2. Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr 1997;127(5 Suppl):990SŌĆō991S.


8. Carrero JJ, Thomas F, Nagy K, et al. Global prevalence of protein-energy wasting in kidney disease: a meta-analysis of contemporary observational studies from the international society of renal nutrition and metabolism. J Ren Nutr 2018;28:380ŌĆō392.


9. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing 2010;39:412ŌĆō423.


10. Pereira RA, Cordeiro AC, Avesani CM, et al. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant 2015;30:1718ŌĆō1725.


12. Ren H, Gong D, Jia F, Xu B, Liu Z. Sarcopenia in patients undergoing maintenance hemodialysis: incidence rate, risk factors and its effect on survival risk. Ren Fail 2016;38:364ŌĆō371.


13. Hotta C, Hiraki K, Wakamiya A, et al. Relation of physical function and physical activity to sarcopenia in hemodialysis patients: a preliminary study. Int J Cardiol 2015;191:198ŌĆō200.


25. Kim JK, Choi SR, Choi MJ, et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr 2014;33:64ŌĆō68.


26. Lin YL, Liou HH, Lai YH, et al. Decreased serum fatty acid binding protein 4 concentrations are associated with sarcopenia in chronic hemodialysis patients. Clin Chim Acta 2018;485:113ŌĆō118.


28. Bataille S, Serveaux M, Carreno E, Pedinielli N, Darmon P, Robert A. The diagnosis of sarcopenia is mainly driven by muscle mass in hemodialysis patients. Clin Nutr 2017;36:1654ŌĆō1660.


30. AsŌĆÖhabi A, Najafi I, Tabibi H, Hedayati M. Prevalence of sarcopenia and dynapenia and their determinants in Iranian peritoneal dialysis patients. Iran J Kidney Dis 2018;12:53ŌĆō60.

31. Lopes LCC, Mota JF, Prestes J, et al. Intradialytic resistance training improves functional capacity and lean mass gain in individuals on hemodialysis: a randomized pilot trial. Arch Phys Med Rehabil 2019;100:2151ŌĆō2158.


34. Koh KP, Fassett RG, Sharman JE, Coombes JS, Williams AD. Effect of intradialytic versus home-based aerobic exercise training on physical function and vascular parameters in hemodialysis patients: a randomized pilot study. Am J Kidney Dis 2010;55:88ŌĆō99.


35. Allman MA, Stewart PM, Tiller DJ, Horvath JS, Duggin GG, Truswell AS. Energy supplementation and the nutritional status of hemodialysis patients. Am J Clin Nutr 1990;51:558ŌĆō562.


36. Eustace JA, Coresh J, Kutchey C, et al. Randomized double-blind trial of oral essential amino acids for dialysis-associated hypoalbuminemia. Kidney Int 2000;57:2527ŌĆō2538.


37. Hiroshige K, Sonta T, Suda T, Kanegae K, Ohtani A. Oral supplementation of branched-chain amino acid improves nutritional status in elderly patients on chronic haemodialysis. Nephrol Dial Transplant 2001;16:1856ŌĆō1862.


38. Zilles M, Betz C, Jung O, et al. How to prevent renal cachexia? A clinical randomized pilot study testing oral supplemental nutrition in hemodialysis patients with and without human immunodeficiency virus infection. J Ren Nutr 2018;28:37ŌĆō44.


39. Pupim LB, Majchrzak KM, Flakoll PJ, Ikizler TA. Intradialytic oral nutrition improves protein homeostasis in chronic hemodialysis patients with deranged nutritional status. J Am Soc Nephrol 2006;17:3149ŌĆō3157.


41. Stein A, Moorhouse J, Iles-Smith H, et al. Role of an improvement in acid-base status and nutrition in CAPD patients. Kidney Int 1997;52:1089ŌĆō1095.


