 |
 |
| Korean J Intern Med > Volume 28(1); 2013 > Article |
|
Abstract
Background/Aims
The causes of functional anorectal outlet obstruction (outlet obstruction) include functional defecation disorder (FDD), rectocele, and rectal intussusception (RI). It is unclear whether outlet obstruction is associated with rectal hyposensitivity (RH) in patients with functional constipation (FC). The aim of this study was to determine the association between RH and outlet obstruction in patients with FC.
Methods
This was a retrospective study using a prospectively collected constipation database, and the population comprised 107 patients with FC (100 females; median age, 49 years). We performed anorectal manometry, defecography, rectal barostat, and at least two tests (balloon expulsion test, electromyography, or colon transit time study). RH was defined as one or more sensory threshold pressures raised beyond the normal range on rectal barostat. We investigated the association between the presence of RH and an outlet obstruction such as large rectocele (> 2 cm in size), RI, or FDD.
Results
Forty patients (37.4%) had RH. No significant difference was observed in RH between patients with small and large rectoceles (22 [44.9%] vs. 18 [31%], respectively; p = 0.140). No significant difference was observed in RH between the non-RI and RI groups (36 [36.7%] vs. 4 [30.8%], respectively; p = 0.599). Furthermore, no significant difference in RH was observed between the non-FDD and FDD groups (19 [35.8%] vs. 21 [38.9%], respectively; p = 0.745).
Functional constipation (FC) results from slow colonic transit and/or outlet obstruction, although many patients have neither, and some fulfill criteria for both. A rectocele > 2 cm in depth may cause functional anorectal obstruction that presents as FC [1]. The causes of functional anorectal outlet obstruction also include paradoxical contraction or inadequate relaxation of the pelvic muscles during attempted defecation (dyssynergic defecation) or luminal obstruction (rectal intussusceptions, RI) [2].
Rectal hyposensitivity (RH) has been reported in 18% to 68% of patients with FC [3]. Functional anorectal obstruction may be associated with RH in patients with FC, although it is unclear whether RH is an etiology for or a consequence of functional anorectal obstruction [3]. Straining and excessive pelvic floor descent is commonly seen in patients with functional anorectal outlet obstruction. These events may cause stretching of the pudendal or hindgut autonomic nerves, resulting in neuropathy [4], which could precipitate RH [5].
The aim of this study was to investigate RH in patients with FC to determine whether there was an association between RH and functional anorectal obstructions such as rectocele, RI, or dyssynergic defecation.
We selected subjects from the constipation database of Soonchunhyang University Hospital. This database provides comprehensive information regarding constipation and/or fecal incontinence. Eligible subjects had the following: 1) findings compatible with FC (Rome III criteria); 2) no evidence of fecal incontinence; 3) defecographic diagnosis of rectocele regardless of its size; 4) rectal sensitivity determined by anorectal barostat; and 5) each had been subjected to anorectal manometry (ARM) and at least two anorectal physiological tests (balloon expulsion test, electromyography, or colon transit time [CTT] study). We identified 107 patients (100 females) referred for investigation of FC and rectocele.
