 |
 |
| Korean J Intern Med > Volume 27(4); 2012 > Article |
|
Abstract
Pseudomembranous necrotizing bronchial aspergillosis (PNBA) is a rare form of invasive aspergillosis with a very poor prognosis. The symptoms are non-specific, and the necrotizing plugs cause airway obstruction. Atelectasis and respiratory failure can be the initial manifestations. Recently, we treated an immunocompromised patient with PNBA, who presented with a sudden onset of atelectasis and acute respiratory failure. There were no preceding signs except for a mild cough and one febrile episode. Bronchoscopy revealed PNBA, and Aspergillus nidulans was cultured from the bronchial wash.
Pseudomembranous necrotizing bronchial aspergillosis (PNBA) is a rare manifestation of Aspergillus infection. Since the first report of this condition in a patient with hemophilia and acquired immune deficiency syndrome [1], most cases have occurred in immunocompromised patients [2], and it is identified in an immunocompetent host only rarely [3]. The clinical manifestations are usually non-specific, and include fever, cough, chest pain, hemoptysis, and dyspnea [4]. On physical examination, wheezing may be a sign of PNBA, since the necrotizing material produced can cause airway obstruction. However, initial suspicion of PNBA is uncommon since wheezing has many other possible causes. Clinicians might thus neglect consideration of PNBA and delay diagnosis, resulting in a poor treatment outcome [2]. Thus, a high index of suspicion and early diagnosis are important. We recently treated an immunocompromised patient with PNBA who presented with a sudden onset of atelectasis and acute respiratory failure.
A 39-year-old female with a diagnosis of acute myeloid leukemia with multi-lineage dysplasia was treated with induction chemotherapy including idarubicin (12 mg/m2 for 3 days) and cytarabin (100 mg/m2 for 7 days). She failed to achieve complete remission, and was referred to our hospital for salvage chemotherapy, which was carried out with a FLAG-Ida regimen (fludarabine 30 mg/m2 for 5 days, cytarabin 2 g/m2 for 5 days, and idarubicin 12 mg/m2 for 3 days, with granulocyte colony-stimulating factor support).
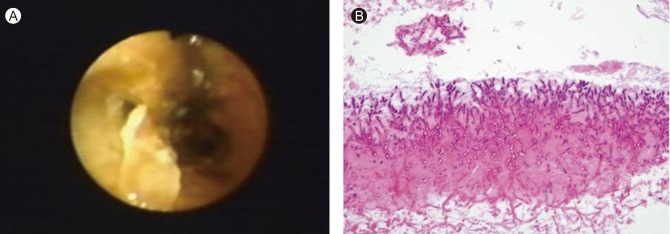
While the patient had neutropenia due to bone marrow suppression after chemotherapy, she had no episodes of febrile neutropenia. On the 21st day after chemotherapy, she complained of a mild cough. There was no fever and her breathing sounds were smooth on auscultation. Two days later the patient developed a fever of 38.3℃; however, her physical examination was unremarkable. We initiated empirical antibiotics, with cefepime 1 g q 12 hours and vancomycin 1 g q 12 hours for febrile neutropenia. Her chest X-ray showed a focal atelectasis (Fig. 1). The following morning, the patient complained of a sudden onset of dyspnea. Her vital signs were as follows: blood pressure 100/60 mmHg, heart rate 102 beats/min, respirations 32/min, and body temperature 37.0℃. By auscultation, breath sounds were nearly absent in the left-lung field. Laboratory findings, including arterial blood gas analysis, showed severe hypoxia and pancytopenia: pH 7.47, PaCO2 29.9 mmHg, PaO2 32.5 mmHg, HCO3 21.3 mmol/L, saturation 67.7%, hemoglobin 7.4 g/dL, white blood cell count 100/µL, absolute neutrophil count 0/µL, and platelet count 25,000/µL. Chest X-rays showed a diffuse radiopaque density with volume decrease of the entire left-lung field, suggesting the development of total left-lung atelectasis (Fig. 1). The patient was transferred to the intensive care unit and mechanical ventilator support was provided. Fiber-optic bronchoscopy revealed a large quantity of necrotic material at the distal trachea. The orifice of the left main bronchus was not visible because of a large quantity of grayish necrotic material covering the opening of the main bronchus (Fig. 2A). Bronchoscopic biopsy, at the necrotic membrane, was performed. Due to suspicion of PNBA, we started intravenous administration of amphotericin B (0.5 mg/kg/day for the first day, 0.75 mg/kg/day on the subsequent day, and 1 mg/kg/day for the following 8 days). Serum galactomannan was also positive, with a level of 2.0 (normal range, 0 to 0.5). Biopsy of the necrotic membrane revealed the presence of fungus with hyphae suggestive of Aspergillus (Fig. 2B). In spite of vigorous treatment in the intensive care unit for 5 days, the lung lesions rapidly progressed with worsening hypoxia. This infection was likely associated with the patient's persistent neutropenia, which was characterized by an absolute neutrophil count < 100/µL. We changed the antifungal agent to voriconazole due to the poor response to amphotericin B. Voriconazole was administered at 6 mg/kg q 12 hours for the loading dose and 4 mg/kg q 12 hours for the maintenance dose. However, respiratory distress progressed and the patient died 3 days later. Culture of the bronchial washing yielded Aspergillus nidulans.