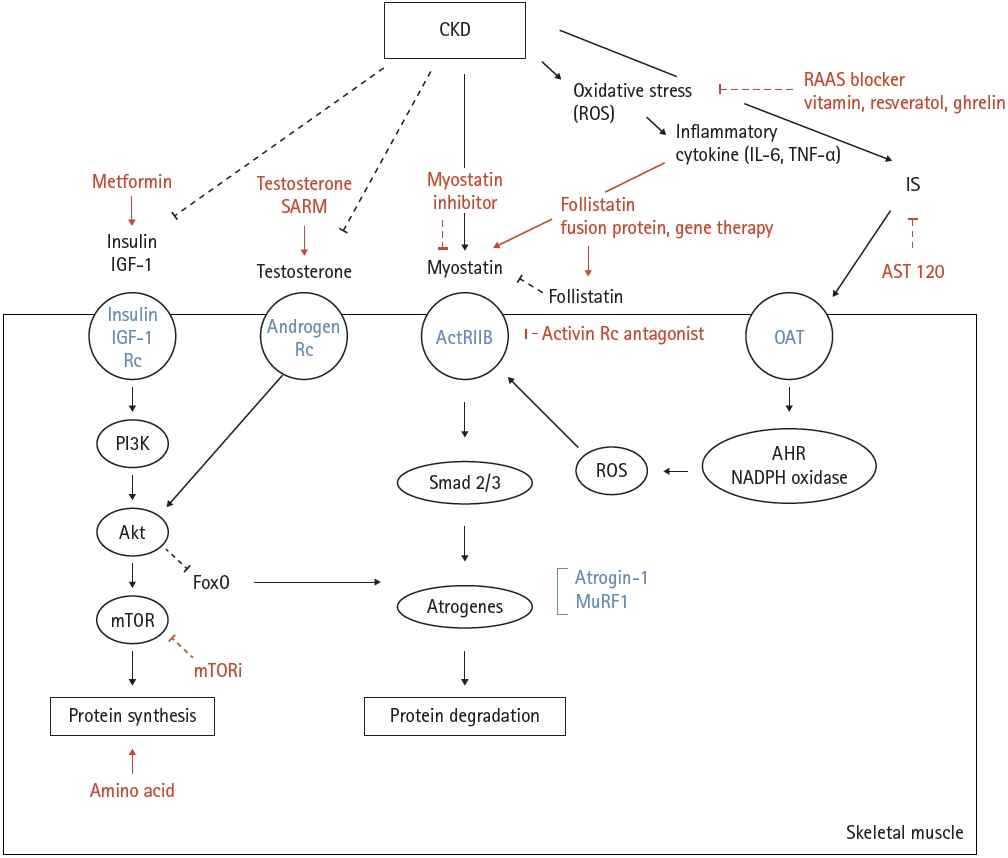
42. Stenvinkel P, Carrero JJ, von Walden F, Ikizler TA, Nader GA. Muscle wasting in end-stage renal disease promulgates premature death: established, emerging and potential novel treatment strategies. Nephrol Dial Transplant 2016;31:1070ŌĆō1077.


45. Adey D, Kumar R, McCarthy JT, Nair KS. Reduced synthesis of muscle proteins in chronic renal failure. Am J Physiol Endocrinol Metab 2000;278:E219ŌĆōE225.


48. Raj DS, Dominic EA, Wolfe R, et al. Coordinated increase in albumin, fibrinogen, and muscle protein synthesis during hemodialysis: role of cytokines. Am J Physiol Endocrinol Metab 2004;286:E658ŌĆōE664.


52. Bodine SC, Latres E, Baumhueter S, et al. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science 2001;294:1704ŌĆō1708.


53. Stitt TN, Drujan D, Clarke BA, et al. The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors. Mol Cell 2004;14:395ŌĆō403.


56. Lee SW, Dai G, Hu Z, Wang X, Du J, Mitch WE. Regulation of muscle protein degradation: coordinated control of apoptotic and ubiquitin-proteasome systems by phosphatidylinositol 3 kinase. J Am Soc Nephrol 2004;15:1537ŌĆō1545.

58. Morley JE. Hormones and sarcopenia. Curr Pharm Des 2017;23:4484ŌĆō4492.


60. Johansen KL, Chertow GM, Foley RN, et al. US renal data system 2020 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2021;77(4 Suppl 1):A7ŌĆōA8.