The characteristics of constipation were subdivided into infrequency of defecation (fewer than three bowel movements/week), obstructed defecation, and two or more of the following symptoms for at least 25% of the time: excessive straining, a sensation of incomplete evacuation or anorectal obstruction blockage, the need for manual maneuvers to facilitate defecation, or infrequency of defecation and obstructed defecation.
Clinical histories were evaluated to identify events or conditions that may have caused RH.
All patients were requested to fast from midnight and to evacuate their bowels on the morning of the experimental day. The barostat device consisted of an infinitely compliant polyethylene bag catheter (10 cm long, 700-mL capacity; Mui Scientific, Mississauga, ON, Canada) connected to a computer-controlled barostat (Synetics Medical AB, Stockholm, Sweden).
To unfold the bag, 200-mL air was manually injected under controlled pressure (< 20 mmHg), and the catheter was pulled back carefully until its passage was restricted by the anal sphincter. The catheter was then introduced a further 2 cm and fixed. The bag was subsequently deflated, and the catheter was connected to the barostat. During the experiment, subjects were in a prone 10° Trendelenburg position to reduce the gravitational effects of the abdominal organs. A conditioning distension was performed by increasing bag pressure from 0 to 36 mmHg in 4-mmHg increments at 30-second intervals in an attempt to stabilize basal tone, enhance reproducibility, and familiarize subjects with the procedure. Isobaric phasic distensions were then performed at 2-mmHg intervals. Each step lasted 1 minute, followed by a 30-second rest period at 0 mmHg. At 30 seconds during each distension step, subjects were asked to state when they first felt the balloon expanding in their rectum (first sensation, FS), when they first appreciated the sensation, and they needed to open their bowels (urge to defecate, UD), and the sensation at which they were unable to tolerate further balloon inflation (maximum tolerated, MT).
These reference ranges were established using the same barostat method in 39 healthy volunteers (23 females) in our motility laboratory unit beginning in 2007. Based on these data, the upper limits of normal for the three rectal sensory thresholds were FS > 14 mmHg, UD > 24 mmHg, and MT > 36 mmHg. RH was defined as an elevation of any or all of the sensory thresholds. Total RH was defined as elevation of all three sensory threshold pressures above the upper limits of normal.
The rectum was filled with barium paste with the patient in the left lateral decubitus position, and then the patient was seated upright on a specially designed commode before being asked to empty the rectum as rapidly and completely as possible. Plain radiography was taken under fluoroscopic control. Anorectal angles during rest, squeeze, and defecation were measured between the anal canal longitudinal axis and the posterior rectal line, parallel to the longitudinal axis of the rectum. Perineal descent was measured as the vertical distance between the anorectal junction and pubococcygeal line. Anal diameter during defecation was also measured.
Rectocele was defined as any anterior bulge outside the line of the anterior rectal wall occurring during defecation or straining. The size of the rectocele was measured as the vertical distance between the tip of the bulge and the longitudinal axis of the anal canal. We distinguished small (< 2 cm) from large (> 2 cm) rectoceles.