Aspergillosis is a common opportunistic infection in immunocompromised patients; it is usually transmitted by the inhalation of spores [5]. Pulmonary aspergillosis is characterized by four major clinical syndromes, as follows: 1) invasive pulmonary aspergillosis, 2) chronic necrotizing aspergillosis, 3) aspergilloma, and 4) allergic bronchopulmonary aspergillosis [5]. PNBA is an unusual clinical form of invasive aspergillosis [4].
Most cases of PNBA occur in patients with a hematologic malignancy. However, some cases are associated with other chronic diseases, including chronic obstructive lung disease, diabetes, and lupus [2]. Therefore, the predisposing factors associated with the occurrence of PNBA include malignancy, AIDS, neutropenia for more than 3 weeks, transplant recipient status, and treatment with immune suppressive and cytotoxic drugs [4]. Acute leukemia and myelodysplastic syndrome with prolonged neutropenia are also risk factors for invasive aspergillosis. Thus, PNBA was a possible etiology, in this patient, from the first signs of respiratory failure and radiological abnormalities. However, her clinical presentation was atypical for PNBA due to the presence of only a mild cough and a small amount of whitish sputum, and only a single febrile episode prior to acute respiratory failure. Thus, the presentation was abrupt and progressed rapidly with no prior signs. When we first noted her acute respiratory failure and abnormal X-ray findings, a massive pulmonary hemorrhage could not be excluded, because of her low platelet count. In a few previous reports of Aspergillus tracheobronchitis, chest radiographic findings showed atelectasis rather than infiltration [6,7]. However, the patients reported previously had preceding signs, including cough, dyspnea, and fever that persisted for a few days, and their clinical courses were not as rapid as that of our case. The present patient did not complain of dyspnea prior to acute respiratory failure. Bronchoscopy is the diagnostic procedure used for PNBA [2]. The most pathognomonic feature is the presence of a well-defined pseudomembrane covering the bronchial tree [8]. Thus, immediate bronchoscopy could facilitate early diagnosis of PNBA.
Among the PNBA cases reported previously, the most common Aspergillus species was Aspergillus fumigates [2,4,7]. A few cases were associated with other Aspergillus spp.: Aspergillus flavus [8], Aspergillus niger [1], and Aspergillus terreus [6]. In our case, A. nidulans was cultured from the bronchial wash fluid. Infections by A. nidulans are relatively rare even in immunocompromised hosts. The standard treatment is aggressive antifungal therapy with amphotericin B, liposomal amphotericin B, voriconazole, or itraconazole [4]. One study reported topical amphotericin B application in patients with bronchial aspergillosis [9]. Recently, novel strategies for the early treatment of invasive fungal infections have been reported [5]. Currently, voriconazole is considered for initial therapy of invasive aspergillosis [5]. A. nidulans and A. terreus are frequently resistant to amphotericin B [10]. Thus, amphotericin B-based treatment could result in failure of treatment for A. nidulans and A. terreus infections.
We used amphotericin B as the initial therapy, and changed to voriconazole due to the patient's poor response. A. nidulans was cultured after the patient died. Although the main treatment is an antifungal agent, penetration into the pseudomembranous necrotizing material is poor, so bronchoscopic removal might be an effective aid to treatment [6]. In this case, bronchoscopic removal was attempted, but failed.
Aspergillus tracheobronchitis is fatal in about 40% of cases despite appropriate therapy; a higher mortality rate, of above 90%, is reported in the PNBA subgroup. Another study reported an overall mortality rate of 80%, and 94% in ventilated patients [2]. This case report illustrates atypical manifestations of PNBA. When sudden atelectasis is found in an immunocompromised patient, especially in association with a hematologic malignancy, physicians should consider the possibility of PNBA, as this might be its initial manifestation.
References
1. Pervez NK, Kleinerman J, Kattan M, et al. Pseudomembranous necrotizing bronchial aspergillosis: a variant of invasive aspergillosis in a patient with hemophilia and acquired immune deficiency syndrome. Am Rev Respir Dis 1985;131:961–963PMID : 4003949.

