INTRODUCTION
Masked hypertension (MH) is not uncommon in the general population [
1], and it is associated with increased cardiovascular risk [
2]. However, treatment strategies for MH are not established, and it is unclear whether the use of antihypertensive drugs is beneficial for MH. To identify patients with MH, out-of-office blood pressure (BP) should be measured [
3,
4]. Although home BP measurements are helpful in the diagnosis of MH, they usually do not include nighttime BP and may lead to the misdiagnosis of masked nocturnal hypertension, especially in cases of isolated nocturnal hypertension (INHT). Therefore, 24-hour ambulatory BP measurements are needed to avoid missing INHT.
INHT, a subtype of MH [
2], is defined as elevated nighttime BP but with normal daytime BP, and it is associated with increased cardiovascular risk [
5]. However, the prevalence of INHT in the general population and its association with MH is unclear. In addition, as INHT is difficult to diagnose with office or home BP measurements, identifying the characteristics of patients with INHT may be important to determine patients who needed 24-hour ambulatory BP measurements.
The purpose of the present study was to evaluate the prevalence and characteristics of patients with INHT in the general population in Korea.
METHODS
The procedure for participant recruitment and the measurement protocols have been described in detail elsewhere [
6,
7]. The original study was designed to evaluate the association between salt intake and BP. Briefly, adults from five cities in Korea were recruited using a representative sample of telephone numbers selected by list-assisted random digit dialing (LARDD) from a frame of all possible telephone numbers within five cities. From these five cities, 1,128 individuals (971 participants who were invited and 157 participants who were relatives or friends of the invited participants) were included, and data from 823 participants who had valid 24-hour ambulatory BP measurements and were not on antihypertensive drug treatment were analyzed. The study protocol and informed consent form were approved by the Institutional Review Board of each participating institution (IRB approval number of Dongguk University Ilsan Hospital: 2011-1 and 2012-5). All participants provided written informed consent.
Office BP was measured from both arms in the sitting position, three times at 1-minute intervals after a 5-minute rest (Watch BP Office, Microlife AG, Widnau, Switzerland) by trained nurses, and three systolic BP (SBP) and diastolic BP (DBP) values were averaged for each arm. Ambulatory BP was measured for 24 hours at 30-minute intervals (Mobil-O-Graph, I.E.M. GmbH, Stolberg, Germany). More than 70% of the attempted measurements, Ōēź 14 measurements during the daytime (00:09 AM to 9:00 PM) and Ōēź 7 measurements at nighttime (00:00 AM to 6:00 AM) were regarded as valid.
Hypertension based on office BP measurement was defined as SBP Ōēź 140 mmHg or DBP Ōēź 90 mmHg in one of the arms. Prehypertension was defined as office SBP 120 to 139 mmHg or office DBP 80 to 89 mmHg, and optimal BP as office SBP < 120 mmHg and office DBP < 80 mmHg [
8]. Hypertension based on ambulatory BP measurement was defined as 24-hour averaged SBP Ōēź 130 mmHg and/or DBP Ōēź 80 mmHg, and/or daytime averaged SBP Ōēź 135 mmHg and/or DBP Ōēź 85 mmHg, and/or nighttime averaged SBP Ōēź 120 mmHg and/or DBP Ōēź 70 mmHg. Definitions of sustained hypertension (SH), white-coat hypertension (WH), MH, isolated daytime hypertension, INHT, day-night normotension, and day-night hypertension are shown in
Table 1.
Fasting blood glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, serum sodium, and potassium levels were measured after at least 8 hours of overnight fasting.
All data are presented as numbers (percentages) or as mean ┬▒ standard deviation. Comparisons of baseline data between groups were performed using the chi-square test (categorical variables) or the analysis of variance (continuous variables). Comparison of the prevalence of isolated nocturnal and day-night hypertension between groups was compared with the chi-square test. To define independent determinants of MH, age, sex, body mass index, diabetes, smoking, low-density-lipoprotein cholesterol, 24-hour SBP and DBP, SBP and DBP dipping, SBP and DBP non-dipper, and INHT were entered in the logistic regression analysis model. Individuals with WH were excluded from the group comparisons because of their small population. p values < 0.05 were considered statistically significant.