The presence of transverse or oblique in-folding of the rectal wall of > 3-mm thickness, which assumes a funnel or ring-like configuration during straining, represented an intussusception.
Defecographic diagnosis of dyssynergic defecation is based on the anorectal angle at rest and during straining, identification of the puborectalis muscle, anal canal diameter, and the amount of rectal and rectocele emptying. We distinguished three subtypes of dyssynergic defecation, including the anal sphincter type (anorectal angle > 20° and anal canal opening < 15-mm during defecation); the puborectalis type (anorectal angle < 20° with continued indentation of the puborectalis muscle during straining, and anal canal opening > 15-mm during defecation); and the mixed type (anorectal angle < 20° with puborectalis indentation and anal canal opening < 15-mm during defecation).
A 3.5-cm latex balloon filled with 50-mL warm water was placed in the rectum through 3-mm-diameter tubing attached to the balloon. A stopwatch was started, and the attendant left the room to provide privacy for the patient during balloon expulsion. The patient was then asked to expel the device into a toilet and to stop the clock. Inability to evacuate the intrarectal balloon in 1 minute was defined as an attempt with expulsion failure [6].
ARM was performed using conventional or high-resolution ARM. Conventional ARM was performed with a standard low-compliance water perfusion system (0.1-mL/min perfusion rate; Synetics Medical AB) and an eight-channel catheter (Arndofer Medical Specialties Inc., Milwaukee, WI, USA) on its tip. The catheter (4.5-mm external diameter) had four radial channels below the balloon and four spiral channels. The performance protocol included the stationary pull-through technique in 1-cm increments while recording anal canal length, resting anal sphincter pressure, and maximum squeezing pressure. Pressures were recorded using a computerized recording device (Polygram Net, Medtronic Inc., Minneapolis, MN, USA).
High-resolution ARM was performed with a solid-state manometric assembly with 12 circumferential sensors spaced at 1-cm intervals (4.2-mm outer diameter; Sierra Scientific Instruments Inc., Los Angeles, CA, USA). This device uses proprietary pressure-transduction technology (TactArray, Sierra Scientific Intruments Inc.) that allows each pressure-sensing element to detect pressure over a length of 2.5-mm in each of 12 radially dispersed sectors. The catheter was placed in the rectum to record anal canal length, resting anal sphincter pressure, and maximum squeezing pressure. We investigated the presence of a pelvic floor dyssynergia pattern using ARM during attempted defecation.
The CTT study was assessed using the Metcalf method [7]. Subjects ingested a capsule with 20 radioopaque markers (Kolomark, M.I. Tech Co., Ltd., Seoul, Korea) on 3 consecutive days, at 10:00 AM. Abdominal radiographs were obtained 1 day after ingestion of the last capsule, each at the same time in the morning. Markers were counted in the right, left, and rectosigmoid regions, and mean segmental transit times were calculated according to a validated formula described previously [7].
According to the reference ranges used in our motility unit, patients were positive for evidence of incomplete evacuation when the total colonic transit time or segmental rectosigmoid transit time exceeded 56 or 20 hours, respectively.
