 |
 |
| Korean J Intern Med > Volume 28(1); 2013 > Article |
|
To the Editor,
Implantation of drug-eluting stents at atherosclerotic ostial lesions of the coronary arteries is currently considered a reasonable treatment strategy, and sirolimus-eluting stents (SESs) have been widely used for intervention in ostial lesions. There have been several reports of SES migration after stent fracture [1,2]. However, SES migration without fracture is very rare. We describe a patient who experienced migration of a SES without fracture from the ostium of the left main coronary artery (LM) to the right deep femoral artery (RDFA).
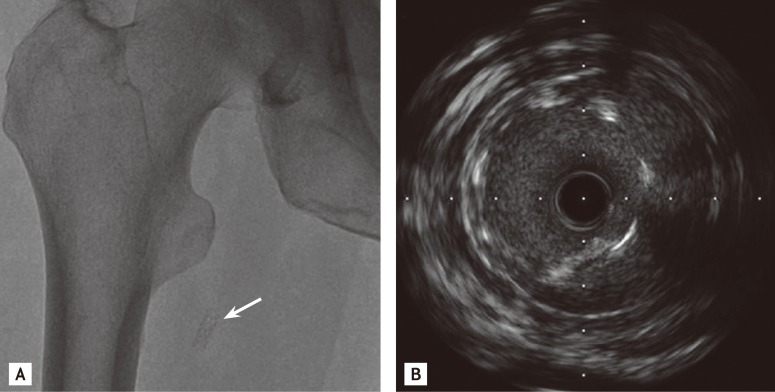
A 67-year-old male presented with complaints of exertional dyspnea and chest discomfort to our cardiovascular center in April 2011. He had coronary risk factors including hypertension and an episode of treatment with percutaneous coronary intervention (PCI) with a 3.5 × 13 mm SES (Cypher, Cordis, Johnson & Johnson, Miami Lakes, FL, USA) at the ostium of the LM 2 years earlier. At that time, coronary angiography (CAG) revealed an 80% stenosis at the ostium of the LM (Fig. 1A), and the minimal luminal area was 4.2 mm2 on intravascular ultrasound (IVUS) (Fig. 1B). The lesion was predilated by a 3.5 × 10 mm balloon inflated at 10 atmospheric pressure (atm), and an SES was deployed at a pressure of 18 atm. Adjuvant balloon angioplasty was performed at a pressure of 20 atm. Thereafter, both CAG and IVUS showed optimal stent expansion and apposition to the vessel wall (Fig. 1C and 1D). Two years later, cardiac computed tomography performed at his hospital visit with symptoms revealed the absence of the SES in the LM, and the SES was found in the RDFA on fluoroscopy (Fig. 2A). IVUS performed in the RDFA showed a decreased stent area at the proximal edge of the migrated SES (Fig. 2B). CAG showed a 90% stenosis at the ostium of the LM, and the minimal luminal area of the LM was 4.0 mm2 on IVUS. Therefore, a 3.5 × 8 mm biolimus A9-eluting stent (Biomatrix, Biosensors Interventional Technologies Pte Ltd., Singapore) was placed at the ostial lesion in the LM. The patient was discharged 2 days after PCI without complications.
Recently, there have been several reports related to SES migration after stent fracture [1,2]. However, migration of SES at the ostium of the LM without fracture has to our knowledge been reported only rarely [3], and the incidence is not available. Several factors may contribute to migration of SES placed at an ostial lesion of the LM. At the ostium of the LM, implanted stents might be affected by perpendicular shear stress caused by blood flow or mechanical forces due to vessel movement during the cardiac cycle. Torsional stress also might be important with respect to stent deformation. Additionally, the effects of mechanical stress on an implanted stent are thought to vary depending on the stent design because differences of strut thickness and mesh architecture would alter the shape of the cells and the links [4]. Since SES have thick struts, dense links, and a wavy open mesh that can be compressed easily, it might be possible to show some plastic deformation after exposure to torsional stress. In our case, IVUS showed optimal stent expansion and apposition to the vessel wall of the LM after SES implantation. However, IVUS performed in the RDFA showed a decreased stent area with a deformed proximal edge of the migrated SES. We believe that contributory factors to SES migration include hinge stress, the shortening of post-dilatation, and the lack of neointimal growth [5]. We performed secondary PCI of the LM with Biomatrix because this stent has several advantages such as quadrature-link design for increased flexibility, a biodegradable polymer, and proven ability in stent placement after SES migration.
This case indicates that SES implantation for ostial lesions in the LM should be performed with great care, and coronary stents that have more flexible designs might be necessary for implantation in LM ostial lesions.
References
1. Eshtehardi P, Ghassemi-Kakroodi P, Mousavi N, Garachemani A, Moayed DA. Complete fracture and migration of a coronary sirolimus-eluting stent. J Cardiovasc Med (Hagerstown) 2011;12:271–273PMID : 20671570.


