INTRODUCTION
Adult onset Still's disease (AOSD) is a rare, clinical entity characterized by spiking fever, evanescent rash, arthralgia or arthritis, and neutrophilic granulocytosis with negative rheumatoid factor and antinuclear antibody test results1-4). The most common cardiac manifestations associated with AOSD are pericarditis and myocarditis1-3). Cardiac valve involvement in AOSD is extremely rare, with only four cases of noninfectious mitral endocarditis having been previously described5-7).
The present report describes the case of a 55-year-old woman with AOSD complicated by acute severe mitral and aortic insufficiency who underwent mitral valve replacement (MVR) and Bentall's operation.
CASE REPORT
In October 2003, a 55-year-old woman with chronic polyarthritis and myalgia was referred by the local tertiary hospital to our hospital. Four months prior, she developed general myalgia and polyarthralgia, mainly in the ankles and shoulders, and recorded body temperatures up to 39.8Ōäā. She was admitted to the local tertiary hospital and intravenous ampicillin/sulbactam was empirically administered. After 3 days, the body temperature of the patient normalized, while polyarthralgia and myalgia remained. Two weeks later, the patient's body temperature again rose to 39.4Ōäā, and an erythematous skin rash developed on both legs and the upper arms. She was empirically administered intravenous vancomycin and ciprofloxacin, and the body temperature normalized and the erythematous skin rash disappeared after 5 days. Polyarthralgia and myalgia persisted.
The patient underwent a series of blood tests which revealed the following: leukocytes 18,400/mL (4,000-10,000/mL, neutrophil 90.2%), hemoglobin 10.5 g/dL (12-16 g/dL), platelets 467,000/mL (150,000-350,000/mL), AST/ALT 110/111 IU/L (0-40 IU/L), ALP 730 IU/L (40-120 IU/L), GTP 473 IU/L (8-35 IU/L), LDH 567 U/L (120-250 U/L), ESR 64 mm/hr (0-20 mm/hr), CRP 23 mg/dL (0-0.6 mg/dL), and ferritin 998 ng/mL (10-290 ng/mL). Testing for rheumatoid factor (RF) and antinuclear antibodies (ANA) returned negative results. Repeated blood cultures returned negative results. Bone marrow examination showed marked granulocytic hyperplasia without evidence of hematologic malignancy, and no growth was observed on bacterial, fungal, or mycobacterial culture plates. Echocardiogram showed minimal mitral regurgitation without evidence of infectious endocarditis. Abdominopelvic computed tomography (CT) showed mild hepatomegaly with four hepatic hemangiomas. Skin biopsy showed diffuse neutrophilic infiltration in the entire dermis, consistent with Sweet's syndrome.
On the basis of the clinical and laboratory findings, the patient was administered 40 mg prednisolone per day, after which the symptoms of polyarthralgia and myalgia were relieved. The patient was discharged two weeks later (August 13, 2003) with a treatment regime of 15 mg prednisolone per day. Two weeks later, she revisited the local hospital outpatient clinic with signs that the polyarthralgia and myalgia had resurfaced, and that ESR and CRP were elevated. The prednisolone dose was increased to 60 mg per day and the symptoms were alleviated for 2 months. However, on October 30, 2003, the patient was transferred to our hospital and, due to complaints of polyarthralgia involving both first metatarsophalangeal joints, both ankles, both hips, both shoulders, and general myalgia, was admitted. Upon physical examination, tenderness and swelling were observed at both metatarsophalangeal joints, the left ankle, and the left sternoclavicular joint. Laboratory testing revealed that ESR, CRP, and ferritin levels were elevated (ESR 70 mm/hr, CRP 11 mg/dL, ferritin 1792 ng/mL).
According to her clinical history and local tertiary hospital laboratory data, the patient was diagnosed with AOSD using Yamaguchi's classification criteria4): fever lasting 1 week or longer, arthralgia lasting 2 weeks or longer, leukocytosis, liver dysfunction, and negative RF and ANA tests.