Surface EMG was performed with a perianal sensor (Perry Elan, SRS Medical Systems, Redmond, WA, USA) and surface electrodes (Perry Elan, SRS Medical Systems). The perianal sensor was placed in the anal canal to monitor muscular activity in the external anal sphincter and puborectalis muscle at rest, during squeezing, and during relaxation. The surface electrodes were attached to the abdominal wall to detect contraction of the abdominal wall muscles. Evidence of inappropriate contraction or failure to relax the pelvic floor muscles during repeated attempts was defined as an increase in EMG activity during straining.
FDD was diagnosed according to the Rome III criteria (diagnostic criteria for FC and evidence of inappropriate contraction or failure to relax the pelvic floor muscles during repeated attempts to defecate, and evidence of incomplete evacuation using ARM, EMG, defecography, BET, and the CTT study).
Contingency tables were analyzed using the chi-square test. Comparisons between groups of nonparametric data were performed using Fisher's exact test. A p value < 0.05 was considered to indicate statistical significance. Data were analyzed using the SPSS version 12.0 software (SPSS Inc., Chicago, IL, USA).
The study population comprised 107 patients with FC and rectocele (100 females [93.5%]; median age, 49 years; range, 24 to 80 years). The most common presenting complaint was obstructed defecation (58.9%, n = 63), followed by infrequency (28%, n = 30), and both infrequency and obstructed defecation (13.1%, n = 14).
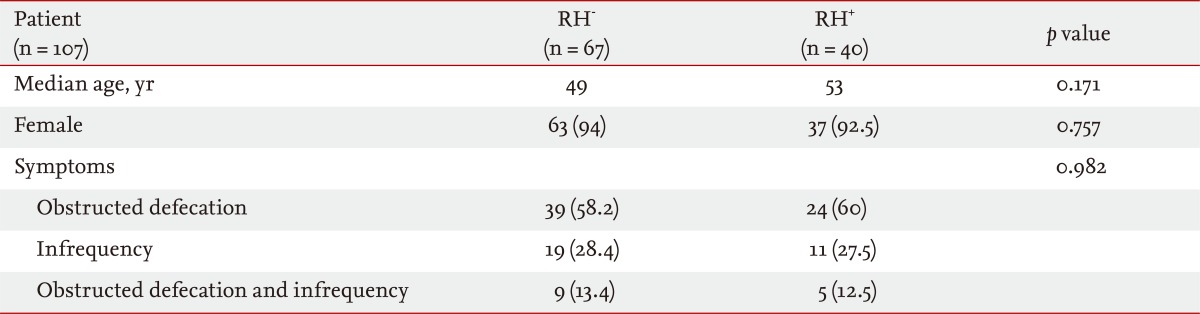
No significant differences were observed in the frequency of RH according to median age, gender, or symptoms (Table 1).
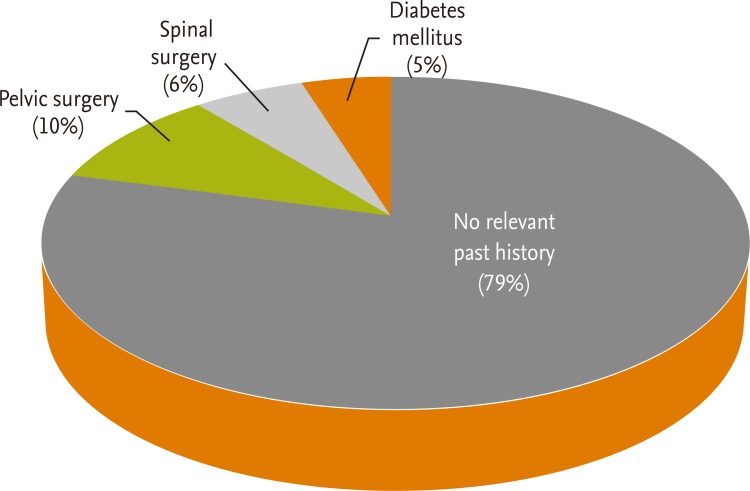
Overall, 21% (23 of 107) of all patients had potential risk factors for development of RH. The most common past events were pelvic surgery (hysterectomy, ovarian surgery, and bladder surgery), followed by spinal surgery and diabetes mellitus (Fig. 1).
The frequency of RH was higher in the patient group (45.5%) with risk factors than in the group (35.3%) without risk factors. However, no significant difference was observed in the frequency of RH according to the presence of risk factors.
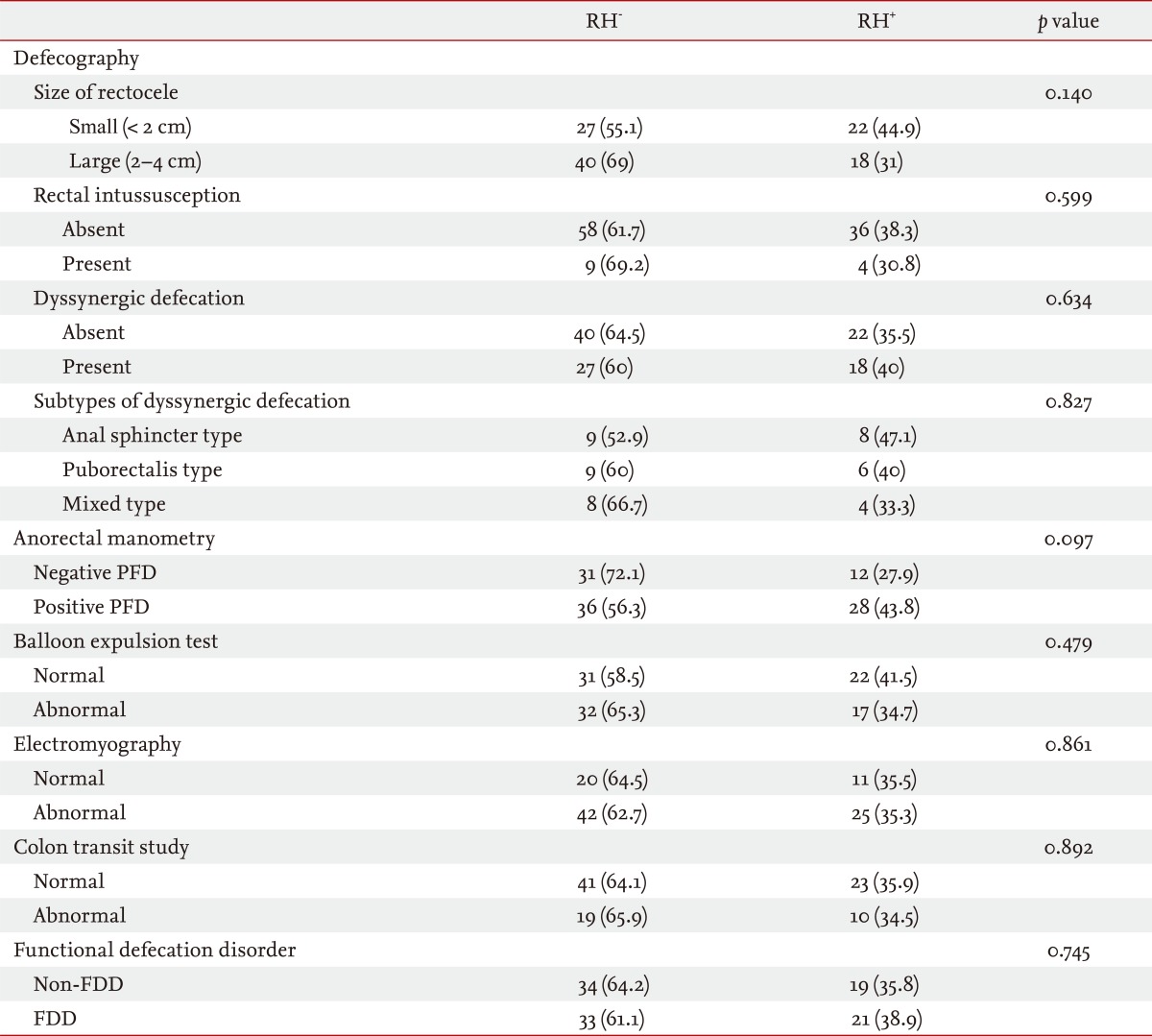
Forty-nine patients (45.8%) had small rectocele (< 2 cm), and 58 (54.2%) had large rectocele (> 2 cm). Overall, 37.4% (40 of 107) of all patients had RH. No significant difference in the frequency of RH according to the size of the rectocele was identified. Thirteen patients (12.1%) had RI. No significant difference in the RH frequency according to the presence of RI was observed. Forty-five patients (42.1%) had a defecographic diagnosis of dyssynergic defecation. The most common subtype of dyssynergic defecation was the anal sphincter type (n = 17), followed by the puborectalis type (n = 15) and the mixed type (n = 13). No significant difference in the frequency of RH according to either the presence or subtype of dyssynergic defecation (defecographic diagnosis) was identified (Table 2).
ARM was performed in all patients and showed pelvic floor dyssynergia in 64 (59.8%). RH was found in 28 (43.8%) patients in the group with pelvic floor dyssynergia on ARM and in 12 (27.9%) of the group with normal ARM. The frequency of RH was not significantly different between the two groups (p = 0.097). Total RH was found in nine (14.1%) patients in the group with pelvic floor dyssynergia on ARM and in one (2.3%) in the group with normal ARM. The frequency of total RH was significantly different between the two groups (p = 0.047).
