INTRODUCTION
Aspergillus is a ubiquitous fungus that causes a variety of clinical syndromes in the lung. The type and severity of airway and parenchymal disease produced by Aspergillus are influenced by the patient's immunologic status and the presence of pre-existing lung disease. In recent years, it has been demonstrated that Aspergillus infections can result in a broad range of airway complications1). Acute pseudomembranous tracheobronchitis is an uncommon form of invasive apergillosis that is usually limited to the large airways and is a newly reported clinical entity2). It has been reported in severely immunocompromised states, such as postallogenic bone-marrow transplantation, malignancy, and AIDS patients, or in immunodeficient patients associated with T cell dysfunction by influenza A infection3). This report is about a case of pseudomembranous necrotizing tracheobronchial aspergillosis that developed in an immunocompetent host.
CASE REPORT
A 44-year-old Korean male presented with a fever, non-productive cough, and myalgias for 10 days. For the previous 5 years, he had been treated for hypertension with an angiotensin-converting enzyme inhibitor. Prior to admission, he was treated with oral quinolone for 7 days by the outpatient department, but his condition progressively worsened with resting dyspnea, a productive cough, and a fever for 2 days before admission to the Wonkwang University Hospital, Iksan, Korea. The patient was a 30-pack-a-year ex-smoker, and had no history of previous respiratory diseases nor a specific family history.
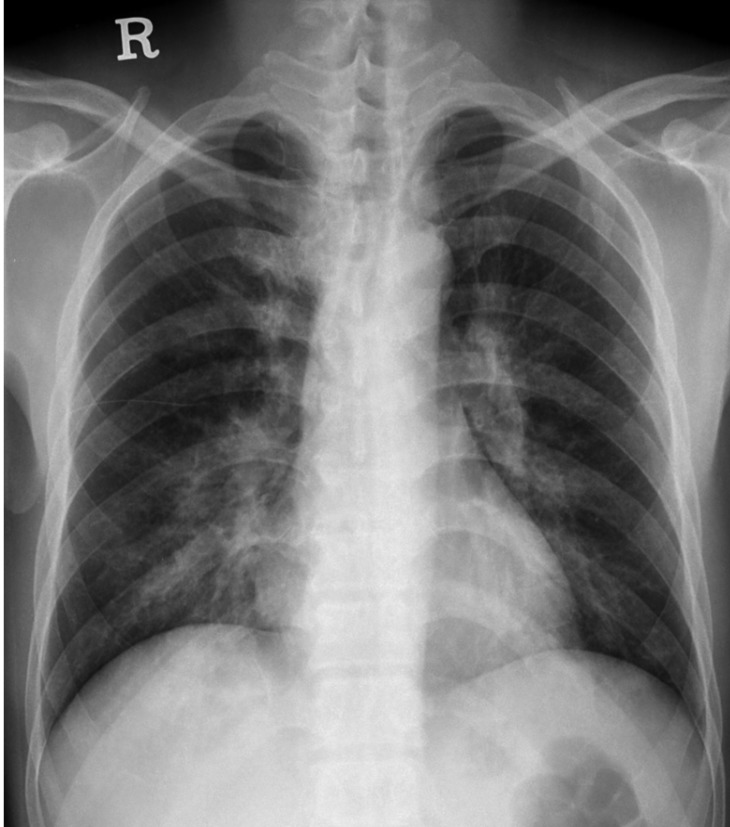
On admission, he had a temperature of 38.6Ōäā, blood pressure of 120/80 mmHg, heart rate of 90 b.p.m, and respiratory rate of 30 breaths/min. Chest auscultation was significant for bilateral inspiratory coarse, crackles and end-expiratory wheezing around the perihilar areas. Arterial blood gas values on room air were: pH 7.343, PaCO2 41.2 mmHg, PaO2 59.2 mmHg, and SaO2 90.7%. The WBC was 19,580/mm3 (neutrophils 82.5%); the ESR was 71 mm/h; and the C-reactive protein was 184.6 mg/L. The percentage of hemoglobin A1c in the blood was 5.8%. The blood urea nitrogen was 32.4 mg/dL and the creatinine was 1.32 mg/dL. The random glucose of capillary blood on admission was 117 mg/dL. A chest X-ray obtained on admission demonstrated bilateral bronchial wall thickening with perihilar area and lower lobe predominance (Figure 1). The results of the initial sputum stains and sputum and blood cultures were all negative. The HIV test also was negative.