2. Tasci S, Glasmacher A, Lentini S, et al. Pseudomembranous and obstructive Aspergillus tracheobronchitis: optimal diagnostic strategy and outcome. Mycoses 2006;49:37–42PMID : 16367817.

3. Oh HJ, Kim HR, Hwang KE, et al. Case of pseudomembranous necrotizing tracheobronchial aspergillosis in an immunocompetent host. Korean J Intern Med 2006;21:279–282PMID : 17249514.



4. Patel N, Talwar A, Stanek A, Epstein M. Tracheobronchial pseudomembrane secondary to aspergillosis. J Bronchology 2006;13:147–150.

5. Zmeili OS, Soubani AO. Pulmonary aspergillosis: a clinical update. QJM 2007;100:317–334PMID : 17525130.


6. Routsi C, Kaltsas P, Bessis E, Rontogianni D, Kollias S, Roussos C. Airway obstruction and acute respiratory failure due to Aspergillus tracheobronchitis. Crit Care Med 2004;32:580–582PMID : 14758182.


7. Routsi C, Platsouka E, Prekates A, Rontogianni D, Paniara O, Roussos C. Aspergillus bronchitis causing atelectasis and acute respiratory failure in an immunocompromised patient. Infection 2001;29:243–244PMID : 11545491.


8. Arriero JM, Chiner E, Marco J, Mayol MJ, Serna M. Simultaneous obstructing and pseudomembranous necrotizing tracheobronchitis due to Aspergillus flavus. Clin Infect Dis 1998;26:1464–1465PMID : 9636883.


Figure 1
(A) Subsegmental atelectasis in the left mid-lung zone (arrows). (B) The atelectasis had rapidly progressed on the following day, together with development of left total lung atelectasis.
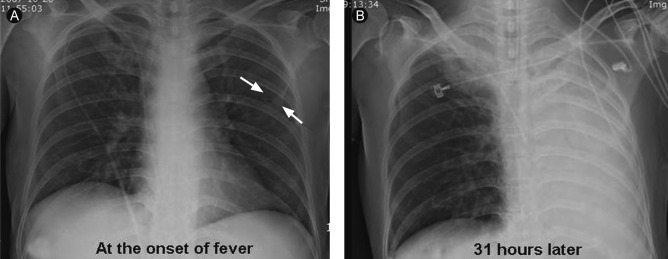
Figure 2
Bronchoscopic appearance of pseudomembranous Aspergillus tracheobronchitis. The opening of the left main bronchus was completely obliterated by mucosal necrotic inflammation; however, (A) the opening of the right main bronchus was intact. (B) Degenerated Aspergillus hyphae were observed (H&E, × 200).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



