INTRODUCTION
Primary aldosteronism is a syndrome characterized by hypertension and hypokalemia [1]. Aldosterone-producing adenomas (APAs) and bilateral idiopathic hyperaldosteronism (IHA) are the most common causes of primary aldosteronism, with APA accounting for approximately 35% of the cases, and IHA accounting for 60% [2]. Aldosterone-producing adrenocortical carcinomas (APACs) are a very rare cause of primary aldosteronism [3]. As a cause of primary aldosteronism, an APAC is characterized by hypertension and hypokalemia [3]; however, very few APACs have features of normotensive primary aldosteronism [4,5]. Here, we report a case of APAC without hypertension.
CASE REPORT
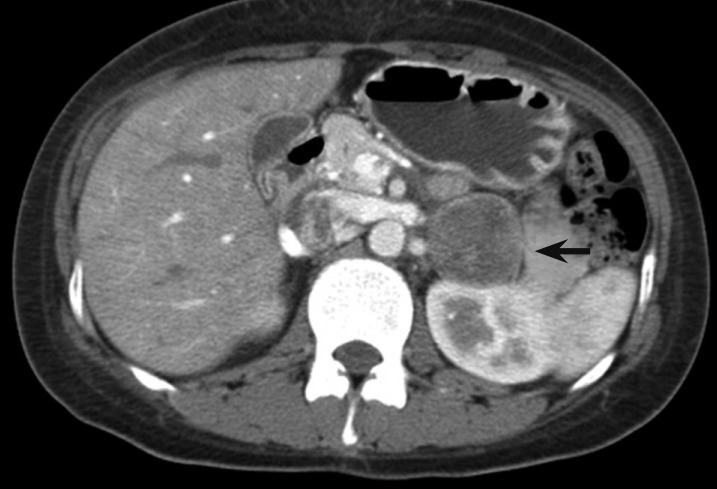
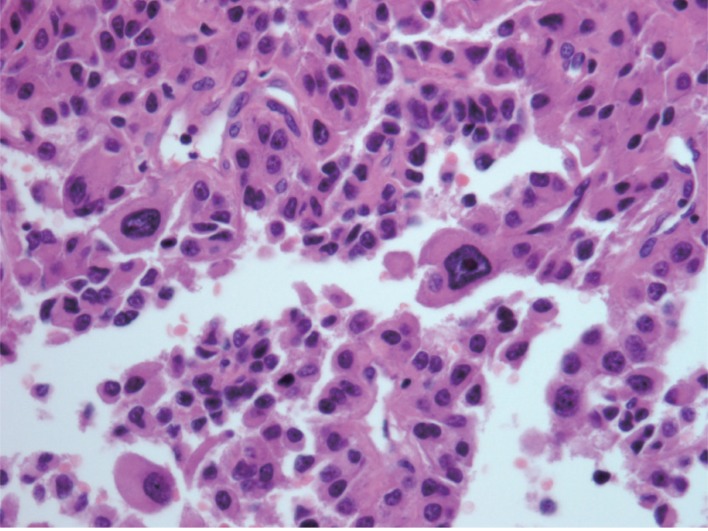
A 32-year-old woman was referred to our hospital for evaluation of a left adrenal mass. She had undergone an appendectomy 2 weeks earlier, and the mass was diagnosed incidentally on postoperative abdominal ultrasonography. On admission, her blood pressure was 110/70 mmHg, and her pulse was 80 beats/min. Serial blood pressures during her hospital stay ranged from 110/70 to 130/80 mmHg. The patient had hypokalemia (2.5 mmol/L) and was started on spironolactone (100 mg twice daily) and oral potassium chloride. The plasma aldosterone level was 389.53 pg/mL (normal range, 10.0 to 105) in the supine position and 716.87 pg/mL in the upright position (normal range, 34.0 to 273.0). Plasma rennin activity was 0.1 nmol/L/hr. Computed tomography showed a solid, homogenous adrenal mass with a maximum diameter of 42 mm (Fig. 1). An adrenalectomy with lymphadenectomy was performed. The tumor was an ill-defined, gray-tan solid mass measuring 42 × 33 × 22 mm (Fig. 2). Histopathologically, it consisted of a solid nest of bland to anaplastic cells with frequent mitoses and necrosis (Fig. 2). Her potassium level normalized on postoperative day 7 without potassium supplements or spironolactone.