A BET was performed in 104 (97.2%) of all patients, and it was abnormal in 51 (47.6%). RH was found in 18 (35.3%) patients in the group with an abnormal BET and in 22 (41.5%) in the group with a normal BET. RH frequency was not significantly different between the two groups (p = 0.515). Total RH was found in four (7.8%) patients in the group with an abnormal BET and in six (11.3%) in the group with a normal BET. The frequency of total RH was not significantly different between the two groups (p = 0.548).
EMG was performed in 98 (91.6%) of all patients, and it showed evidence of dyssynergic defecation in 67 (62.6%). RH was found in 25 (37.3%) patients in the group with dyssynergic defecation on EMG and in 11 (35.5%) in the group with a normal EMG. The frequency of RH was not significantly different between the two groups (p = 0.861). Total RH was found in eight (11.9%) patients in the group with dyssynergic defecation on EMG and in two (6.5%) in the group with a normal EMG. The frequency of total RH was not significantly different between the two groups (p = 0.404).
CTT was performed in 93 (86.9%) patients and was abnormal in 29 (27.1%). RH was found in 10 (34.5%) patients in the group with prolonged CTT and in 23 (35.9%) in the group with normal CTT. The frequency of RH was not significantly different between the two groups (p = 0.892). Total RH was found in two (6.9%) patients in the group with prolonged CTT and in six (9.4%) in the group with normal CTT. The frequency of total RH was not significantly different between the two groups (p = 0.693).
FDD was diagnosed in 54 (50.5%) patients. RH was found in 21 (38.9%) patients in the group with FDD and in 19 (35.8%) in the non-FDD group. RH frequency was not significantly different between the two groups (p = 0.745). Total RH was identified in six (11.1%) patients in the group with FDD and four (7.5%) in the non-FDD group. The frequency of RH was not significantly different between the two groups (p = 0.742).
FC may result from diverse pathophysiologies, such as delayed colonic transit and/or pelvic floor dysfunction [8]. RH may also be important in the etiology of constipation in some patients, as it is the only demonstrable physiological abnormality in half of such patients [9]. Normalization of rectal sensory function following biofeedback produces marked improvements in clinical and other physiological parameters [10]. Furthermore, RH, objectively assessed during a physiological evaluation, improves (frequently falling to within the normal limits) in 65% to 92% of patients, although this is not the case in nonresponders [10,11]. These findings suggest a significant relationship between RH and a functional anorectal outlet obstruction. It is not known whether RH assessed by anorectal barostat is associated with a functional anorectal outlet obstruction. The method used to assess RH in most studies is simple balloon distension. Diagnosis on the basis of abnormal threshold balloon distension volumes alone may be inaccurate due to the influence of differing rectal wall properties and volume [12]. This can be overcome by controlling balloon insufflation with a barostat, an electro-mechanical device that delivers isobaric rectal distension using a highly compliant polyethylene balloon. Using this device and proper technique, sensory thresholds are measured independent of rectal volume and compliance [13]. A barostat can distinguish between rectal compliance disorders and afferent sensory dysfunction.
