 |
 |
| Korean J Intern Med > Volume 20(1); 2005 > Article |
|
Abstract
Background
The Diabcare-Asia study was designed for the purpose of describing diabetes control and management, and late complication status in the diabetic population.
Methods
From the 1st of July 2001 to the 1st of September 2001, data from 1170 diabetic patients were collected in 21 centers (one university hospital and 20 clinics located in Seoul and in Gyeonggi, Korea), and blood samples were collected for centralized HbA1c measurements.
Results
Only 16.8% of patients at the clinics reported self-monitoring their blood glucose. The mean HbA1c was 7.3┬▒1.4% at the hospital and 7.5┬▒1.5% at the clinics, and the mean fasting plasma glucose (FPG) levels were 7.0┬▒3.3 mmol/L at the hospital and 7.9┬▒2.5 mmol/L at the clinics. About 40% of patients had a HbA1c and FPG above the normal upper limits. Screening for microalbuminuria was rarely performed. The available data represents only about 0.9% of the patients at the hospital and 12.3% of the patients at the clinics. Nephropathy (serum creatinine >2 mg/dL) was found in 0.8% of the patients at the hospital and in 3.4% of the patients at the clinics. Retinopathy and neuropathy were commonly reported diabetic complications. The prevalence of other severe late complications was relatively low.
Diabetes mellitus is a common disease with a 4% worldwide prevalence1), and its prevalence is expected to increase to 5.4% by 20252). The incidence of diabetes in the Asian population seems to be on the rise and the incidence of late diabetes complications is also expected to correspondingly increase. This will eventually pose a major healthcare and economic problem.
In common with other countries that have undergone recent industrialization, the prevalence of diabetes has increased dramatically in Korea. While the prevalence of diabetes in Koreans was estimated to be less than 0.5% in the 1960's, recent studies from Yonchon and Jungup counties in 1993 and 1997 showed a dramatic increase to 7.2% and 7.1%, respectively3, 4).
Numerous studies have reported on the importance of good metabolic control to reduce, prevent or delay the progression of late diabetes complications, and this has resulted in a growing awareness of the need to improve care5-9). However, although an adequate knowledge of baseline status is fundamental to any future diabetes care program, no proper data have been available until now.
For this reason, the Diabcare-Asia project was designed with collaboration between Novo Nordisk Asia Pacific Pte. Ltd. and the participating Asian regions by working through their national diabetes associations. The project was initiated in 1997 in six regions, and it was subsequently extended to include 12 regions in 199810, 11). The results of the surveys that have undertaken have been very informative, and the Diabcare-Asia 2001 project was initiated to continue this work.
Unlike the 1997 and 1998 projects, both of which were carried out in specialized diabetes centers, the 2001 survey was carried out in primary healthcare facilities. It was a multi-country, multi-center observational study designed to profile the current status of diabetes control, diabetes management and diabetes complications in many Asian countries. The regions which participated were Korea, China, Indonesia, Malaysia, Philippines, Singapore, Taiwan, Thailand and Vietnam.
We report here upon the data of the Diabcare-Asia Study in Korea.
The study population included all patients that were registered for more than 12 months for the management of diabetes at the 21 described centers. It was planned to recruit all the patients within a period of two months. In Korea, the primary healthcare centers (clinics) are defined as hospitals having less than 20 beds that treat general diseases at the outpatient level. From the 1st of July 2001 to the 1st of September 2001, a total of 20 collection centers from Seoul and Gyeonggi (including Incheon) participated, and each center collected data from about 50 patients. One university hospital (Kyung Hee University Medical Center, Seoul) also participated. All the patients were selected randomly.