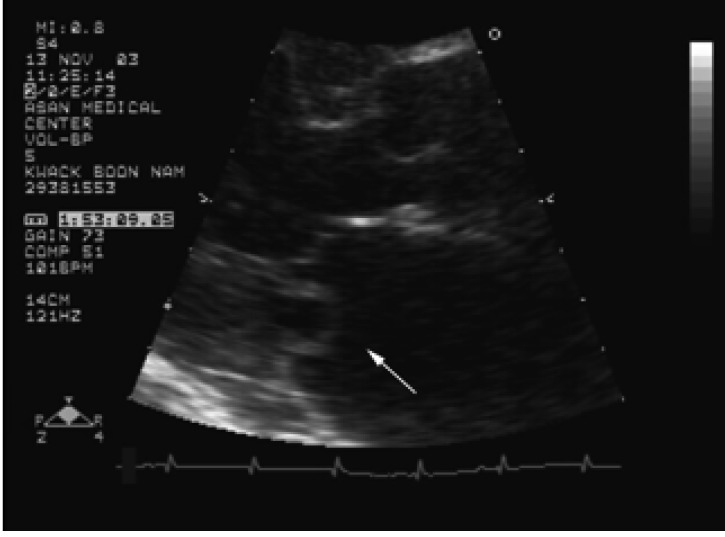
Following admission, we administered 30 mg prednisolone twice per day and 10 mg methotrexate per week. The polyarthralgia and myalgia were subsequently alleviated. On follow up laboratory tests, ESR, CRP, and ferritin levels had decreased (ESR 52 mm/hr, CRP 2.01 mg/dL, ferritin 789 ng/mL). The patient was discharged five days later. She was readmitted one week later for dyspnea and general edema. Systolic murmurs and diastolic murmurs at the apex were observed upon cardiac auscultation. Chest X-rays showed cardiomegaly and bilateral pulmonary edema. Transthoracic echocardiogram showed severe mitral regurgitation (MR) due to prolapse of the posterior mitral valve leaflet, and moderate to severe aortic regurgitation (AR) due to right coronary cusp prolapse. Transesophageal echocardiogram also showed severe MR and AR due to valve leaflet prolapse. The valve prolapse appearance was notable because the prolapsing posterior mitral valve was focally fixed in the left atrium during systolic and diastolic cycles (Figure 1). The patient underwent a mitral valve replacement (MVR) and Bentall's operation on November 22, 2003.
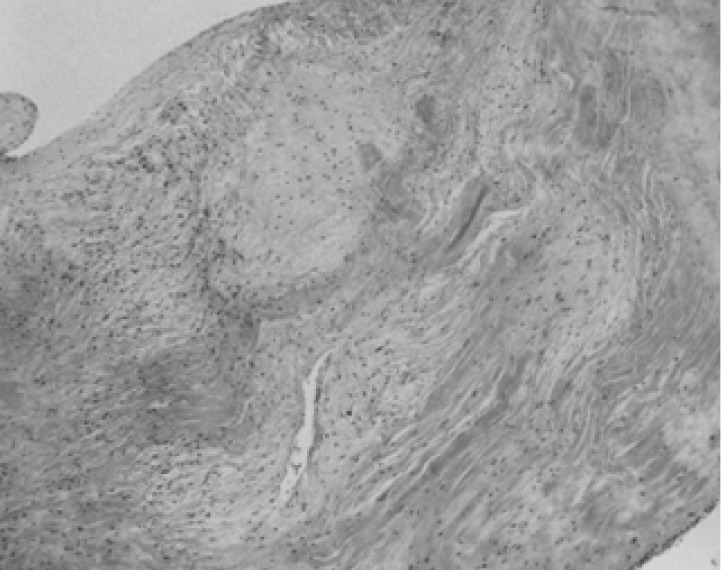
Histological examination of heart tissue showed fibromyxoid degeneration with chronic active inflammation in the aortic wall, and chronic active inflammation with fibrinoid necrosis of the aortic and mitral valves (Figure 2). Ziehl-Neelson, Periodic acid shiff, and Gram staining failed to identify any organisms. The presence of extensive fibrinoid necrosis, which is unusual in the case of ordinary valvulopathy, suggested valvulopathy associated with connective tissue disease. After MVR and Bentall's operation, the patient acquired normal mitral and aortic valvular function. She was, thereafter, administered oral medication through the outpatient clinic. Upon outpatient follow-up laboratory testing, ESR, CRP, and ferritin levels were 28 mg/hr, 1.30 mg/dL, and 720 ng/mL, respectively. The patient is currently taking 10 mg prednisolone per day and 17.5 mg methotrexate per week without relapse.