Thus, we measured rectal sensitivity using a barostat in constipated patients to determine the association between RH and functional anorectal outlet obstruction. Our data suggest that the presence of functional anorectal outlet obstruction is unlikely to affect the proportion of RH in constipated patients. In other words, RH is not significantly associated with functional anorectal outlet obstruction, such as FDD, rectocele, or RI. Our results correspond with those of a recent study, which reported that RH is unlikely to be the central cause of obstructed defecation in patients with high-grade internal rectal prolapse [14]. Indeed, it is possible that RH plays a role in the development of FC irrespective of the presence of functional factors, particularly a functional anorectal outlet obstruction.
True RH, impaired rectal afferent pathway function, may result from disruption to any of the following levels of the brain-gut axis [15]: increased rectal mechanoreceptor threshold, abnormal impulse conduction, or altered processing of information in the central nervous system. Observational evidence supports the proposition that alterations in the central processing of afferent information from the rectum, such as activation of pain inhibitory systems or attenuation of central arousal systems, may lead to the development of RH [16,17]. Thus, psychological factors may act at a central level, resulting in RH [18]. It is widely believed that behavior related to defecation, such as habitual suppression, may lead to RH [15,16,19]. In addition, a history of severe sexual/physical abuse may be associated with RH [20].
The cross-sectional design used in this study did not allow for establishing causal relationships. However, the lack of a significant difference in the proportion of RH according to the presence of functional anorectal obstruction suggests that RH and functional anorectal obstruction are not causally linked. A limitation of this study was the inclusion of a large portion of patients who were transferred from community hospitals to our large tertiary hospital. The central response was not evaluated with cerebral evoked potentials, functional magnetic resonance imaging, or position emission tomography scanning in our study population, which might explain the pathophysiological mechanisms of RH.
Our results suggest that the presence of RH should be considered when managing constipated patients with a functional anorectal outlet obstruction, although the optimal treatment for RH is currently not clear. A recent study reported that stapled transanal rectal resection (STARR) is more effective than biofeedback training to resolve obstructed defecation symptoms and improve quality of life in selected patients [21]. Our data provide an explanation for the improved results of STARR, which removes the "hyposensitive" portion of the rectum, in patients with an outlet obstruction associated with RI and rectocele.
In conclusion, our findings suggest that RH and functional anorectal outlet obstruction are common entities but appear not to be significantly associated.
1. The causes of functional anorectal outlet obstruction include functional defecation disorder, rectocele, and rectal intussusception.
2. The gold standard for diagnosis of rectal hyposensitivity is using a barostat.
3. In our study using a barostat, rectal hyposensitivity, and functional anorectal outlet obstruction are common entities but appear not to be significantly associated.
References
1. Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW. Defecography in normal volunteers: results and implications. Gut 1989;30:1737–1749PMID : 2612988.