RESULTS
The demographic and clinical characteristics of the study population are presented in
Table 2. The prevalence of normotension, WH, MH, and SH was 53.1%, 0.6%, 35.4%, and 10.9%, respectively. The distribution of office BP was 53.6% (n = 441) for optimal BP, 34.9% (n = 287) for prehypertension, and 11.5% (n = 95) for hypertension.
In the study population, the prevalence of INHT was 22.8% with a margin of error of 2.9% points at the 95 percent confidence level, while the prevalence of isolated daytime hypertension was 3.5% with a margin of error of 1.3% points at the same confidence level (
Table 3). The prevalence of nocturnal hypertension was 42.8% with a margin of error of 3.4% points (n = 352), and that of daytime hypertension was 23.5% with a margin of error of 2.9% points (n = 193). Among individuals with nocturnal hypertension, 53.4% (n = 188) had INHT. Individuals with INHT had a higher office, 24-hour, and daytime and nighttime ambulatory SBP and DBP values compared to individuals with day-night normotension (
Table 3).
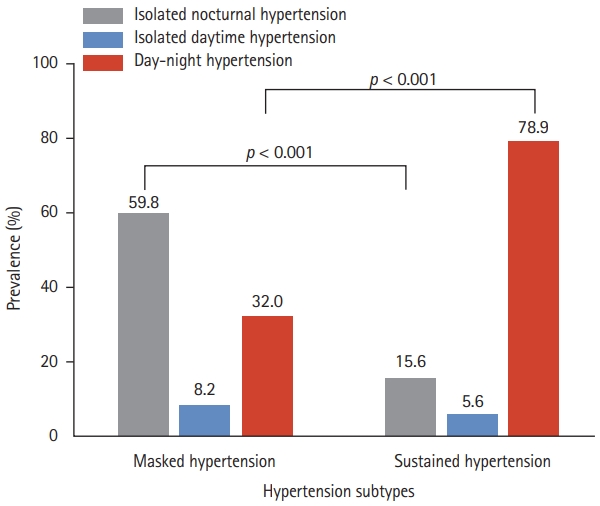
The prevalence of INHT in individuals with MH was higher than that in individuals with SH (59.8% vs. 15.6%,
p < 0.001). However, the prevalence of day-night hypertension was lower in individuals with MH than in those with SH (32.0% vs. 78.9%,
p < 0.001) (
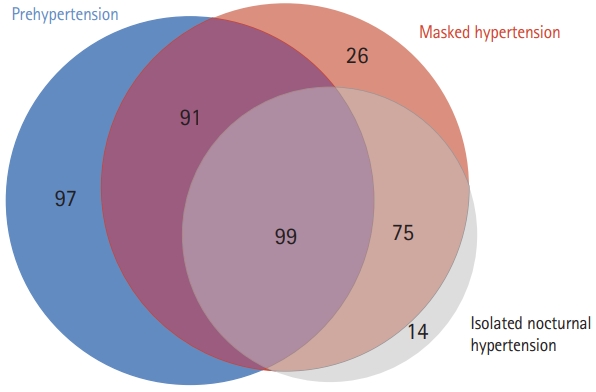
Fig. 1). Among individuals with INHT, 92.6% (174 of 188 subjects) had MH (
Fig. 2). Among the individuals in the prehypertension range of office BP (n = 287), 34.5% of subjects (n = 99) had both INHT and MH, and 66.2% of subjects (n = 190) had MH (
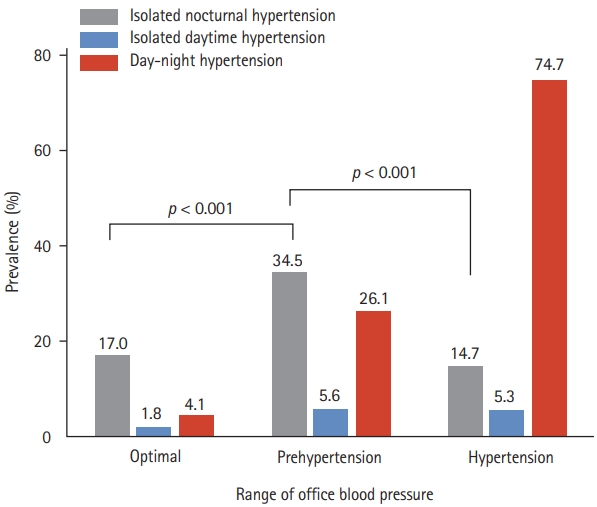
Fig. 2). The prevalence of INHT was highest in individuals with office BP-based prehypertension (
Fig. 3). In individuals with an optimal office BP, 17.0% had INHT (
Fig. 3).