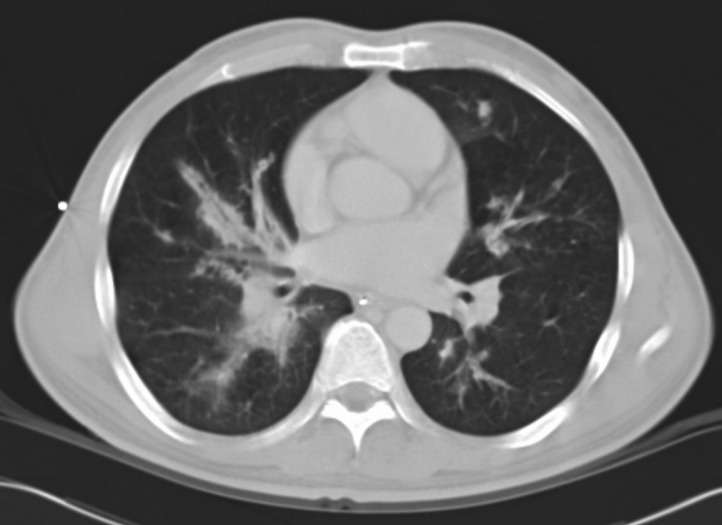
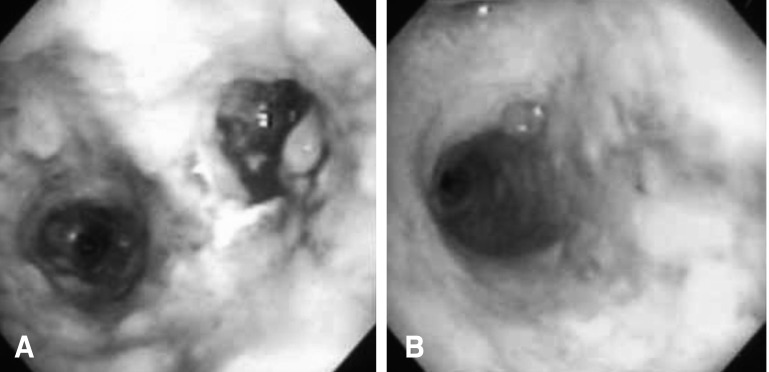
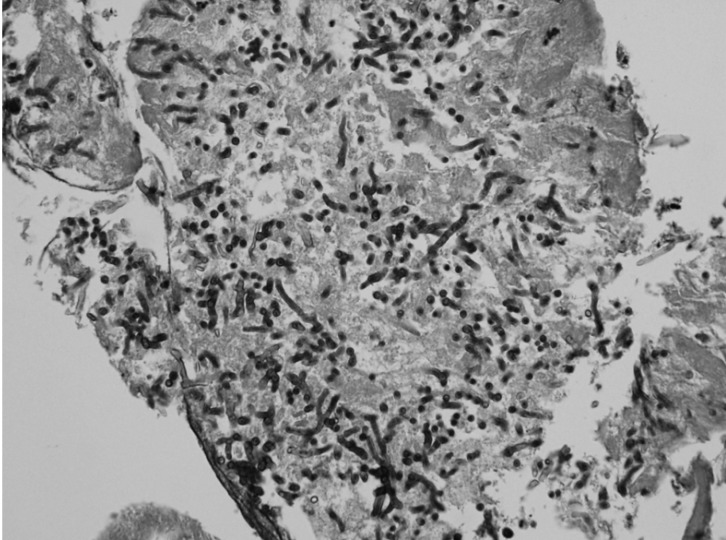
The patient received empirical therapy with cefoperazone/sulbactam and vancomycin for 4 days, but rapidly deteriorated with a high fever, increasing dyspnea, and hypoxemia. He developed respiratory failure with severe CO2 retention, and was admitted to the intensive care unit and mechanically ventilated. On the fifth day of therapy, chest CT and fiberoptic bronchoscopy were performed because of a rapidly increasing respiratory acidosis with hypoxemia in contrast to the chest X-ray lesions. A chest CT scan revealed only bilateral peribronchial infiltrates with patent bronchi and no consolidation of the parenchyma (Figure 2). A bronchoscopy demonstrated extensive whitish exudative membranes covering the trachea and both mainstem bronchi (Figure 3). The endobronchial biopsy specimens and bronchial washing fluid revealed Aspergillus species without parenchymal invasion (Figure 4). A high fever persisted and 2 days later the patient developed refractory septic shock and hypoxemia. Despite using IV amphotericin B and supportive care, acute deterioration followed with refractory hypoxemia and oliguria, resulting in a fatal cardiac arrest on the fifth day of the intensive care unit stay. We could not perform a post-mortem examination because of the refusal of his family members.
DISCUSSION
Invasive pulmonary aspergillosis (IPA) occurs usually following inhalation of Aspergillus in the immunocompromised host3). The rate of invasive mycoses has been on the rise recently, and especially invasive aspergillosis among all mycoses increased from 14% to 60% over a 14-year period, probably as a result of greater life expectancies and an increase in the number of immunocompromised patients4). Rarely, IPA has been reported in apparently immunocompetent or in mildly immunocompromised patients, such as those with alcoholism, chronic liver disease, and diabetic ketoacidosis3, 4). Because the diagnosis is often delayed for such patients, the mortality rate has been reported at 100%3). Therefore, invasive pulmonary aspergillosis must be considered in immunocompetent patients with pulmonary infiltrates who do not respond to broad-spectrum antibiotics.
