was then discharged from the hospital because he had no abdominal pain after starting oral intake. One month after the intervention, a follow-up abdominal CT scan showed obliteration of the fistulous tract and a decrease in the extent of the abscess (Fig. 1C). Eight months later, he underwent four sessions of additional TACE without abscess recurrence (Fig. 3). The most recent CT scan, taken 7 months after Histoacryl injection, showed advanced HCC without abscess or fistula formation. The patient is still alive and has been followed up at the outpatient clinic.
Hepatoenteric fistulas are rare complications of palliative treatments for HCC. Only a few cases have been reported in the literature [3,6-9]. Three mechanisms of hepatoenteric fistula formation have been suggested. In the f irst mechanism, a f istula is formed by the spread of inflammation from an inadequately treated liver abscess in cases of fistulas that form secondary to a liver abscess [9]. TACE is a widely used treatment option for unresectable HCC. This chemoembolization causes ischemic damage to the surrounding liver tissue and induces tumor necrosis, subsequently resulting in abscess formation by secondary bacterial infection in about 0.2% to 1.1% of all patients [3,10]. In the second mechanism, in cases of a direct perforation of the adjacent bowel by sharp electrodes during RFA or a delayed perforation by thermal injury during RFA, infection is caused by the leakage of bowel contents, resulting in a fistula or abscess [6,8]. Finally, in the third mechanism, a fistula is formed after treatment of direct invasion of the gastrointestinal tract by advanced HCC [7]. In our patient, the f istula was detected 1 month after abscess treatment; therefore, the mechanism of the fistula appears to be liver abscess formation. In particular, the combination of TACE and RT caused more severe ischemic damage to the tumor and surrounding liver tissue. The risk of abscess formation is higher in combination therapies than in TACE alone [4]. In our patient, the abscess developed at the site of the previous RT.
If a hepatoenteric fistula that formed during HCC treatment is not completely treated, it will become a cause of recurrent ascending infection and intractable liver abscess formation, which deteriorate liver function. Furthermore, it can shorten the life expectancy of the patient because of a delay in appropriate treatment of HCC. Therefore, early diagnosis and treatment of hepatoenteric fistulas is vital.
In the literature, most patients with fistulas have complained of abdominal pain after an initial symptom-free period, and persistent fever and chills have been seen in some patients (Table 1). The exact mechanism of pain in these patients is unknown. However, the symptoms usually disappear in patients treated for the abscess without repairing the fistula. Thus, the abscess, rather than the fistula itself, is a more probable cause of the abdominal symptoms.
For early diagnosis of liver abscess or fistula formation, clinicians should be alert for patients complaining of such symptoms and should immediately perform contrast-enhanced CT [3].
There is no standard treatment for hepatoenteric fistula. In most previous reports, conservative treatment with intravenous antibiotics and percutaneous catheter drainage (PCD) was preferred [6,9]. However, there have been few reports of abscess drainage and surgical fistulectomy [3]. When only an abscess is treated, the fistula remains, and in some cases, it causes recurrent infection or secondary complications such as massive gastrointestinal bleeding [7]. Therefore, aggressive treatment such as surgical excision of the fistula is needed; however, excision is usually difficult because patients have decreased liver function and poor performance. In addition, the benefit from surgery is likely to be limited due to the short life expectancy of patients with advanced HCC. In our patient, a nonsurgical approach was attempted first because of the inoperability of the fistula due to the advanced HCC state and residual poor liver function. Initially, endoscopic clipping was performed to close the fistula opening, but this failed. Histoacryl was then injected into the fistula endoscopically and was successful in treating the fistula. Treatment of an abscesso-colonic fistula caused by RFA with Histoacryl injection through a percutaneous catheter during fistulography has been reported [8]. In our case, a percutaneous catheter could not be inserted because of the small size of the abscess. Instead of fistulography, ERCP was performed to visualize the fistula and inject the Histoacryl.
In conclusion, although hepatoenteral fistula formation after treatment of HCC is a rare complication, it can be intractable and fatal. For early diagnosis of fistulas, clinicians should be alert for symptoms such as persistent fever and abdominal pain after an initial symptom-free period. If a fistula is identified, Histoacryl injection should be considered as an alternative to major surgical intervention for treatment. Endoscopic Histoacryl injection can be a useful treatment choice, especially if PCD is difficult to insert because of the small size or location of the abscess.
References
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90PMID : 21296855.