In logistic regression analysis, INHT was an independent determinant of MH (
Table 4) after adjustment for age, sex, body mass index, diabetes, smoking, low-density-lipoprotein cholesterol, 24-hour SBP and DBP, SBP and DBP dipping, and SBP and DBP non-dipper.
In the additional analysis of treated individuals who had valid 24-hour ambulatory BP measurements and were on antihypertensive medication (181 of 1,128 individuals) (
Supplementary Tables 1 and
2), the prevalence of isolated nocturnal uncontrolled hypertension was not different between masked uncontrolled hypertension and sustained uncontrolled hypertension (
Supplementary Fig. 1).
DISCUSSION
The present study revealed a high prevalence of INHT in the general population and individuals with prehypertension and the contribution of INHT to MH. Our study seems crucial because it is the first to be conducted on persons in the Korean general population who were not on antihypertensive medication. An important finding of the present study is that one-third of individuals with office BP-based prehypertension had INHT, and INHT was an independent determinant of MH, emphasizing the important role of 24-hour ambulatory BP measurements in identifying individuals with INHT.
INHT, a subtype of MH, was first described in 2007 by Li et al [
9]. The reported prevalence of INHT ranged from 6% to 13% [
5,
9,
10]. However, the prevalence of INHT in the present study was 22.8%. The difference in prevalence between our study and previous studies can be explained by the ethnic diversity of diurnal BP patterns as suggested by Li et al [
9]. In addition, the different definitions of nighttime and the different characteristics and compositions of our study population compared to previous study populations may have contributed to the different prevalence rates. In our study, we used a fixed time interval (00:00 AM to 6:00 AM) instead of the participantŌĆÖs diary. Li et al. [
9] used a different fixed time interval (10:00 PM to 4:00 AM), and Salazar et al. [
10] used the patientŌĆÖs diary. Salazar et al. [
10] recruited patients who underwent ambulatory BP measurement for the diagnosis or treatment of hypertension. We recruited our study population from the general population via a random method (LARDD) in order to obtain a representative population [
11]. In the Salazar et al. [
10] study, the prevalence of office BP-based hypertension was 44.4%, and that of nocturnal hypertension was 61.5%. In our study, the prevalence of office BP-based hypertension was 11.5%, and that of nocturnal hypertension in untreated individuals was 42.8%. The prevalence of INHT noted in our study may be close to the prevalence in the untreated general population. In the present study, we excluded patients on antihypertensive drug treatment because the use of antihypertensive drugs may affect nighttime BP, although the influence of antihypertensive drug treatment on the prevalence of INHT is uncertain.
There has not yet been much research on INHT. Although the association between INHT and subclinical target organ damage is inconclusive [
12], INHT has been supported to have an increased risk of cardiovascular morbidity and mortality. Analysis of the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) showed a significant association of INHT with all-cause mortality and all cardiovascular events [
5]. In Chinese chronic kidney disease patients, INHT was associated with an increased risk for renal and cardiovascular events compared to nocturnal normotension [
13]. The risk factors and useful marker of INHT are not determined, but older age, blunted sodium metabolism, increased arterial stiffness, and obstructive sleep apnea have been suggested as risk factors [
14]. Among those suggested, blunted sodium metabolism may be a plausible explanation. In our study population, individuals with INHT had significantly higher 24-hour urine sodium-to-potassium ratio compared to individuals with normotension (2.9 ┬▒1.2 vs. 3.3 ┬▒ 3.2, respectively;
p = 0.038 by multivariate analysis controlled with age, gender, body mass index, estimated glomerular filtration rate, and use of diuretics), but 24-hour urine sodium and potassium levels in individuals with INHT were not different from those in individuals with normotension [
15].
