 |
 |
| Korean J Intern Med > Volume 25(3); 2010 > Article |
|
Abstract
Background/Aims
Endoscopic papillary balloon dilation (EPBD) is a safe and effective method for the treatment of choledocholithiasis, but previous studies have rarely reported the appropriate ballooning time (BT). We prospectively evaluated the safety and efficacy of EPBD according to BT in patients undergoing bile duct stone removal.
Methods
Seventy consecutive patients with bile duct stones were randomly assigned to receive EPBD with either conventional (n = 35, 60 seconds) or short (n = 35, 20 seconds) BT.
Results
EPBD alone achieved complete bile duct clearance in 67 patients (long BT, n = 33, 94.3%; short BT, n = 34, 97.1%; p = 0.808). We also found no significant difference in the rate of complete duct clearance, including procedures that used mechanical lithotripsy, between the long and short BT groups (97.1% vs. 100%; p = 0.811). Mild pancreatitis was noted in four (11.4%) patients in the long BT group and two (5.7%) patients in the short BT group, but this incidence was not significantly different.
Endoscopic papillary balloon dilatation (EPBD) has been suggested as an alternative to endoscopic sphincterotomy (EST) for the treatment of choledocholithiasis [1,2], despite its possible association with an unacceptably high risk of pancreatitis [3]. Because this technique dilates the biliary sphincter without requiring surgical incision, acute complications such as hemorrhage and perforation are less likely [2,4,5] and biliary sphincter function is preserved [6-8]. Despite the frequent use of EPBD, studies have rarely reported the appropriate ballooning time (BT). A single recent EPBD study demonstrated a decreased tendency for post-procedural pancreatitis with a short BT (vs. long BT), with no differences in the efficacy of bile duct stone extraction [9]. Because patients experience pain during an EPBD despite adequate pre-procedural medication, the reduction in BT is desirable if the outcome is not affected. We therefore evaluated the safety and efficacy of EPBD performed with short and long BTs.
From September 2005 to July 2007, 70 consecutive patients who had been diagnosed with common bile duct (CBD) stones were randomly allocated to a long or short BT group. Patients were excluded if they had a history of previous EST or EPBD, choledochoduodenal fistula, benign bile duct stricture, previous precut papillotomy, or concomitant pancreatic or biliary malignancies. This study was approved by the institutional review board of our institution, and all patients provided written informed consent before enrolling in the study.
The initial diagnostic endoscopic retrograde cholangiopancreatography (ERCP) provided measurements of the CBD diameter, number of stones, and maximal transverse diameter of the largest stone. The technical success of the EPBD procedure was defined as the complete removal of all CBD stones, with or without the use of mechanical lithotripsy. Physical examination, abdominal radiography, and measurement of serum amylase and lipase, total bilirubin, alkaline phosphatase, and complete blood counts were performed the morning after the ERCP to detect early complications such as acute pancreatitis, acute cholangitis, perforation, or bleeding. Major complications associated with the ERCP were diagnosed and their severity was graded according to modified Cotton's criteria [10]. Bleeding that was controlled during the procedure without clinical evidence was not considered a complication. Post-procedural pancreatitis was defined as epigastric pain persisting for at least 24 hours with a serum amylase level exceeding three times the normal level. The pancreatitis was considered mild if hospitalization was extended for 2 to 3 days, moderate if hospitalization lasted 4 to 10 days, and severe when hospitalization time was prolonged for more than 10 days. Post-procedural hyperamylasemia was defined as a serum amylase concentration that exceeded three times the upper limit of normal levels.
The ERCP was performed with a side-viewing duodenoscope (TJF-240, Olympus Optical Corp. Ltd., Tokyo, Japan) under sedation with 3 to 5 mg midazolam and 25 mg meperidine hydrochloride. Duodenal peristalsis was suppressed with 20 mg scopolamine butylbromide. After selective cannulation of the CBD with a 0.035-inch cholangiography catheter (ERCP-Katheter, MTW® Endoskopie, Wesel, Germany), an initial cholangiogram was performed and the maximal transverse diameter of the CBD and the largest stone was measured. The measurements were corrected for magnification effects using the external diameter of the distal end of the duodenoscope as a reference. The catheter was then removed while the guide wire was left in place, and a balloon-tipped catheter (CRE balloon®, Boston Scientific Corp., Natick, MA, USA) was passed over the guide wire and placed across the papilla. Under endoscopic and fluoroscopic control, the balloon was gradually inflated with diluted radiopaque contrast medium to the target diameter using an inflation device (Indeflator®, Abbott, Santa Clara, CA, USA). The target diameter was based on the CBD and stone diameters.