Each center contributed all the collected patient data by interview, laboratory assessments (for HbA1c only), and clinical examination information as detailed in the patients' medical records. Data were recorded on the Diabcare-Asia Data Collection Forms that were provided to each patient. The collected data included information on basic patient data, the type of diabetes, diabetes management, and self-monitoring (blood and urine glucose), glycemic control (HbA1c and FPG for one time), cardiovascular risk factors (smoking, alcohol, lipid profile, hypertension), renal function monitoring (serum creatinine, microalbuminuria, proteinuria), eye and foot examinations over the past 12 months, and severe late complications. Blood samples were obtained by finger pricking for the centralized HbA1c measurements, and they were taken from at least one-third of the recruited patients. Bio-Rad Asia was responsible for the appointment of a central laboratory for the participating centers and for the quality assurance of the centralized HbA1c determinations. HbA1c analyses were performed by automatic high-pressure liquid chromatography (Bio-Rad VARIANTŌäó, Bio-Rad Laboratories, Hercules, CA, USA). The reference range for this assay was 4.7% to 6.4%.
All data were entered into a Statistical Analysis System (SAS, Version 6.12; SAS Institute Inc., Cary, NC, USA) by electronic scanning (TELEform Elite, version 5.2; Cardiff Software, San Marcos, CA, USA), and a data entry program was used to validate the data quality and to generate any queries on missing/inconsistent/invalid data. The sub-groupings were created according to the clinic type of diabetes and the duration of diabetes. The response rates to all assessed variables were presented as percentages. Only descriptive statistical analysis was performed.
There were 1193 patients participating at the 21 centers, of which 23 patients (1.9%) were not included in the statistical analysis due to incomplete basic patient information. Hence, 1170 patients constituted the analysis. The number of patients recruited from the hospital (one center) was 118, and the number of patients recruited from the clinics (20 centers) was 1052.
In both the hospital and clinics, the majority (Ōēź97%) of the patients were diagnosed as having type 2 diabetes with a female preponderance of approximately 61% (Table 1). The patients' mean age was about 60 years and the mean age of diabetes onset was about 51 years. The patients treated at the hospital had suffered from diabetes for a slightly longer duration (10.2┬▒6.0 years) than those treated at the clinics (8.7┬▒5.8 years).
According to the guideline of the International Diabetes Institute Asia-Pacific12), obesity was defined as a BMI Ōēź23 kg/m2. The mean BMIs of all patients was approximately 25 kg/m2, and the majority of patients at both types of medical centers were obese (77% and 68% in the hospital and clinics, respectively).
Less than a quarter of the patients were smokers or alcohol drinkers, and the majority of the patients did not adhere to the diet plan recommended by a dietician, with more patients from the hospital (71%) ignoring the diet recommendations than the patients from the clinics (57%). Exercise did not appear to be a regular part of the life-style management of diabetes as a half (50% and 48% for hospital and clinics, respectively) of the patients seldom exercised. Over the previous 12 months, about 91% of the patients that visited the hospital received 1~2 days of education on diabetes compared to 31% of the patients who visited the clinics.
A higher proportion of patients treated at the hospital (64%) reported monitoring their own blood glucose levels compared to only 17% of the patients treated at the clinics who reported monitoring their own blood glucose levels (Table 2). A glucose meter was not commonly used for this purpose by the patients treated at clinics (19%) but was used by many of the patients treated at the hospital (63%). The monitoring of urine glucose levels was not commonly done by either group. The frequency of monitoring was low: 9 times/month using blood and twice/month using urine among patients in the clinics group and 7 times/month using blood among patients in the hospital group.
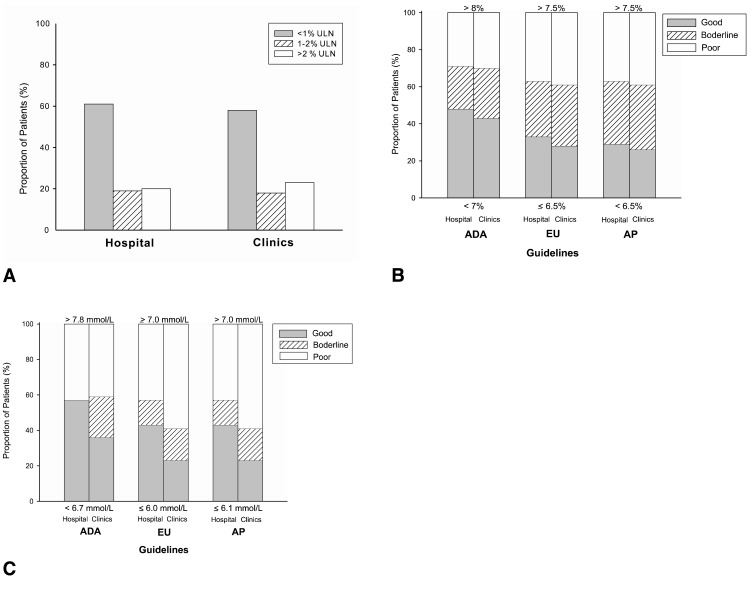