63. Kim TN, Park MS, Yang SJ, et al. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care 2010;33:1497ŌĆō1499.


65. Abbatecola AM, Ferrucci L, Ceda G, et al. Insulin resistance and muscle strength in older persons. J Gerontol A Biol Sci Med Sci 2005;60:1278ŌĆō1282.


66. Abbatecola AM, Paolisso G. Is there a relationship between insulin resistance and frailty syndrome? Curr Pharm Des 2008;14:405ŌĆō410.


72. Giannocco G, Oliveira KC, Crajoinas RO, et al. Dipeptidyl peptidase IV inhibition upregulates GLUT4 translocation and expression in heart and skeletal muscle of spontaneously hypertensive rats. Eur J Pharmacol 2013;698:74ŌĆō86.


73. Holmes BF, Kurth-Kraczek EJ, Winder WW. Chronic activation of 5ŌĆÖ-AMP-activated protein kinase increases GLUT-4, hexokinase, and glycogen in muscle. J Appl Physiol (1985) 1999;87:1990ŌĆō1995.


74. Pawelczyk L, Spaczynski RZ, Banaszewska B, Duleba AJ. Metformin therapy increases insulin-like growth factor binding protein-1 in hyperinsulinemic women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol 2004;113:209ŌĆō213.


75. Hern├Īndez-├ülvarez D, Mena-Montes B, Toledo-P├®rez R, et al. Long-term moderate exercise combined with metformin treatment induces an hormetic response that prevents strength and muscle mass loss in old female wistar rats. Oxid Med Cell Longev 2019;2019:3428543.


77. Das S, Behera SK, Srinivasan A, et al. Effect of metformin on exercise capacity: a meta-analysis. Diabetes Res Clin Pract 2018;144:270ŌĆō278.


78. Dousdampanis P, Trigka K, Fourtounas C, Bargman JM. Role of testosterone in the pathogenesis, progression, prognosis and comorbidity of men with chronic kidney disease. Ther Apher Dial 2014;18:220ŌĆō230.


79. Leavey SF, Weitzel WF. Endocrine abnormalities in chronic renal failure. Endocrinol Metab Clin North Am 2002;31:107ŌĆō119.


80. Palmer BF. Sexual dysfunction in uremia. J Am Soc Nephrol 1999;10:1381ŌĆō1388.


82. Axell AM, MacLean HE, Plant DR, et al. Continuous testosterone administration prevents skeletal muscle atrophy and enhances resistance to fatigue in orchidectomized male mice. Am J Physiol Endocrinol Metab 2006;291:E506ŌĆōE516.


88. Corona G, Maseroli E, Maggi M. Injectable testosterone undecanoate for the treatment of hypogonadism. Expert Opin Pharmacother 2014;15:1903ŌĆō1926.


102. Li JB, Jefferson LS. Influence of amino acid availability on protein turnover in perfused skeletal muscle. Biochim Biophys Acta 1978;544:351ŌĆō359.


104. Anthony JC, Yoshizawa F, Anthony TG, Vary TC, Jefferson LS, Kimball SR. Leucine stimulates translation initiation in skeletal muscle of postabsorptive rats via a rapamycin-sensitive pathway. J Nutr 2000;130:2413ŌĆō2419.


106. Grodstein GP, Blumenkrantz MJ, Kopple JD. Nutritional and metabolic response to catabolic stress in uremia. Am J Clin Nutr 1980;33:1411ŌĆō1416.


107. Kalantar-Zadeh K, Mehrotra R, Fouque D, Kopple JD. Poor nutritional status and inflammation: metabolic acidosis and malnutritionŌĆÉinflammation complex syndrome in chronic renal failure. Semin Dial 2004;17:455ŌĆō465.


108. Pickering WP, Price SR, Bircher G, Marinovic AC, Mitch WE, Walls J. Nutrition in CAPD: serum bicarbonate and the ubiquitin-proteasome system in muscle. Kidney Int 2002;61:1286ŌĆō1292.


109. Wolfson M, Jones MR, Kopple JD. Amino acid losses during hemodialysis with infusion of amino acids and glucose. Kidney Int 1982;21:500ŌĆō506.


110. Ikizler TA, Flakoll PJ, Parker RA, Hakim RM. Amino acid and albumin losses during hemodialysis. Kidney Int 1994;46:830ŌĆō837.


