 |
 |
| Korean J Intern Med > Volume 27(2); 2012 > Article |
|
Abstract
Extrahepatic cholangiocarcinoma is often clinically challenging to diagnose. Even multidisciplinary approaches which include computed tomography, magnetic resonance imaging, and endoscopic retrograde cholangiography are unsatisfactory in some cases, especially with biliary stricture. Percutaneous transhepatic cholangioscopy (PTCS) with its direct visualization for biopsy appears to be a promising technique for detecting cholangiocarcinoma at an early stage. We report a case of adenocarcinoma in situ of the distal common bile duct (CBD) that was confirmed by PTCS. This case suggests the useful role of PTCS in the differential diagnosis of a distal CBD obstruction, particularly when other diagnostic modalities do not provide definitive information.
Cholangiocarcinoma accounts for almost 3% of all gastrointestinal cancers [1], and about one-fourth of cases with cholangiocarcinoma are distal extrahepatic cholangiocarcinomas [2]. Patients with cholangiocarcinoma typically present at advanced stages, and the cure rate is low, even with aggressive therapy [3]. The diagnosis of cholangiocarcinoma requires a multidisciplinary approach, which consists of high clinical suspicion in combination with appropriate imaging studies such as computed tomography (CT), magnetic resonance imaging (MRI) with cholangiopancreatography, percutaneous transhepatic cholangiography, and endoscopic retrograde cholangiopancreatography (ERCP) [3]. Percutaneous transhepatic cholangioscopy (PTCS) or peroral cholangioscopy appears to be a promising technique for detecting cholangiocarcinoma at an early stage [2]. We report the case of a patient with an adenocarcinoma in situ of the distal common bile duct (CBD) that was confirmed by PTCS.
A 55-year-old man was referred to our hospital for the evaluation of the obstruction of the distal CBD.
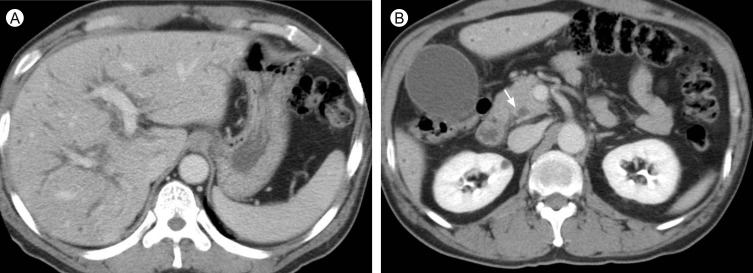
He had visited to a local hospital due to right upper quadrant pain, jaundice, and clay-colored stools for 1 week. An abdominal CT revealed a distended gallbladder with dilated intrahepatic and extrahepatic bile ducts (Fig. 1). The laboratory data were consistent with obstructive jaundice. Percutaneous transhepatic biliary drainage (PTBD) was performed, and the right upper quadrant pain was relieved. ERCP revealed a filling defect at the distal CBD with bile sludge. No stone was found. The patient was referred to our hospital for further evaluation and treatment.
No medical history of hypertension, diabetes mellitus, tuberculosis, or chronic liver disease was identified, and he denied smoking and alcohol intake. On admission, the vital signs were within normal ranges. No jaundice was observed in his conjunctiva. There was no palpable mass or tenderness in the abdomen. Laboratory test results included the following: white blood cell count, 6,790/┬ĄL; hemoglobin level, 13.8 g/dL; platelet count, 330 k/┬ĄL; serum creatinine, 1.1 mg/dL; blood urea nitrogen, 11 mg/dL; serum total bilirubin, 1.0 mg/dL; alkaline phosphatase, 112 IU/L; aspartate aminotransferase, 44 IU/L; alanine aminotranferase, 89 IU/L; serum amylase, 56 U/L; and C-reactive protein, 1.43 mg/dL. The serum hepatitis B surface antigen and serum hepatitis C antibodies were negative, and the serum levels of carcinoembryonic antigen and carbohydrate antigen 19-9 were 1.0 ng/mL and 22 U/mL, respectively.
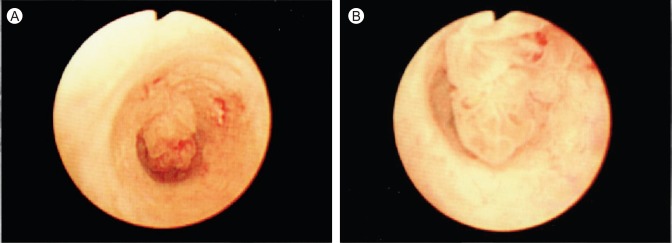
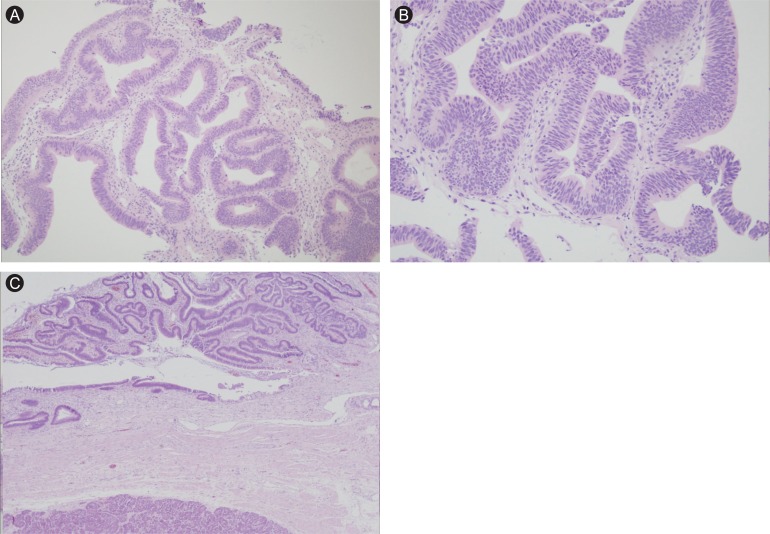
Abdominal CT revealed biliary decompression, but failed to demonstrate an obstructive lesion at the CBD, such as a stone or mass. A filling defect in the distal CBD was noted on a cholangiogram obtained through a PTBD tube (Fig. 2A); cellblock cytology of the bile drained through the tube was negative for malignant cells. The ERCP demonstrated a suspicious polypoid lesion at the distal CBD consistent with the previous cholangiogram; therefore, we performed a retrieval balloon sweep to evaluate whether a stone was in the CBD, and a biopsy was conducted (Fig. 2B). No stone was found in the CBD, but a microscopic examination of the duodenoscopic biopsy specimen showed high-grade epithelial dysplasia. PTCS was performed to determine a definitive diagnosis. A 1.0 ├Ś 1.0 cm polypoid lesion was visualized at the distal CBD on PTCS (Fig. 3). Adenocarcinoma in situ was confirmed after a pathology examination of the PTCS biopsy specimen.