The HbA1c values in patients managed at the hospital and clinics were 7.3┬▒1.4% and 7.5┬▒1.5%, respectively. 59.7% of the patients at the hospital and 99.2% of the patients at the clinics had their HbA1c levels assessed by a local laboratory. To assess the level of patient control of glycemia, the mean central HbA1c values were categorized according to upper limits of the normal range (UNL); as <1% ULN (good), 1~2% UNL (borderline), and >2% ULN (poor). Approximately 40% of the patients were considered to have inappropriate glycemic control (borderline or poor, 39% and 41%, respectively) (Figure 1A).
The proportion of patients with satisfactory glycemic control of HbA1c was also assessed by using the guidelines of the American Diabetes Association13) (HbA1c <7%, 7~8%, >8%), the guidelines of the European Diabetes Policy Group14) (HbA1c Ōēż6.5%, 6.5~7.5%, >7.5%) and the guidelines of the Asia Pacific Type 2 Diabetes Policy Group15) (HbA1c <6.5%, 6.5~7.5%, >7.5%). Figure 1B summarizes the central HbA1c profiles according to the 3 different guidelines used for these categories by the hospital and clinics. The HbA1c level in at least 50% of the patients was not ideal, as indicated by the different guidelines (hospital vs. clinics, respectively): 52% and 57% had HbA1c Ōēź7% (ADA); 67% and 72% had HbA1c >6.5% (EU); 71% and 74% had HbA1c Ōēź6.5% (AP).
The proportion of patients with satisfactory glycemic control of fasting plasma glucose (FPG) was also assessed by using the guidelines of the American Diabetes Association13) (FPG <6.7 mmol/L, 6.7~7.8 mmol/L, >7.8 mmol/L), the guidelines of the European Diabetes Policy Group14) (FPG Ōēż6 mmol/L, 6~7 mmol/L, Ōēź7 mmol/L) and the guidelines of the Asia Pacific Type 2 Diabetes Policy Group15) (FPG Ōēż6.1 mmol/L, 6.1~7.0 mmol/L, >7.0 mmol/L). Figure 1C presents the patient FPG profiles according to the three different guidelines, where glycemia in Ōēź 43% of the patients was not optimally controlled (hospital vs. clinics, respectively): 43% and 64% had FPG Ōēź6.7 mmol/L (ADA); 57% and 77% had FPG >6.0 mmol/L (EU); and 57% and 77% had FPG >6.1 mmol/L (AP). It appeared that the control of blood glucose was not optimal in a higher proportion of patients managed at the clinics than for the patients managed at the hospital.
Lipid measurements were performed in 93% and 74% of the patients managed at the hospital and clinics, respectively. The mean cholesterol levels were comparable in the two groups; it was approximately 5.0 mmol/L. Both groups of patients appeared to have good control of the HDL-cholesterol (HDL-C) levels, and approximately 42% of the patients in both groups had a HDL-C >1.2 mmol/L. This tendency was also reflected in the proportion of patients with optimal control of the TG levels at below <1.7 mmol/L, 62% vs. 45% of patients in hospital and clinics, respectively. Approximately 17% of patients in both groups indicated that they were being treated for hyperlipidemia. Statins were commonly used to lower the lipid levels for both patient groups.
More patients managed at the hospital (57%) were treated for hypertension than were the patients being managed at the clinics (46%). Ca2+ antagonist (30%) was more commonly prescribed to treat hypertension in clinics. However, ╬▓-blockers (25%) were more commonly prescribed in the hospital.
The tests for abnormal levels of serum creatinine (63% of patients were tested in clinics vs. 92% of patients in the hospital) and proteins in urine (70% of the patients were tested in clinics vs. 92% of patients in the hospital) were more commonly carried out for the patients than were tests for trace levels of albumin (microalbuminuria; 12% of patients were tested in clinics vs. 1% of patients in the hospital). However, the tests for abnormal levels of serum creatinine and urinary proteins were carried out more often at the hospital than at the clinics. Despite the low proportion of patients that had their albumin level measured, the test was more often carried out in patients managed at clinics (12%), and only 1% of patients were tested at the hospital (Table 3).
The prevalence of abnormal levels of serum creatinine (5%) and protein (16%) was low among the patients attending clinics. Only 1% of the patients attending the hospital had a serum creatinine > 2 mg/dL, but almost 60% of the patients had abnormal levels of protein.
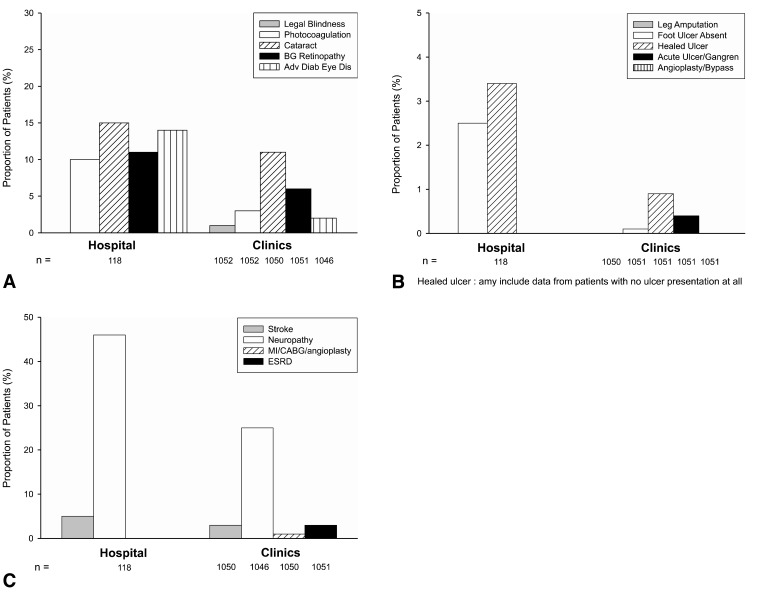