111. Chazot C, Shahmir E, Matias B, Laidlaw S, Kopple JD. Dialytic nutrition: provision of amino acids in dialysate during hemodialysis. Kidney Int 1997;52:1663ŌĆō1670.


112. Mak RH. Insulin resistance but IGF-I sensitivity in chronic renal failure. Am J Physiol 1996;271(1 Pt 2):F114ŌĆōF119.


114. Fouque D, Peng SC, Shamir E, Kopple JD. Recombinant human insulin-like growth factor-1 induces an anabolic response in malnourished CAPD patients. Kidney Int 2000;57:646ŌĆō654.


115. Kopple JD, Cianciaruso B, Massry SG. Does parathyroid hormone cause protein wasting? Contrib Nephrol 1980;20:138ŌĆō148.


116. Fouque D, Kalantar-Zadeh K, Kopple J, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 2008;73:391ŌĆō398.


117. Ikizler TA, Burrowes JD, Byham-Gray LD, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis 2020;76(3 Suppl 1):S1ŌĆōS107.


118. Haba Y, Fujimura T, Oyama K, et al. Effect of oral branched-chain amino acids and glutamine supplementation on skeletal muscle atrophy after total gastrectomy in rat model. J Surg Res 2019;243:281ŌĆō288.


122. Acchiardo S, Moore L, Cockrell S. Effect of essential amino acids (EAA) on chronic hemodialysis (CHD) patients (PTS). Trans Am Soc Artif Intern Organs 1982;28:608ŌĆō614.

123. Wu H, Xia Y, Jiang J, et al. Effect of beta-hydroxy-beta-methylbutyrate supplementation on muscle loss in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr 2015;61:168ŌĆō175.


127. Workeneh BT, Rondon-Berrios H, Zhang L, et al. Development of a diagnostic method for detecting increased muscle protein degradation in patients with catabolic conditions. J Am Soc Nephrol 2006;17:3233ŌĆō3239.


128. Elkasrawy MN, Hamrick MW. Myostatin (GDF-8) as a key factor linking muscle mass and bone structure. J Musculoskelet Neuronal Interact 2010;10:56ŌĆō63.

129. Han HQ, Zhou X, Mitch WE, Goldberg AL. Myostatin/activin pathway antagonism: molecular basis and therapeutic potential. Int J Biochem Cell Biol 2013;45:2333ŌĆō2347.


131. Trendelenburg AU, Meyer A, Rohner D, Boyle J, Hatakeyama S, Glass DJ. Myostatin reduces Akt/TORC1/p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am J Physiol Cell Physiol 2009;296:C1258ŌĆōC1270.


132. Argil├®s JM, Orp├Ł M, Busquets S, L├│pez-Soriano FJ. Myostatin: more than just a regulator of muscle mass. Drug Discov Today 2012;17:702ŌĆō709.


135. Verzola D, Procopio V, Sofia A, et al. Apoptosis and myostatin mRNA are upregulated in the skeletal muscle of patients with chronic kidney disease. Kidney Int 2011;79:773ŌĆō782.


138. Becker C, Lord SR, Studenski SA, et al. Myostatin antibody (LY2495655) in older weak fallers: a proof-of-concept, randomised, phase 2 trial. Lancet Diabetes Endocrinol 2015;3:948ŌĆō957.


139. Wagner KR, Fleckenstein JL, Amato AA, et al. A phase I/IItrial of MYO-029 in adult subjects with muscular dystrophy. Ann Neurol 2008;63:561ŌĆō571.


147. Castonguay R, Lachey J, Wallner S, et al. Follistatin-288-Fc fusion protein promotes localized growth of skeletal muscle. J Pharmacol Exp Ther 2019;368:435ŌĆō445.


150. Statland JM, Campbell C, Desai U, et al. Randomized phase 2 study of ACE-083, a muscle-promoting agent, in facioscapulohumeral muscular dystrophy. Muscle Nerve 2022;66:50ŌĆō62.


157. Axelsson J, Heimb├╝rger O, Stenvinkel P. Adipose tissue and inflammation in chronic kidney disease. Contrib Nephrol 2006;151:165ŌĆō174.