DISCUSSION
The diagnosis of AOSD is based exclusively on clinical findings because serological markers and other diagnostic tests do not exist1-4). Several sets of classification criteria have been published without statistical endorsement. The preliminary criteria for AOSD proposed by Yamaguchi et al.4) have a sensitivity of 96.2% and a specificity of 92.1%, and comprise five or more criteria, including two or more major criteria in the absence of other clinical explanations. The patient described in the present report fulfilled three major and two minor criteria: fever, arthritis, leukocytosis, liver dysfunction, and negative RF and ANA test results. The diagnosis of AOSD in this patient was also consistent with criteria which have recently been proposed by Fautrel et al.8) and do not require exclusion criteria. Since the late 1980s, several authors have suggested that an increased serum ferritin level (>5 times normal) may indicate AOSD9). In the present patient, the initial ferritin level was 760 ng/mL (10-290 ng/mL), and increased to 1792 ng/mL upon follow-up enzyme immunoassay. At greater than 5 times the normal level, this is consistent with AOSD.
The patient described in the present report developed an erythematous skin rash consistent with Sweet's syndrome, an acute febrile neutrophilic dermatosis characterized by painful red papules, nodules, or plaques. Elinav et al.10) reported the coexistence of Sweet's syndrome and AOSD, and cast doubt as to whether this association was as rare as initially assumed, because erroneous omission of one diagnosis may occur, especially when findings are not confirmed by tissue diagnosis. Histologically, AOSD patients have no specific inflammation of diagnostic significance3). Biopsies of skin rashes indicate only non-specific inflammatory reactions in the dermis, with mild or moderate perivascular infiltration by polymorphonuclear and/or mononuclear leukocytes1, 2). Histological analysis of mitral and aortic valve tissue of the present patient revealed chronic active inflammation with neutrophilic infiltration that was similar to previous skin histology. Additionally, the patient was found to possess extensive fibrinoid necrosis, which is unusual in ordinary valvulopathy, suggesting the involvement of an unusual systemic inflammatory disorder. To our knowledge, only two cases of non-infectious mitral endocarditis5) and two cases of aortic endocarditis have been described in patients with AOSD6, 7). Histological analysis of tissue from one of these patients revealed valvular fibrinoid necrosis with massive lymphohistiocytic infiltration5). Although the present patient had extensive fibrinoid necrosis with neutrophilic infiltration contrary to previously reported lympho-histiocytic infiltration, we assumed AOSD as a cause of severe MR and AR, since the histologic findings of AOSD were nonspecific and no other explainable clinical cause, such as subacute infective endocarditis, syphilis, etc., was found.
The mainstays of AOSD treatment have been aspirin, non-steroidal anti-inflammatory drugs (NSAID), and steroids. We initially administered 10 mg methotrexate per week, as the patient had relapsed despite taking prednisolone. It has been reported that methotrexate is useful for controlling AOSD disease activity in refractory patients11, 12). Nonetheless, the present patient still developed acute severe mitral and aortic regurgitation. Because she was hemodynamically unstable, we were compelled to perform mitral valve replacement (MVR) and Bentall's operation.
Although many connective tissue disorders are known to be associated with aortitis and valvulitis, it is unusual for cardiac valvular disease complicating chronic inflammatory disorders of connective tissue to be severe enough to require surgical intervention13).
Townend et al.14) previously reported five patients with aortitis and aortic incompetence due to systemic rheumatological disorders. Among these patients, three were treated successfully with immunosuppressive therapy involving steroids and cyclophosphamide. Zenagui et al.6) reported on a 38-year-old man who exhibited non-infectious aortic valve endocarditis associated with AOSD, which was successfully treated with 1 mg/kg prednisolone. Immunosuppressive regimens which principally use steroids and cyclophosphamide are of proven benefit in systemic vasculitides15, 16), and as aortitis and aortic valvulitis are vasculitic processes, a response to immunosuppression might be expected. Therefore, in an effort to control inflammation and thereby prevent hemodynamic instability, immunosuppressive therapy of active aortitis should be considered at an early stage.
In summary, this report describes an extremely rare case of cardiac valvular complication in AOSD. We believe that such cases require the careful vigilance of clinicians in order to ensure early diagnosis of this complication in AOSD patients, and that early appropriate immunosuppressive therapy may be useful for preventing hemodynamic instability due to valvular insufficiency.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





