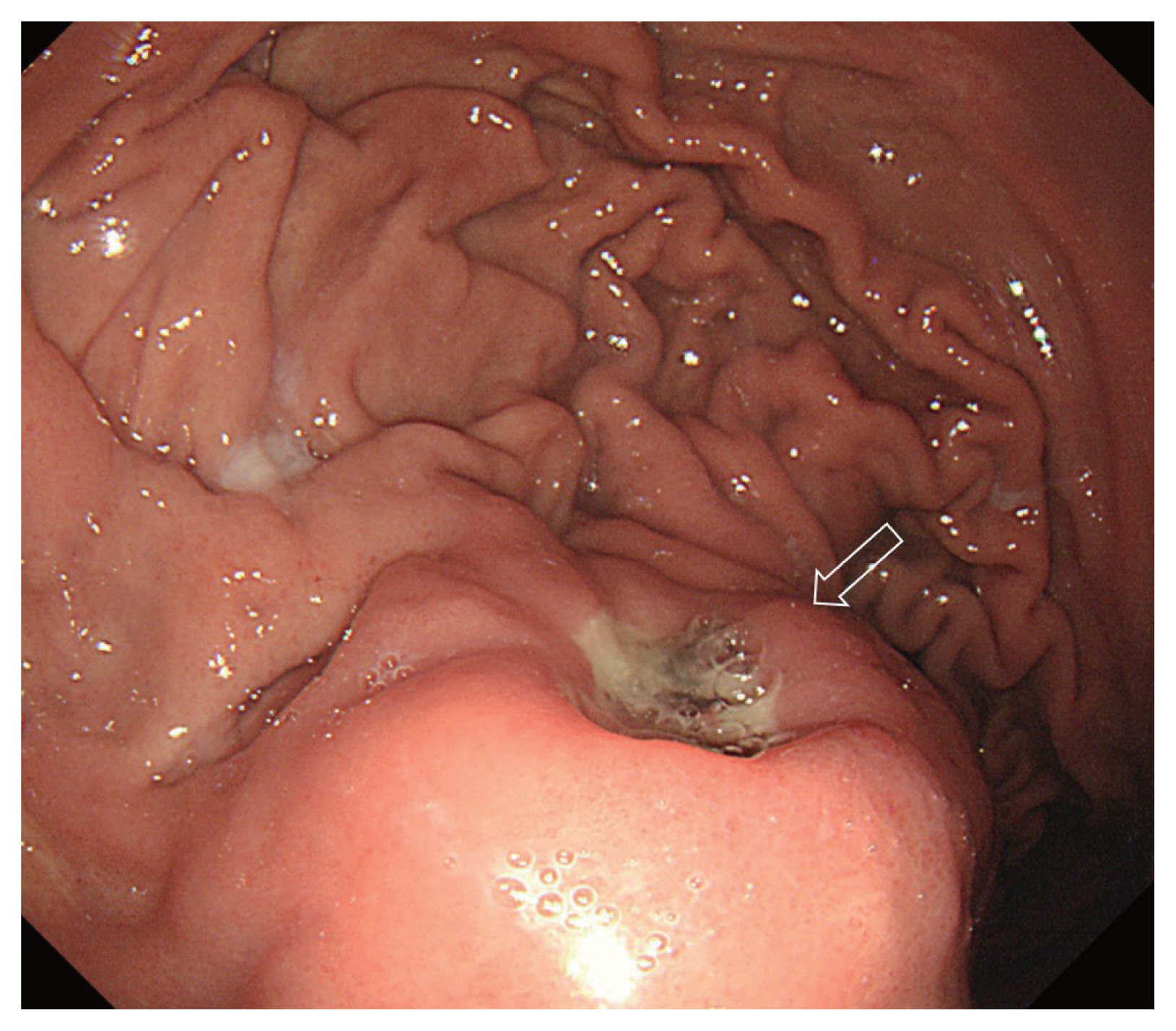
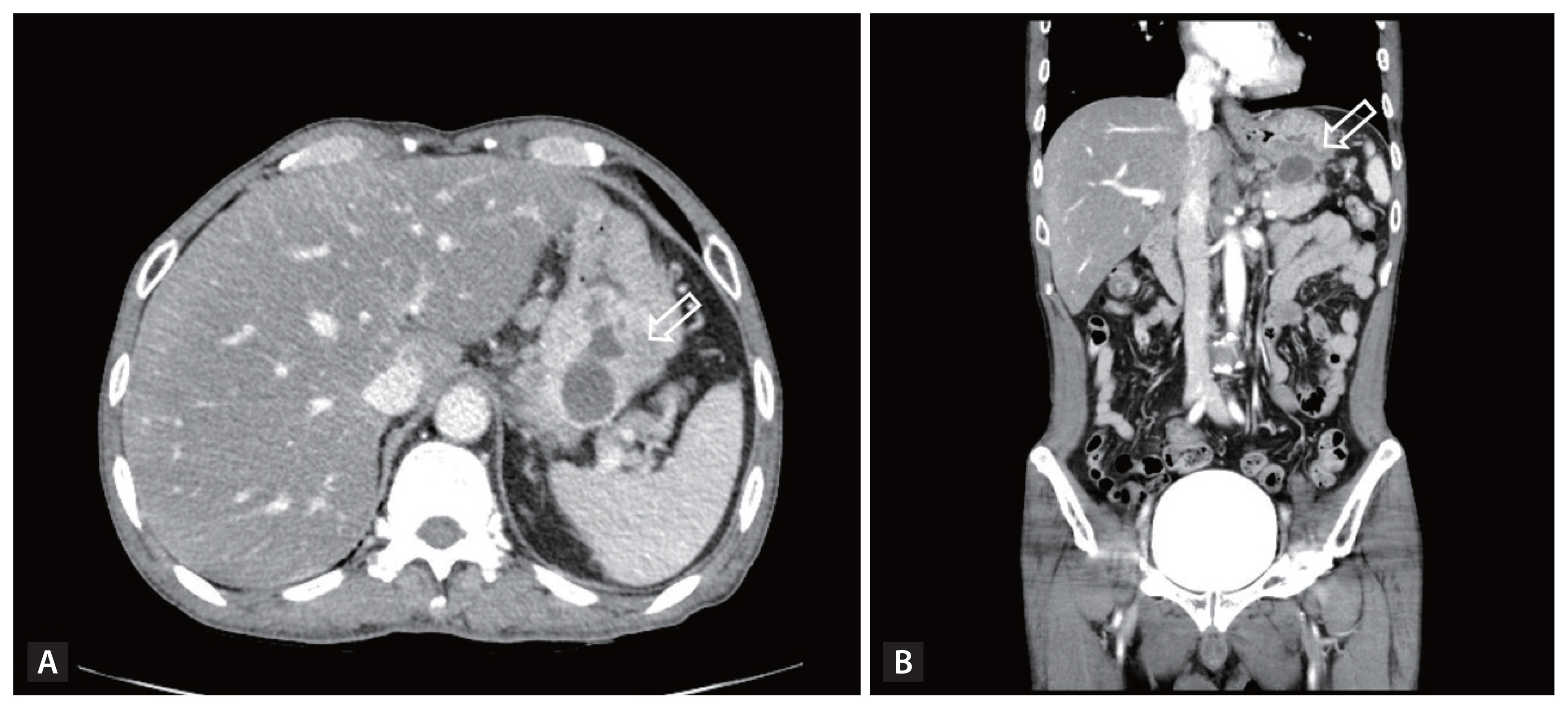
A 59-year-old man was presented to the emergency department due to abdominal discomfort and dizziness for 1 day. He experienced an episode of hematemesis (approximately 50 cc) with nausea. He was diagnosed with solitary pulmonary nodule 2 years ago and had no medication history. The patient had drunken daily one bottle of Soju, Korean distilled spirits for approximately 30 years. Physical examination revealed soft and flat abdomen. There was no tenderness point in the abdomen. His blood pressure was 100/60 mmHg; heart rate, 116 beats per min; body temperature 36.5┬░C; hemoglobin level, 9.8 g/dL; and platelet count, 256 ├Ś 10E3/╬╝L. Prothrombin time and activated partial thromboplastin time were within the normal range. Serum amylase level was 24 U/L and lipase level was 28 U/L. Gastroscopy revealed a 5 cm sized hard subepithelial lesion with active ulcer on the upper body and posterior wall of the stomach. Malignant subepithelial tumor, such as gastrointestinal stromal tumor (GIST) was suspected (Fig. 1). Abdominal computed tomography (CT) revealed a 3.3 cm sized cystic mass with an enhancing wall at the pancreatic tail protruding to the stomach lumen and adjacent gastric wall thickening consistent with infected pancreatic pseudocyst associated with inflammatory gastric wall change (Fig. 2). The result of endoscopic biopsy was active ulcer with ulcer detritus. Explorative laparotomy was performed to drain the abscess cavity. The surgical field showed pancreatic pseudocyst and gastropancreatic fistula. Due to severe adhesion located at the posterior surface of stomach, the operator could not directly approach the posterior wall. Therefore, the operator decided to open the anterior wall of the stomach. The turbid fluid was noted in the cyst. The cyst was drained and irrigated, and the fistula opening was closed through the opened anterior wall of the stomach. Then, the opened gastric wall was closed. Abdominal CT at 6 days postoperatively showed a decreased size of the pseudocyst at the pancreatic tail (Fig. 3). This study was approved by the Institutional Review Board of the Pusan National University Yangsan Hospital (IRB No. 05-2022-187). The need for informed consent was waived by the Institutional Review Board.
Secondary change of the gastric wall due to pancreatic psudocyst can mimic gastric submucosal tumor, like malignant GIST. Therefore, physicians should consider pancreatic diseases, such as pancreatic pseudocysts, when they experience gastric subepithelial lesion located on the body posterior wall of the stomach.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