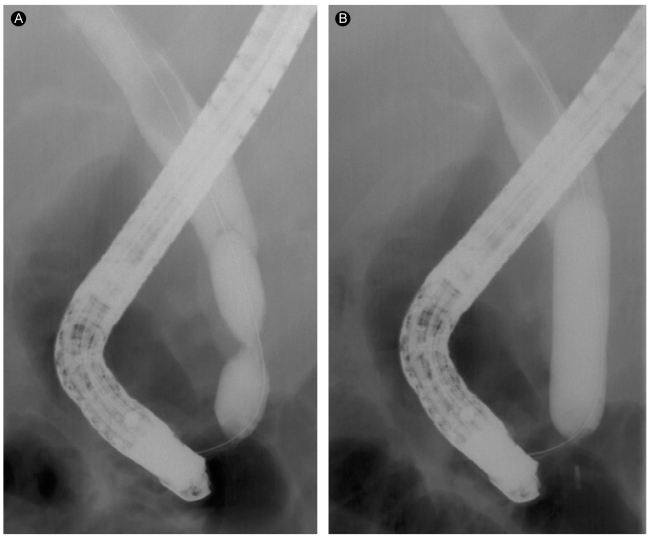
We defined BT as the period between attainment of the target diameter (Fig. 1) and deflation of the balloon. Short BT in this study was 20 seconds in duration, and long BT was 60 seconds. After dilation of the papilla, the balloon was deflated and the balloon catheter and guide wire were removed. CBD stones were removed with Dormia baskets (Web® extraction basket, Wilson-Cook Medical Inc., Winston-Salem, NC, USA) and/or retrieval balloon catheters (two-lumen retrieval balloon catheter, Boston Scientific Corp.). Mechanical lithotripsy was performed when the stone extraction could not be achieved with EPBD alone. A balloon-occlusion cholangiogram was obtained at the end of the procedure to ensure complete stone removal.
All continuous variables are expressed as means ┬▒ standard deviation (SD). Student's t test was used to compare mean values between the two groups. Categorical and binary variables were analyzed using chi-square tests. A p value of less than 0.05 was considered statistically significant. All analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
The conventional, long BT group included 35 patients (19 men, 16 women; mean age, 66.2 ┬▒ 17.4 years), as did the short BT group (16 men, 19 women; mean age, 63.3 ┬▒ 13.6 years). No significant differences were found in bile duct diameter, stone number or size, or previous cholecystectomy between groups (Table 1). The EPBDs of three patients (8.5%) in each group used a large (> 15 mm diameter) balloon catheter.
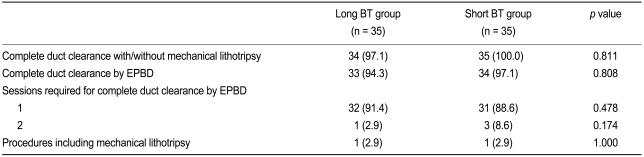
EPBD achieved complete duct clearance in 33 patients (94.3%) in the long BT group and 34 patients (97.1%) in the short BT group; this difference was not significant (p = 0.808). All CBD stones were completely retrieved during the initial EPBD in 32 patients (91.4%) in the long BT group and 31 patients (88.6%) in the short BT group (p = 0.478). Complete stone removal was achieved during the second EPBD in one patient (2.9%) in the long BT group and two patients (5.7%) in the short BT group (p = 0.174). The mean numbers of sessions required for complete duct clearance were 1.2 and 1.1, respectively, for the long and short BT groups. No significant difference was observed in the rate of complete bile duct clearance between groups, independent of the use of mechanical lithotripsy (long BT, 97.1% vs. short BT, 100%; p = 0.811). One patient (2.9%) in each group required mechanical lithotripsy (Table 2); in these cases, the dilated biliary outlet was unexpectedly smaller than the largest stone after EPBD, preventing extraction. The stone of one patient in the long BT group could not be extracted because it was impacted in the CBD lumen, and the basket could not open properly. This stone was extracted using peroral transpapillary cholangioscopy with electrohydraulic lithotripsy.
Pancreatitis was noted in four patients (11.4%) in the long BT group and two patients (5.7%) in the short BT group (p = 0.393). All post-ERCP pancreatitis observed in this study was mild and resolved without complications. Asymptomatic hyperamylasemia was present in four patients (11.4%) in the long BT group and three patients (8.6%) in the short BT group (p = 0.690). No other complications, such as hemorrhage, perforation, or cholangitis, occurred in either group. Serum amylase levels measured the morning after ERCP were 346.8 ┬▒ 55.6 IU/L in the long BT group and 198.2 ┬▒ 39.5 IU/L in the short BT group; this difference was significant (p = 0.037) (Table 3).