The eye examination for complications included screening for legal blindness, photocoagulation, cataract, background retinopathy, and advanced diabetic eye disease. Eye examinations had been carried during the previous 12 months in 51% of patients at the hospital and in 48% of patients at the clinics. The most commonly reported eye complication was cataract: 15% of patients at the hospital and 11% of the patients at the clinics had cataract. The frequencies of photocoagulation, background retinopathy and advanced diabetes eye disease were higher in patients attending the hospital (Figure 2A).
The examination for extremity complications included screening for leg amputation, absence of a foot pulse, a healed ulcer, acute ulcer/gangrene, and bypass/angioplasty. During the previous 12 months, 48% and 54% of patients at the hospital and clinics, respectively, had received a foot examination. The prevalence of complications related to the feet was low (<1%) among the patients treated at the clinics compared to patients treated at the hospital. The absence of a foot pulse (2.5%) and the presence of a healed ulcer (3.4%) were reported by the hospital patients (Figure 2B).
Other complications examined were; cerebral stroke, signs of neuropathy, myocardial infarction/coronary artery bypass graft/angioplasty (MI/CABG/angioplasty), and end-stage renal failure. In both groups of patients, neuropathy was common, with a higher frequency reported in the hospital group (46%) than in the clinic group (25%). The prevalence of other severe complications was low (Ōēż5%) in both groups. MI/CABG/angioplasty and end stage renal failure were absent in the patients managed at the hospital, but these maladies were reported at low frequency by the clinic patients (Figure 2C).
The objectives of this Diabcare - Korea study were to describe the diabetes control management and the complication status of the Korean diabetes population. Since the DCCT5-7) and UKPDS8, 9) showed that poor diabetic control over an extended period contributes to chronic diabetic complications, and they also demonstrated a relationship between the blood glucose level and the risk of diabetes complications, efforts should be directed towards helping the patients maintain normoglycemia.
In terms of their demographic characteristics, the patients were considered obese if they had a mean BMI Ōēź 25 kg/m2. In the present study, the majority of patients in both groups were found to be obese (77% and 68% in the hospital and clinics, respectively). This result indicates that obesity has an important association with type 2 diabetes.
Although dietary control is an essential component of diabetes management, the majority of the patients did not follow the diet plans recommended by dieticians. Future studies must address this issue to help define and recommend appropriate nutritional guidelines for the patients as an integral part of diabetes health care.
One unsatisfactory result was that only 17% of patients treated at the clinics reported any form of home glucose monitoring compared with a much higher proportion of hospital patients who monitored their glucose (64%). These numbers were lower than those reported in the NHANES III study16), which indicated that almost 47% of American diabetes patients with a HbA1c Ōēź8%, and 32% of those with a HbA1c <8% performed home blood glucose monitoring at least once daily. Thus, there is a need to educate patients at the clinics on the importance of home glucose monitoring.
Of the 1,170 patients surveyed, about 743 patients (99.2% at the hospital and 59.7% at the clinics) had data on their HbA1c measurement. But about 40% of patients had a HbA1c > 7.4% (>1% above the upper limit of the normal range) and over 40% had an FPG >7.8 mmol/L. Hence both the HbA1c data and the FPG data suggest that many Korean patients had relatively poor glycemic control. Recent results from the United Kingdom Prospective Diabetes Study (UKPDS)8, 9) have shown a continuous relationship between the risks of microvascular complications and glycemia, such that for every percentage point of decrease in HbA1c, there is a 35% reduction in the risk of complications.