159. Ramalingam L, Menikdiwela K, LeMieux M, et al. The renin angiotensin system, oxidative stress and mitochondrial function in obesity and insulin resistance. Biochim Biophys Acta Mol Basis Dis 2017;1863:1106ŌĆō1114.


161. Allen AM, Zhuo J, Mendelsohn FA. Localization and function of angiotensin AT1 receptors. Am J Hypertens 2000;13(1 Pt 2):31SŌĆō38S.


162. Linderman JR, Greene AS. Distribution of angiotensin II receptor expression in the microcirculation of striated muscle. Microcirculation 2001;8:275ŌĆō281.


164. Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002;288:2421ŌĆō2431.


165. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001;345:851ŌĆō860.


166. Jafar TH, Schmid CH, Landa M, et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 2001;135:73ŌĆō87.


167. Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med 2001;134:629ŌĆō636.


168. Onder G, Penninx BW, Balkrishnan R, et al. Relation between use of angiotensin-converting enzyme inhibitors and muscle strength and physical function in older women: an observational study. Lancet 2002;359:926ŌĆō930.


176. Levi A, Cohen E, Levi M, Goldberg E, Garty M, Krause I. Elevated serum homocysteine is a predictor of accelerated decline in renal function and chronic kidney disease: a historical prospective study. Eur J Intern Med 2014;25:951ŌĆō955.


177. Bostom AG, Shemin D, Verhoef P, et al. Elevated fasting total plasma homocysteine levels and cardiovascular disease outcomes in maintenance dialysis patients. A prospective study. Arterioscler Thromb Vasc Biol 1997;17:2554ŌĆō2558.

178. Robinson K, Gupta A, Dennis V, et al. Hyperhomocysteinemia confers an independent increased risk of atherosclerosis in end-stage renal disease and is closely linked to plasma folate and pyridoxine concentrations. Circulation 1996;94:2743ŌĆō2748.


181. Ng TP, Aung KC, Feng L, Scherer SC, Yap KB. Homocysteine, folate, vitamin B-12, and physical function in older adults: cross-sectional findings from the Singapore Longitudinal Ageing Study. Am J Clin Nutr 2012;96:1362ŌĆō1368.


184. Padayatty SJ, Katz A, Wang Y, et al. Vitamin C as an antioxidant: evaluation of its role in disease prevention. J Am Coll Nutr 2003;22:18ŌĆō35.


186. Konopacka M, Rzeszowska-Wolny J. Antioxidant vitamins C, E and beta-carotene reduce DNA damage before as well as after gamma-ray irradiation of human lymphocytes
in vitro. Mutat Res 2001;491:1ŌĆō7.

187. Polj┼Īak B, Raspor P. The antioxidant and pro-oxidant activity of vitamin C and trolox
in vitro: a comparative study. J Appl Toxicol 2008;28:183ŌĆō188.


188. Liu X, Wang P, Zou YX, Luo ZG, Tamer TM. Co-encapsulation of vitamin C and ╬▓-carotene in liposomes: storage stability, antioxidant activity, and
in vitro gastrointestinal digestion. Food Res Int 2020;136:109587.


189. Takahashi N, Morimoto S, Okigaki M, et al. Decreased plasma level of vitamin C in chronic kidney disease: comparison between diabetic and non-diabetic patients. Nephrol Dial Transplant 2011;26:1252ŌĆō1257.


192. Bauer JM, Verlaan S, Bautmans I, et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc 2015;16:740ŌĆō747.


193. Beaudart C, Buckinx F, Rabenda V, et al. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab 2014;99:4336ŌĆō4345.


194. Murad MH, Elamin KB, Abu Elnour NO, et al. The effect of vitamin D on falls: a systematic review and meta-analysis. J Clin Endocrinol Metab 2011;96:2997ŌĆō3006.


195. Nelsestuen GL, Zytkovicz TH, Howard JB. The mode of action of vitamin K. Identification of gamma-carboxyglutamic acid as a component of prothrombin. J Biol Chem 1974;249:6347ŌĆō6350.

199. Cranenburg EC, Schurgers LJ, Uiterwijk HH, et al. Vitamin K intake and status are low in hemodialysis patients. Kidney Int 2012;82:605ŌĆō610.