DISCUSSION
In approximately 60% of cases, an adrenocortical carcinoma presents with evidence of adrenal steroid hormone excess [6], while APACs are exceedingly rare. To our knowledge, only 59 cases have been reported, including our case [3]. An apac is usually associated with hypokalemia, renal potassium leakage, and arterial hypertension due to excessive aldosterone secretion. A few specific symptoms such as muscle weakness and cramping, headache, palpitations, polydipsia, polyuria, and nocturia, or a combination of these symptoms, may be present in cases of marked hypokalemia [7]. Patients with suspected primary aldosteronism can be screened by measuring the morning ambulatory paired random plasma aldosterone concentration and plasma renin activity [2]. However, several studies have shown that most patients with primary aldosteronism have baseline blood potassium levels in the normal range [8,9]. Consequently, hypokalemia is not used to establish the diagnosis of primary aldosteronism, and an increased ratio of plasma aldosterone concentration to plasma renin activity is not diagnostic in itself [2]. Primary aldosteronism can be confirmed by an oral sodium loading test, an intravenous saline infusion test, or a fludrocortisone suppression test [2].
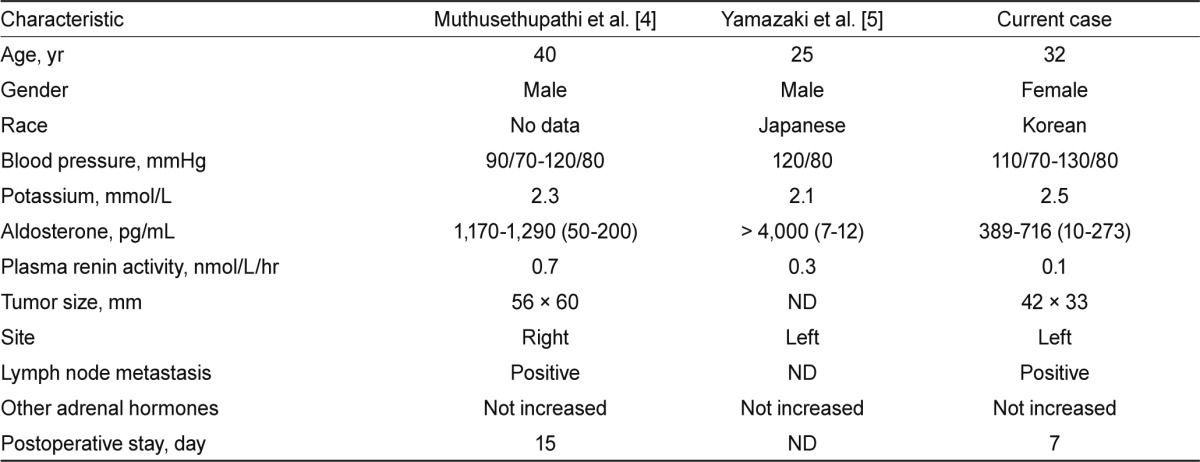
An APAC is a rare cause of primary aldosteronism. Typically, a patient with an APAC has features of primary aldosteronism, including hypertension and hypokalemia. Nevertheless, two of the 58 reported APAC patients had normal blood pressure [3]. The two cases of APAC without hypertension were reported by Muthusethupathi et al. [4] and Yamazaki et al. [5] Information on these two published cases and our case is summarized in Table 1.
Vantyghem et al. [7] presented two cases of apa without hypertension; including these two cases, 18 cases of normotensive primary hyperaldosteronism have been reported. Only 10 of these cases have been published in the English literature, and about 75% of cases have been reported in Eurasians. Of the three cases listed in Table 1, one patient was Japanese, and another patient was Korean; no information was available regarding the third.
The normal blood pressure in these rare cases of primary aldosteronism is not fully understood, and various explanations have been offered, including an absence of volume expansion, a low-salt diet, abnormal atrial natriuretic peptide activity, and the use of glucocorticoids [7]. The patients might have been hypotensive before the onset of the disease, might have experienced a blunted response to pressor agents, or might have exhibited associated hypopituitarism [4]. The exact cause of this disease in our patient remains unknown.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