Screening for microalbuminuria was rarely performed, as indicated by the availability of data for only about 0.9% of hospital patients and 12.3% of clinic patients. Of these patients, nephropathy (serum creatinine >2 mg/dL) was present in 0.9% and 5.4% of the hospital and clinic patients, respectively. However, this result should be interpreted with care due to the low frequency of testing in patients. Because microalbuminuria is a useful indicator of the early manifestations of nephropathy, and it is also a marker of increased cardiovascular morbidity and mortality for diabetic patients, more screening tests for microalbuminuria are necessary for the Korean patients.
The proportion of diabetes patients with retinopathy in this study was 50% in the hospital group and 23% in the clinic group. The prevalence of complications related to the feet was 0.9% among the clinic patients and 5.9% among the hospital patients. Neuropathy was common in both patient groups, with 46% of patients reporting neuropathy in the hospital group and 25% of patients reporting neuropathy in the clinics group. The early detection and treatment of these complications are known to be clinically effective at preventing the progression of severe late complications.
The prevalence of other severe complications was relatively low (Ōēż5%) in both groups. MI/CABG/angioplasty and end stage renal failure were absent in hospital patients, but they were reported at a low frequency in the clinic patients.
In conclusion, the data obtained from this stratified sample of clinic and hospital based diabetes patients in Korea showed that many patients had sub-optimal glycemia control and that microalbuminuria screening was infrequently done. The DCCT and UKPDS has shown that chronic poor diabetes control contributes to long term diabetic complications and that near normal glycemic control reduces and delays the onset of microvascular complications. These findings call for greater efforts at establishing and maintaining improved diabetes management with regards to glycemia control and microalbuminuria screening.
In addition, the findings of this study suggest the importance of empowering patients to adopt diabetes self-care skills, of improving diabetes education, of organizing diet plans, and of modifying the patients' known risk factors. Greater encouragement is needed to enable patients to make continued efforts in achieving optimal glycemic control. Better relationships between diabetes healthcare providers and patients, a more comprehensive diabetes service, and better patient cooperation with therapy are also recommended.
However, this study has some limitations. In particular, the random method of patient selection in the specific regions and centers used in this study was insufficient to reflect the overall Korean situation. Moreover, this selection bias may have affected the prevalence of diabetes related complications. However, despite its limitations, this study does provide valuable information on the current status of diabetes care and it also provides a fundamental data foundation for future improvements.
ACKNOWLEDGEMENT
Diabcare-asia 2001 study group members in Korea
Dr. Kwan Soo Hong, Cecil Clinics, Seoul; Dr. Young Suk Yoon, Yoon's Medical Clinic Hemodialysis Center, Seoul; Dr. Jung Back Kim, Kim's IM Clinic, Seoul; Dr. Seung Hwon Sohn, Dr. Sohn's Hemodialysis Center, Seoul; Dr. Yeo Wun Yoon, Seong Dong People's Clinic, Seoul; Dr. Ho Joon Jo, Jo's IM Clinic, Seoul; Dr. Dong Sub Kim, Kim Dong Sub Internal Medicine Clinic, Seoul; Dr. Young Geun Yoon, Dr. Yoon's IM Clinic, Seoul; Dr. Kyung Hwan Son, Son's IM Clinic, Seoul; Dr. Hyung Keun Chung, Chung's IM Clinic, Seoul; Dr. Jong Eun Park, Park's IM Clinic, Seoul; Dr. Tae Bin Kim, Dr. Kim's Internal Medicine Clinic, Gyeonggi; Dr. Hyeon Su Kim, Hyeon Medical Clinic, Gyeonggi; Dr. Woo Jin Jeong, Jeong's IM Clinic, Gyeonggi; Dr. Yeun Ho Nam, Nam's IM Clinic, Gyeonggi; Dr. Young Gil Yoo, Yoo Young Gil Int. Med. Clinic, Gyeonggi; Dr. Seung Joo Lee, Dr. Lee's IM Clinic, Gyeonggi; Dr. Hyun Il Chun, Dr. Chun's IM Clinic, Gyeonggi; Dr. Hyuk Ho Kwon, Dr. Kwon's IM Clinic, Gyeonggi; Dr. Suk Hwan Yoo, Yoo Suk Hwan Int. Med. Clinic, Incheon; Professor Young Seol Kim, Kyung Hee University Medical Center, Seoul
This study was made possible by a research grant provided generously by Novo Nordisk Pharma Korea.
References
1. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998;21:1414ŌĆō1431PMID : 9727886.