201. van Ballegooijen AJ, van Putten SR, Visser M, Beulens JW, Hoogendijk EO. Vitamin K status and physical decline in older adults-The Longitudinal Aging Study Amsterdam. Maturitas 2018;113:73ŌĆō79.


205. Harikumar KB, Aggarwal BB. Resveratrol: a multitargeted agent for age-associated chronic diseases. Cell Cycle 2008;7:1020ŌĆō1035.


208. Liao ZY, Chen JL, Xiao MH, et al. The effect of exercise, resveratrol or their combination on Sarcopenia in aged rats via regulation of AMPK/Sirt1 pathway. Exp Gerontol 2017;98:177ŌĆō183.


213. Hosoda H, Kojima M, Matsuo H, Kangawa K. Purification and characterization of rat des-Gln14-Ghrelin, a second endogenous ligand for the growth hormone secretagogue receptor. J Biol Chem 2000;275:21995ŌĆō22000.


214. Hosoda H, Kojima M, Matsuo H, Kangawa K. Ghrelin and des-acyl ghrelin: two major forms of rat ghrelin peptide in gastrointestinal tissue. Biochem Biophys Res Commun 2000;279:909ŌĆō913.


215. Rodriguez Ayala E, Pecoits-Filho R, Heimb├╝rger O, Lindholm B, Nordfors L, Stenvinkel P. Associations between plasma ghrelin levels and body composition in end-stage renal disease: a longitudinal study. Nephrol Dial Transplant 2004;19:421ŌĆō426.


216. DeBoer MD, Zhu XX, Levasseur P, et al. Ghrelin treatment causes increased food intake and retention of lean body mass in a rat model of cancer cachexia. Endocrinology 2007;148:3004ŌĆō3012.


218. Miyazaki T, Tanaka N, Hirai H, et al. Ghrelin level and body weight loss after esophagectomy for esophageal cancer. J Surg Res 2012;176:74ŌĆō78.


219. Argil├®s JM, Stemmler B. The potential of ghrelin in the treatment of cancer cachexia. Expert Opin Biol Ther 2013;13:67ŌĆō76.


220. Garcia JM, Boccia RV, Graham CD, et al. Anamorelin for patients with cancer cachexia: an integrated analysis of two phase 2, randomised, placebo-controlled, double-blind trials. Lancet Oncol 2015;16:108ŌĆō116.


221. Temel J, Bondarde S, Jain M, Yan Y, Duus E, Allen S. Efficacy and safety results from a phase II study of anamorelin HCl, a ghrelin receptor agonist. NSCLC patients. J Cachexia Sarcopenia Muscle 2013;4:295ŌĆō343.


222. White HK, Petrie CD, Landschulz W, et al. Effects of an oral growth hormone secretagogue in older adults. J Clin Endocrinol Metab 2009;94:1198ŌĆō1206.


224. Ohtsuki S, Asaba H, Takanaga H, et al. Role of blood-brain barrier organic anion transporter 3 (OAT3) in the efflux of indoxyl sulfate, a uremic toxin: its involvement in neurotransmitter metabolite clearance from the brain. J Neurochem 2002;83:57ŌĆō66.


225. Deguchi T, Ohtsuki S, Otagiri M, et al. Major role of organic anion transporter 3 in the transport of indoxyl sulfate in the kidney. Kidney Int 2002;61:1760ŌĆō1768.


226. Koppe L, Pillon NJ, Vella RE, et al.
p-Cresyl sulfate promotes insulin resistance associated with CKD. J Am Soc Nephrol 2013;24:88ŌĆō99.



228. Niwa T. Role of indoxyl sulfate in the progression of chronic kidney disease and cardiovascular disease: experimental and clinical effects of oral sorbent AST-120. Ther Apher Dial 2011;15:120ŌĆō124.


231. Watanabe I, Tatebe J, Namba S, Koizumi M, Yamazaki J, Morita T. Activation of aryl hydrocarbon receptor mediates indoxyl sulfate-induced monocyte chemoattractant protein-1 expression in human umbilical vein endothelial cells. Circ J 2013;77:224ŌĆō230.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