2. Muller-Lissner S. The difficult patient with constipation. Best Pract Res Clin Gastroenterol 2007;21:473–484PMID : 17544112.


3. Gladman MA, Lunniss PJ, Scott SM, Swash M. Rectal hyposensitivity. Am J Gastroenterol 2006;101:1140–1151PMID : 16696790.


4. Kiff ES, Barnes PR, Swash M. Evidence of pudendal neuropathy in patients with perineal descent and chronic straining at stool. Gut 1984;25:1279–1282PMID : 6094314.



5. Solana A, Roig JV, Villoslada C, Hinojosa J, Lledo S. Anorectal sensitivity in patients with obstructed defaecation. Int J Colorectal Dis 1996;11:65–70PMID : 8739829.


6. Rao SS. Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am 2008;37:569–586PMID : 18793997.



7. Metcalf AM, Phillips SF, Zinsmeister AR, MacCarty RL, Beart RW, Wolff BG. Simplified assessment of segmental colonic transit. Gastroenterology 1987;92:40–47PMID : 3023168.


8. Glia A, Lindberg G, Nilsson LH, Mihocsa L, Akerlund JE. Constipation assessed on the basis of colorectal physiology. Scand J Gastroenterol 1998;33:1273–1279PMID : 9930390.


9. Gladman MA, Scott SM, Williams NS, Lunniss PJ. Clinical and physiological findings, and possible aetiological factors of rectal hyposensitivity. Br J Surg 2003;90:860–866PMID : 12854114.


10. Rao SS, Welcher KD, Pelsang RE. Effects of biofeedback therapy on anorectal function in obstructive defecation. Dig Dis Sci 1997;42:2197–2205PMID : 9398795.


11. Peticca L, Pescatori M. Outlet obstruction due to anismus and rectal hyposensation: effect of biofeedback training. Colorectal Dis 2002;4:67. PMID : 12780659.


12. Lagier E, Delvaux M, Vellas B, et al. Influence of age on rectal tone and sensitivity to distension in healthy subjects. Neurogastroenterol Motil 1999;11:101–107PMID : 10320590.


13. Hammer HF, Phillips SF, Camilleri M, Hanson RB. Rectal tone, distensibility, and perception: reproducibility and response to different distensions. Am J Physiol 1998;274(3 Pt 1):G584–G590PMID : 9530161.


14. Wijffels NA, Angelucci G, Ashrafi A, Jones OM, Cunningham C, Lindsey I. Rectal hyposensitivity is uncommon and unlikely to be the central cause of obstructed defecation in patients with high-grade internal rectal prolapse. Neurogastroenterol Motil 2011;23:151–154PMID : 21108696.


15. Wingate D, Hongo M, Kellow J, Lindberg G, Smout A. Disorders of gastrointestinal motility: towards a new classification. J Gastroenterol Hepatol 2002;17(Suppl):S1–S14PMID : 12000590.

16. Harraf F, Schmulson M, Saba L, et al. Subtypes of constipation predominant irritable bowel syndrome based on rectal perception. Gut 1998;43:388–394PMID : 9863485.



17. Houghton LA. Sensory dysfunction and the irritable bowel syndrome. Baillieres Best Pract Res Clin Gastroenterol 1999;13:415–427PMID : 10580918.


18. Baldi F, Ferrarini F, Corinaldesi R, et al. Function of the internal anal sphincter and rectal sensitivity in idiopathic constipation. Digestion 1982;24:14–22PMID : 7128948.


19. Mimura T, Nicholls T, Storrie JB, Kamm MA. Treatment of constipation in adults associated with idiopathic megarectum by behavioural retraining including biofeedback. Colorectal Dis 2002;4:477–482PMID : 12790924.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