2. Kamura A, Kawasaki T, Koga N, Inoue T, Node K. Fracture of a sirolimus-eluting stent with migration. Int J Cardiol 2008;130:e86–e88PMID : 18258316.


3. Kubota T, Ishikawa T, Miyamoto T, Mutoh M. Asymptomatic migration of a sirolimus-eluting stent into the aorta. Intern Med 2010;49:2021–2022PMID : 20847511.


Figure 1
Pre- and postintervention imaging findings. (A) Coronary angiography (CAG) demonstrating tubular eccentric 80% stenosis at the proximal portion of the left main coronary artery (LM). (B) Intravascular ultrasound (IVUS) demonstrating significant luminal narrowing of the proximal portion of the LM. (C) CAG demonstrating well-expanded sirolimus-eluting stent in the LM. (D) IVUS demonstrating optimal stent expansion and apposition to the vessel wall at the ostium of the LM.
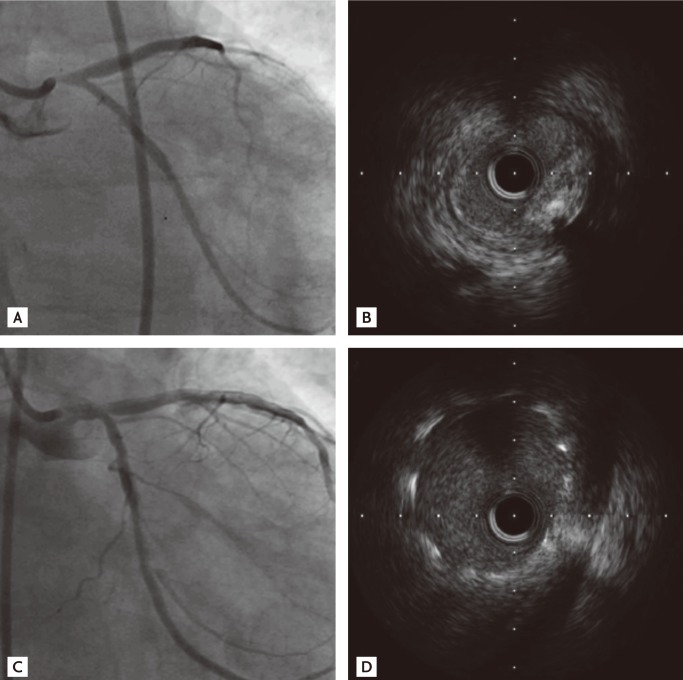
Figure 2
Migrated coronary sirolimus-eluting stent (SES) in the right deep femoral artery (RDFA). (A) A lower extremity fluoroscopy demonstrating the SES (arrow) that had migrated from the left main coronary artery to the RDFA. (B) Intravascular ultrasound performed in the RDFA demonstrating decreased stent diameter and area with deformation of the proximal edge of the migrated SES.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