With the diagnosis of adenocarcinoma in situ of the distal CBD, a laparoscopic pylorus-preserving pancreaticoduodenectomy was conducted. The resection margins of the bile duct and the pancreatic duct were confirmed negative for cancer cells by microscopic examination of frozen sections. A macroscopic examination of the resected specimen revealed a 1.8 ├Ś 1.5 cm elevated mass around the distal CBD adjacent to the ampulla of Vater. Microscopically, a papillary carcinoma that had developed in the bile duct was noted without features of lamina propria invasion and lymph node metastases (Fig. 4, pathologic TisN0 according to the TNM staging system). The patient remained healthy, with no evidence of recurrence 3 months after the resection.
According to cancer incidence data between 1999 and 2002 from the Korea Central Cancer Registry and International Agency for Research on Cancer, extrahepatic cholangiocarcinoma, including gallbladder cancer, is the seventh most common cancer in men and the eighth most common in women. The crude incidence rate per year is 6.8 and 6.9 cases per 100,000 Korean males and females, respectively [4]. The majority of cases occur in patients older than 65 years of age and the peak incidence is during the seventh decade of life [3].
In general, extrahepatic cholangiocarcinomas have a poor prognosis, with an overall five-year survival rate of 10-20% [1,3]. This is because most cases are locally advanced at presentation. In one large series, although a resection with negative margins was possible in 78% of cases, lymph node involvement was observed in 60% of the patients [5]. According to Korean report, resectability rate was 56%, and stage III or more disease is present in about 60% of the patients who undergo resection [6]. To improve the long-term survival of patients with extrahepatic cholangiocarcinoma, efforts should be directed toward early detection in patients presenting with obstructive jaundice.
The most common presenting symptoms of extrahepatic cholangiocarcinoma are jaundice (90%), pruritus (66%), abdominal pain (30-50%), weight loss (30-50%), and fever (up to 20%) [3]. Imaging studies for the diagnosis of extrahepatic cholangiocarcinoma include ultrasonography, CT, MRI, PTC, and ERCP. Preoperative tissue diagnosis is difficult because of the intense desmoplastic nature of the tumor [2,7]. Brush cytology and intraductal biopsies have a sensitivity < 50% [7]. Therefore, biliary endoscopy, with its direct visualization for biopsy, is often a good diagnostic tool for a definite diagnosis in patients who are suspicious for biliary tract cancer [8].
Since first introduced by Takada et al. in 1974 PTCS has been utilized to manage a variety of biliary tract disorders [9]. The introduction of small-caliber flexible cholangioscopes in 1976 by Yamakawa et al. further enhanced the application of this technique [9]. PTCS has been used to manage diverse biliary tract disorders, including intrahepatic calculi removal, dilatation of intrahepatic biliary strictures, and the evaluation of suspected bile duct cancers [9]. Several reports have suggested that PTCS can improve biopsy accuracy [8-10]. One large study reported that percutaneous cholangioscopic biopsy had a sensitivity of 82.4% for the diagnosis of cholangiocarcinoma [8]. Nimura [10] reported that a PTCS-directed biopsy had a sensitivity of 96% for diagnosing cholangiocarcinoma. These results are significantly better than those reported for fluoroscopically guided biopsies [9]. In the present case, the lesion was too small to be detected on abdominal CT. Although the ERCP revealed a suspicious filling defect in the distal CBD, the ERCP-directed biopsy failed to provide a precise diagnosis. PTCS visualized a polypoid lesion that was a high-grade dysplasia by ERCP-directed biopsy, and enabled more accurate biopsy and early diagnosis of a cholangiocarcinoma in situ.
In conclusion, extrahepatic cholangiocarcinoma is still clinically challenging to diagnose. When a cholangiocarcinoma is clinically suspected on abdominal CT or a cholangiogram but the results are not definitive, a PTCS and biopsy are a safe and effective approach for a more accurate and earlier diagnosis.
References
1. Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis 2004;24:115ŌĆō125PMID : 15192785.