EPBD is technically easy and can be readily performed by endoscopists trained in standard therapeutic ERCP techniques [11]. Concerns regarding the increased incidence of ascending cholangitis and the possible recurrence of bile duct stones after EST [12,13], especially in younger patients, have led to the revival of EPBD. However, no agreement has been reached on the appropriate BT, which has been determined primarily by the operator's experience with the procedure. Balloon dilation has been used on the strictures of the esophagus, pylorus, and colon. BT must be sufficient for the dilation of the stricture and the reduction of restenosis risk. However, the papilla is a physiologically narrow area and should lack fibrosis unless a benign or malignant biliary stricture is also present. Reduction in BT may therefore help to preserve the physiological function of the papilla after EPBD, and may also reduce the risk of post-ERCP pancreatitis by curtailing the obstruction time of the pancreatic duct orifice. The sphincter is thought to be adequately dilated when the waist of the balloon disappears completely. In our experience, the waist disappeared within 20 seconds of achieving the target diameter in most EPBD procedures. We therefore found it reasonable to determine the effective minimum BT as the time required for the waist to disappear (20 seconds), and further believed that this minimum BT would be sufficient to dilate the papilla.
Patients may experience abdominal pain during EPBD, and the procedure has been associated with an increased risk of pancreatitis. Longer BTs further exacerbate these disadvantages [14]; BT reduction may conversely help alleviate these problems. Previous studies have reported BTs ranging from 30 to 120 seconds, with most operators using a 60-second BT [11,15-20]. The present study found comparable outcomes in the short and long BT groups, measured by the overall technical success of stone removal. Our results suggest that BT may be reduced when EPBD is performed.
This study found lower rates of post-procedural pancreatitis and hyperamylasemia in the short BT group than in the long BT group, but these differences were not significant. Post-procedural serum amylase levels were significantly lower in the short BT group than in the long BT group. The compression of the papilla or the pancreatic duct orifice by ballooning may cause papillary edema or a sphincter of Oddi spasm during the EPBD procedure, which obstructs the flow of pancreatic juice and eventually results in a pancreatic insult [21-23]. Many factors may act independently or in concert to cause post-ERCP pancreatitis [24-26]; high-risk predictors include suspected sphincter of Oddi dysfunction (SOD), young age, history of post-ERCP pancreatitis, number of contrast injections into the pancreatic duct, and experience of the endoscopist. This study did not assess risk factors for post-ERCP pancreatitis, but our data suggest that a shorter BT may reduce the frequency of pancreatic insults during an EPBD, thus leading to a lower incidence of pancreatitis. A review of eight EPBD studies in which BT was specified (Table 4) found that BT ranged from 30 to 120 seconds, based on the operator's personal experience, and that a single EPBD was performed in most cases [11,15-20]. Two or three EPBDs were performed in two studies [17,20]. A comparison of efficacy and early complications according to BT showed no significant differences in the results of previous studies. Several confounding variables, however, prevented us from ruling out the possibility of correlations. These variables included the endoscopist's experience and the number of pancreatic duct cannulations.
Tsujino et al. [27] reported immediate and long-term complications associated with EPBD in 1000 patients; they initially inflated the balloon with air or diluted contrast material for 2 minutes, but reduced BT after one patient developed severe post-procedural pancreatitis. In the modified procedure, the balloon was inflated slowly for 1 to 2 minutes with diluted contrast, until the waist disappeared. The pressure was maintained for 15 seconds and they achieved complete removal of CBD stones with EPBD. The results of this study suggested that a short BT was sufficient for the removal of CBD stones, and that the ballooning speed may have been an important factor associated with complications; a slowly inflated balloon appeared to be less harmful to the ampulla of Vater, as it decreased post-procedural complications.
In conclusion, this study found that EPBD with a short, 20-second BT was safe and effective. The outcomes of procedures using a short BT were comparable to those using a conventional, 60-second BT for the treatment of bile duct stones. In addition, a short BT tended to be associated with a decreased incidence of post-ERCP pancreatitis and hyperamylasemia. Large prospective population studies are required to confirm the safety and efficacy of EPBD with a short BT, and to empirically define the appropriate BT for EPBD.
Acknowledgments
This study was supported by an Inha University Research Grant. All authors state that they have no conflicts of interest.
References
1. Fujita N, Maguchi H, Komatsu Y, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: a prospective randomized controlled multicenter trial. Gastrointest Endosc 2003;57:151ŌĆō155PMID : 12556774.


2. Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol 2004;99:1455ŌĆō1460PMID : 15307859.


3. Disario JA, Freeman ML, Bjorkman DJ, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology 2004;127:1291ŌĆō1299PMID : 15520997.


4. Park DH, Kim MH, Lee SK, et al. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc 2004;60:180ŌĆō185PMID : 15278041.


5. Toda N, Saito K, Wada R, et al. Endoscopic sphincterotomy and papillary balloon dilation for bile duct stones. Hepatogastroenterology 2005;52:700ŌĆō704PMID : 15966186.

6. Sato H, Kodama T, Takaaki J, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut 1997;41:541ŌĆō544PMID : 9391256.



7. Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut 2001;49:686ŌĆō691PMID : 11600473.



8. Isayama H, Komatsu Y, Inoue Y, et al. Preserved function of the Oddi sphincter after endoscopic papillary balloon dilation. Hepatogastroenterology 2003;50:1787ŌĆō1791PMID : 14696405.

9. Tsujino T, Kawabe T, Isayama H, et al. Efficacy and safety of low-pressured and short-time dilation in endoscopic papillary balloon dilation for bile duct stone removal. J Gastroenterol Hepatol 2008;23:867ŌĆō871PMID : 18086110.


10. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383ŌĆō393PMID : 2070995.


11. Natsui M, Narisawa R, Motoyama H, et al. What is an appropriate indication for endoscopic papillary balloon dilation? Eur J Gastroenterol Hepatol 2002;14:635ŌĆō640PMID : 12072597.


12. Sugiyama M, Atomi Y. Follow-up of more than 10 years after endoscopic sphincterotomy for choledocholithiasis in young patients. Br J Surg 1998;85:917ŌĆō921PMID : 9692563.


13. Wojtun S, Gil J, Gietka W, Gil M. Endoscopic sphincterotomy for choledocholithiasis: a prospective single-center study on the short-term and long-term treatment results in 483 patients. Endoscopy 1997;29:258ŌĆō265PMID : 9255528.


14. Nakagawa H, Ohara K. Safeguards against acute pancreatitis associated with endoscopic papillary balloon dilatation. J Hepatobiliary Pancreat Surg 2006;13:75ŌĆō79PMID : 16547665.


15. Seo DW. Prospective analysis of endoscopic papillary balloon dilatation and endoscopic sphincterotomy for removal of common bile duct stones. Gastrointest Endosc 2000;52:140ŌĆō142PMID : 11012300.


16. Vlavianos P, Chopra K, Mandalia S, Anderson M, Thompson J, Westaby D. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut 2003;52:1165ŌĆō1169PMID : 12865276.



17. Ochi Y, Mukawa K, Kiyosawa K, Akamatsu T. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. J Gastroenterol Hepatol 1999;14:90ŌĆō96PMID : 10029284.


18. Watanabe H, Yoneda M, Tominaga K, et al. Comparison between endoscopic papillary balloon dilatation and endoscopic sphincterotomy for the treatment of common bile duct stones. J Gastroenterol 2007;42:56ŌĆō62PMID : 17322994.


19. Bergman JJ, Rauws EA, Fockens P, et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet 1997;349:1124ŌĆō1129PMID : 9113010.


20. Mac Mathuna P, White P, Clarke E, Lennon J, Crowe J. Endoscopic sphincteroplasty: a novel and safe alternative to papillotomy in the management of bile duct stones. Gut 1994;35:127ŌĆō129PMID : 8307433.



21. Tulassay Z, Papp J, Koranyi L, Szathmari M, Tamas G Jr. Hormonal and biochemical changes following endoscopic retrograde cholangio-pancreatography. Acta Gastroenterol Belg 1981;44:538ŌĆō544PMID : 6180583.

22. Ueno N, Ozawa Y. Pancreatitis induced by endoscopic balloon sphincter dilation and changes in serum amylase levels after the procedure. Gastrointest Endosc 1999;49(4 Pt 1):472ŌĆō476PMID : 10202061.


23. Pezzilli R, Romboli E, Campana D, Corinaldesi R. Mechanisms involved in the onset of post-ERCP pancreatitis. JOP 2002;3:162ŌĆō168PMID : 12432182.

24. Sugiyama M, Izumisato Y, Abe N, Masaki T, Mori T, Atomi Y. Predictive factors for acute pancreatitis and hyperamylasemia after endoscopic papillary balloon dilation. Gastrointest Endosc 2003;57:531ŌĆō535PMID : 12665764.


25. Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol 2006;101:139ŌĆō147PMID : 16405547.


Figure┬Ā1
Cholangiogram showing endoscopic papillary balloon dilation. (A) The biliary sphincter is visible as a 'waist' during balloon inflation. (B) The biliary sphincter is adequately dilated when the balloon's waist has completely disappeared.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