Acute airway invasive aspergillosis accounts for less than one-third of all cases of invasive aspergillosis5). Pseudomembranous necrotizing tracheobronchial aspergillosis has been reported recently as an uncommon form of airway invasive aspergillosis in immunocompromised patients2, 6-8). In a review of the literature on Aspergillus tracheobronchitis, including all forms of tracheobronchial involvement, reports indicated that the disease was progressive and fatal in about 40% of cases. It is apparently a lethal variant of tracheobronchial aspergillosis with a markedly higher mortality rate and more parenchymal lung involvement (65%) compared with all cases with Aspergillus tracheobronchitis (45%)9). It presents with an extensive transmural necrotizing bronchitis with pseudomembrane formation that develops in immunocompromised patients, and it is usually characterized by a limited extension of inflammation and hyphae into the peribronchial tissue, without an invasion of the pulmonary parenchyma2). The pseudomembrane is the whitish membrane or large plugs that occlude the lumen due to the accumulation of hyphae, exudates, and necrotic material. Although those are distinct pulmonary entities from Aspergillus pneumonia, occasionally, involvement of the bronchial tree can be invasive, leading to a pseudomembranous tracheobronchitis that is associated with extensive bronchial hemorrhage and an invasion of the bronchial walls and vessels.
Generally, host immune status determines the manifestations of Aspergillus lung disease and the response to treatment. Patients with Aspergillus tracheobronchitismay be less neutropenic and require less exposure to corticosteroids and cytotoxic drugs than patients with parenchymal involvement. In the literature review, 22 cases with this variant of tracheobronchial involvement by Aspergillus have been described. To date, there have been only five reports of this disease developing in a immunocompetent or mildly immunocompromised patient. But the first case revealed cutaneous anergy and lymphopenia involving T cells and NK cells, related to a recent influenza A infection10). In the second case, there were "Grayish" mucus plugs in several segmental bronchi on autopsy and focally limited extension into the adjacent lung parenchyma8). The third case revealed the presence of a fungal invasion through the bronchial wall into the adjacent lung parenchyma and pulmonary arteries8). The fourth case was a 70-year-old man with risk factors, including corticosteroid use. The last case was a 66-year-old woman whose underlying disease was chronic airway limitation. The present patient had no risk factors associated with an immunocompromised state, and without invasion of the parenchyma, or atelectasis, but who progressed rapidly to severe CO2 retention and respiratory failure. To the best of our knowledge, this is a report of a rare case of Aspergillus pseudomembranous tracheobronchitis without an invasion of the pulmonary parenchyma that developed in an immunocompetent patient. In this regard, Aspergillus tracheobronchitis was confined, at least initially, to the airways with only a superficial mucosal invasion, and the diagnosis is usually delayed because of non-specific signs and symptoms and lack of radiographic abnormalities9).
A chest X-ray is not much help in the diagnosis for several reasons, usually because of normal radiological findings: intraluminal mycetomas may not be readily detectable, aspergillus may enlarge so rapidly that recent prior chest radiographs may not reveal atelectasis and the lung parenchyma is usually unaffected1). And radiologically, the only alteration may be the presence of patchy atelectasis related to the mucus plugs. A chest CT scan is a much more helpful tool in the early diagnosis and aids further diagnostic studies, such as bronchoscopies and open-lung biopsies. Occasionally, a chest CT scan reveals tracheal or bronchial wall thickening, including opacification of paratracheal fat, tracheal narrowing, and pneumomediastinum in Aspergillus tracheobronchitis2, 11). Although a CT scan is helpful in the diagnosis of airway aspergillosis, specific organism diagnosis cannot be made on the basis of imaging features alone.
Bronchoscopy, apart from providing specimens for microbiological examination, is a very useful method for detecting infections with endobronchial manifestations9). Bronchoscopic findings are characteristic, revealing focal or diffuse ulcerative or 'plaque-like' inflammatory lesions (pseudomembranes) along the tracheobronchial walls. It should be recommended as early as possible to both diagnose and maintain airway patency at a time when it is most feasible5, 12, 13). Aspergillus is seen deep to the basement membrane of the bronchioles at histology, and is usually seen within the airway lumen. A presumptive diagnosis is made when the fungus is isolated from bronchial aspirates or BAL cultures, and a definitive diagnosis is made when there is histologic demonstration of invasion of the mucosa by hyphae. Therefore, culture and histologic examinations of bronchoscopically identified trcheobronchial mucus plugs and necrotic material should be performed in all immunocompromised individuals, even when the main radiographic finding is atelectasis. Early detection of intraluminal growth of Aspergillus and prompt institution of antifungal therapy may facilitate the management of these patients.
In conclusion, as in our patient, the Aspergillus infection of the tracheobronchial tree probably contributed significantly to the development of terminal respiratory failure in an immunocompetent patients. Although its incidence is rare, pseudomembranous necrotizing tracheobronchial aspergillosis must be considered in immunocompetent patients with dyspnea progressing to severe hypoxemia without an invasion of the pulmonary parenchyma and without a response to broad spectrum antibiotics. Therefore, although early recognition of the infection may not have altered the course of the underlying disease in some of these patients, in others, identification and early treatment might have been life-saving.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