2. de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med 1999;341:1368ŌĆō1378PMID : 10536130.


3. Anderson CD, Pinson CW, Berlin J, Chari RS. Diagnosis and treatment of cholangiocarcinoma. Oncologist 2004;9:43ŌĆō57PMID : 14755014.

4. Curado MP, Edwards B, Shin HR, et al. IARC Scientific Publications No. 160. Cancer incidence in five continents. 2007;Vol. IX:Lyon: IARC.
5. DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 2007;245:755ŌĆō762PMID : 17457168.



6. Joo YH, Myung SJ, Kim MH, et al. Clinical study on 193 cases of extrahepatic bile duct carcinomaand its prognostic factors. Korean J Gastroenterol 1999;33:114ŌĆō123.
7. Abu-Hamda EM, Baron TH. Endoscopic management of cholangiocarcinoma. Semin Liver Dis 2004;24:165ŌĆō175PMID : 15192789.


8. Ponchon T, Genin G, Mitchell R, et al. Methods, indications, and results of percutaneous choledochoscopy: a series of 161 procedures. Ann Surg 1996;223:26ŌĆō36PMID : 8554415.



Figure┬Ā1
Portal-phase computed tomography scans show the distended gallbladder with both intrahepatic bile duct and common bile duct dilatation (white arrow), which is suggestive of obstructive jaundice. However, there is no obstructive lesion such as an abnormal enhancing lesion or eccentric wall thickening at the distal common bile duct.
Figure┬Ā2
(A) Percutaneous transhepatic cholangiogram, and (B) endoscopic retrograde cholangiopancreatogram show a suspicious small contrast filling defect at the distal common bile duct (white arrow), but no definite obstructive lesion in the common bile duct.

Figure┬Ā3
On percutaneous transhepatic cholangioscopy, a 1 ├Ś 1 cm polypoid lesion was visualized in the distal common bile duct.
Figure┬Ā4
(A) The biopsy specimen obtained by percutaneous transhepatic cholangioscopy consisted of three tiny pieces of neoplastic biliary mucosa characterized by complex glandular structures lined by stratified neoplastic columnar epithelium (H&E, ├Ś 100). (B) High-power magnification demonstrates the loss of polarity of the surface lining, the nuclei occupying the entire thickness of the epithelium, and the architectural complexity shown by the back-to-back arrangement of the glandular structures (H&E, ├Ś 200). (C) A low power view of the laparoscopic pylorus preserving pancreaticoduodenectomy specimen demonstrates the elevated mass in the common bile duct, without definite features of lamina propria invasion (H&E, ├Ś 100).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