In the present study, among individuals with INHT, the majority had normotension based on office BP measurement (i.e., MH). The prevalence of INHT was higher in individuals with prehypertension than in individuals within the optimal and hypertension range of office BP. About one-third of individuals with office BP-based prehypertension had INHT. These findings indicate the need for more active measurement of 24-hour ambulatory BP in this particular population.
MH has a greater association with cardiovascular events than normotension [
16]. In the present study, the prevalence of MH was 35.4%, which is higher than in previous reports [
1,
17,
18]. Among the participants, 66.2% of participants with office BP-based prehypertension had MH, and 65.3% (190/291) of participants with MH had office BP-based prehypertension. The prevalence of MH in our study is different from that in the Masked Hypertension Study [
17] and IDACO [
18]. The difference may be due to different definitions of MH used in the study. The Masked Hypertension Study and IDACO used mean awake ambulatory BP, not 24-hour and nighttime ambulatory BP measurements, and mean awake ambulatory BP may miss individuals with INHT, yielding a lower prevalence of MH. In the present study, the prevalence of MH was 14.2% when daytime ambulatory BP was used as the reference standard for hypertension diagnosis (data not shown), which is similar to the prevalence of 14.4% and 14.0% in the untreated populations of the Masked Hypertension Study [
17] and IDACO [
18], respectively.
The present study emphasizes the importance of active use of 24-hour ambulatory BP measurement, especially for people with prehypertension. Office BP measurement can miss patients with MH. Measurements of out-of-office BP are required to diagnose MH. Therefore, current guidelines recommend the use of out-of-office BP measurements (home and ambulatory BP measurements) for the diagnosis of WH and MH [
3,
4]. Although home BP measurements are commonly used, ambulatory BP measurements are not widely used by general practitioners [
19,
20]. This study highlights the importance of 24-hour ambulatory BP measurements. The high prevalence of INHT in MH indicates that out-of-office BP measurements during the daytime are not enough to diagnose all subtypes of MH. Home BP assessment is unsuitable for measuring nighttime BP unless it is specially designed to measure nocturnal BP [
21]. Therefore, 24-hour ambulatory BP measurements may be more advantageous than home BP measurements. However, 24-hour ambulatory BP measurements may not be applicable to all patients, but they seem necessary for individuals with office BP-based prehypertension considering the high prevalence of INHT and MH in these individuals.
In terms of treatment, there have been no therapeutic trials for individuals with INHT. However, many studies have shown the potential benefits of antihypertensive drug treatment. A meta-analysis showed that antihypertensive drug treatment reduces the risk of stroke, congestive heart failure, composite cardiovascular disease events, and all-cause mortality in individuals with prehypertension and a clinical history of cardiovascular disease [
22]. In the present study, two-thirds of those with office BP-based prehypertension had MH, and two-thirds of those with MH had office BP-based prehypertension. Half of those with INHT had prehypertension based on office BP. This overlap between prehypertension, MH, and INHT shows the potential benefits of antihypertensive drug treatment for individuals with INHT. Therefore, further trials of antihypertensive drug treatment for individuals with INHT are required.
The present study has some limitations. First, the association between INHT and long-term cardiovascular risk could not be evaluated as this study was cross-sectional in nature; and second, this study was only conducted on the Korean population.
In conclusion, this study showed that INHT is not uncommon and it is an independent determinant of MH. The high prevalence of INHT and MH in individuals with prehypertension strongly suggests the use of 24-hour ambulatory BP measurements for individuals within the prehypertension range of office BP.
KEY MESSAGE
1. Isolated nocturnal hypertension is not uncommon.
2. Isolated nocturnal hypertension is an independent determinant of masked hypertension.
3. In a general population, 24-hour ambulatory blood pressure (BP) should be actively measured in individuals within the prehypertension range of office BP.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print