2. Cockram CS. The epidemiology of diabetes mellitus in the Asia-Pacific region. Hong Kong Med J 2000;6:43ŌĆō52PMID : 10793402.

3. Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in yonchon county, South Korea. Diabetes Care 1995;18:545ŌĆō548PMID : 7497867.


4. Kim YI, Choi CS, Kim SW, Lee JS, Kim HH, Lee MS, Lee SI, Park JY, Hong SK, Lee KU. Prevalence of diabetes mellitus and impaired glucose tolerance in Korean adults living in Jungup district, South Korea. J Korean Diabetes Assoc 1998;22:363ŌĆō371.
5. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977ŌĆō986PMID : 8366922.


6. The Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes therapy on measures of autonomic nervous system function in the diabetes control and complications trial (DCCT). Diabetologia 1998;41:416ŌĆō423PMID : 9562345.




7. The Diabetes Control and Complications Trial Research Group. Effect of intensive therapy on the development and progression of diabetic nephropathy in the diabetes control and complications trial. Kidney Int 1995;47:1703ŌĆō1720PMID : 7643540.


8. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837ŌĆō853PMID : 9742976.


9. UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854ŌĆō865PMID : 9742977.


10. Nitiyanant W, Tandhanand S, Mahtab H, Zhu XX, Pan CY, Raheja BS, Sathe SR, Soegondo S, Soewondo P, Kim YS, Embong M, Lantion-Ang L, Lim-Abraham MA, Lee WW, Wijesuriya M, Tai TY, Chuang LM, Le HL, Cockram C, Jorgensen LN, Yeo JP. The Diabcare-Asia 1998 study: outcomes on control and complications in type 1 and type 2 diabetic patients. Curr Med Res Opin 2002;18:317ŌĆō327PMID : 12240795.


11. Chuang LM, Tsai ST, Huang BY, Tai TY. The status of diabetes control in Asia: a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med 2002;19:978ŌĆō985PMID : 12647837.


12. The Asia-Pacific Perspective. Redefining obesity and its treatment. 2000;Health Communications Australia Pty.
13. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2002;25:213ŌĆō229PMID : 11772918.



14. European Diabetes Policy Group. A desktop guide to type 2 diabetes mellitus. Diabet Med 1999;16:716ŌĆō730PMID : 10510947.


15. Type 2 diabetes: practical targets and treatments. 2002;3rd ed. Health Communications Australia Pty Limited.
Figure┬Ā1
Glycemic Control.
(A) According to the Upper Limits in the Normal Range
(B) According to Different Guidelines (HbA1c)
(C) According to the Different Guidelines (FPG)
Figure┬Ā2
Diabetes Related Complications
(A) Eye Complications
(B) Extremity Complications
(C) Other Complications
Table┬Ā1
Patient Demographics According to Diabetes Clinic Type

N, number of sets of valid patient data used in the analysis
n (%), number of patients (percent patients)
Obesity was defined as a BMIŌēź23 kg/m2, according to the Asia-Pacific guideline12)
BMI was measured for patients with an ageŌēź21 years
Table┬Ā3
Renal Function

N, number of sets of valid patient data used in the analysis
n (%), number of patients (percent)
*albumin levels of : 20~300 mg/L or 30~300 mg/24h or an albumin/creatinine ratio of 2.5 to 25 mg/mol (male) or 3.5 to 25 mg/mol (female)
Proteinuria was tested by urinary dip stick.
+/- : 30 mg/dL, + : 100 mg/dL, ++ : 300 mg/dL, ++++ : 1000 mg/dL, >++++ : >1000 mg/dL




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