2. Lee JS. Advances in the treatment of hepatocellular carcinoma. Korean J Med 2009;77:290–297.
3. Wang CY, Leung SW, Wang JH, Yu PC, Wang CC. Delayed spontaneous hepatogastric f istula formation following transcatheter arterial embolisation and radiotherapy for hepatocellular carcinoma. Br J Radiol 2009;82:e105–e107PMID : 19451307.


4. Meng MB, Cui YL, Lu Y, et al. Transcatheter arterial chemoembolization in combination with radiotherapy for unresectable hepatocellular carcinoma: a systematic review and meta-analysis. Radiother Oncol 2009;92:184–194PMID : 19042048.


5. Marelli L, Stigliano R, Triantos C, et al. Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol 2007;30:6–25PMID : 17103105.


6. Park SG, Park SJ, Koo HS, et al. Biliary-duodenal fistula following radiofrequency ablation therapy for hepatocellular carcinoma. Korean J Gastroenterol 2008;51:199–203PMID : 18451695.

7. Park H, Kim SU, Choi J, et al. Hepatogastric f istula caused by direct invasion of hepatocellular carcinoma after transarterial chemoembolization and radiotherapy. Korean J Hepatol 2010;16:401–404PMID : 21415585.



8. Kim JY, Kwon YH, Lee SJ, et al. Abscesso-colonic fistula following radiofrequency ablation therapy for hepatocellular carcinoma: a case successfully treated with Histoacryl embolization. Korean J Gastroenterol 2011;58:270–274PMID : 22113044.


Figure 1
Serial contrast-enhanced computed tomography findings. (A) A gas-containing cavity is seen, suggestive of an abscess within a necrotic mass in the left lateral segment of the liver. (B) Communication between the liver abscess cavity and the duodenal bulb is present (arrows). (C) The fistulous tract is obliterated and the extent of the abscess has decreased.

Figure 2
Endoscopic findings. (A) The fistula orifice is seen at the proximal portion of the duodenal bulb. (B) The fistula opening remains visible beside the clips. (C) The fistula orifice is filled with Histoacryl after Histoacryl injection.
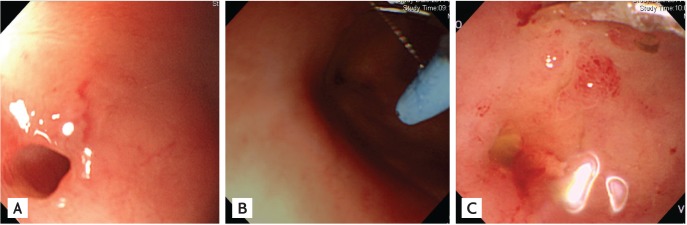
Figure 3
The clinical course of the patient from the time of hepatocellular carcinoma (HCC) diagnosis.
RT, radiation therapy; TACE, transcatheter arterial chemoembolization.
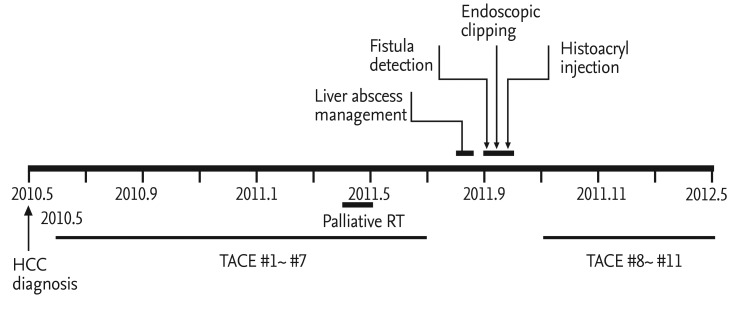
Table 1
Review of cases of hepatocellular carcinoma with hepatoenteric fistula

HCC, hepatocellular carcinoma; RFA, radiofrequency ablation; RUQ Td, tight upper quadrant tenderness; TACE, transcatheter arterial chemoembolization; RT, radiation therapy; CTx, systemic chemotherapy; TAE, transarterial embolization.
aAt the time of fistula diagnosis.
bVascular invasion or extrahepatic metastasis of HCC at the time of fistula diagnosis.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



