 |
 |
| Korean J Intern Med > Volume 36(3); 2021 > Article |
|
Abstract
Background/Aims
High-sensitivity cardiac troponin (hs-TnT) assays detect very low levels of cardiac troponin. This study examined the interval change between initial and subsequent hs-TnT levels and evaluated its ability to predict significant coronary stenosis.
Methods
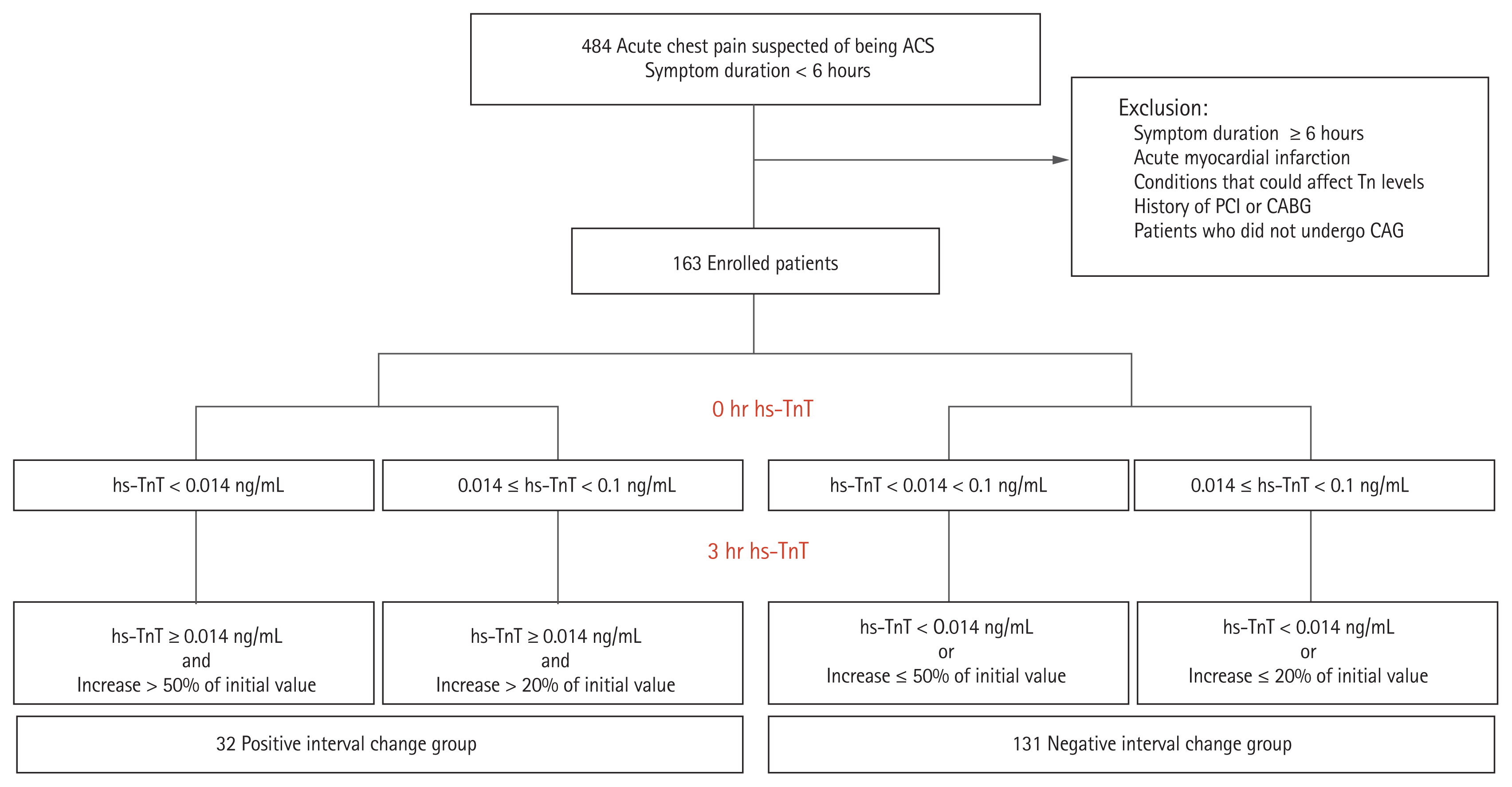
The study analyzed 163 patients who presented with acute coronary syndrome (ACS) and underwent coronary angiography (CAG) between April 2014 and May 2018. The 0 and 3-hour hs-TnT were checked. The patients were subdivided into positive (n = 32) and negative (n = 131) interval change groups. The presence of significant coronary artery stenosis on CAG in the two groups was compared.
Results
The positive interval change group was older and had higher 0 and 3-hour hs-TnT and blood glucose levels than the negative interval change group. Significant coronary stenosis was more common in the positive interval change group than in the negative interval change group (68.8% vs. 23.7%, p = 0.001). However, vasospasm was more common in the negative interval change group (6.3% vs. 31.3%, p = 0.003). The positive interval change group had higher rates of bifurcation lesions and received more percutaneous coronary intervention. In multivariate analysis, age, interval change of serial hs-TnT and diabetes mellitus were independent predictors of significant coronary artery stenosis.
In South Korea, the incidence of acute coronary syndrome (ACS), including acute myocardial infarction (AMI), is increasing gradually and becoming a serious socioeconomic problem [1]. In the emergency setting, an early diagnosis of myocardial infarction (MI) is advantageous for patients and the physicians treating them [2]. Therefore, several rapid diagnosis methods have been devised, and cardiac biomarkers are considered the most important [3ŌĆō7]. Cardiac troponin is the biomarker of choice for diagnosing myocardial necrosis, as it is considered the most sensitive and specific biomarker of myocardial injury [8,9]. High-sensitivity troponin (hs-Tn) has emerged for the assessment of acute chest pain and the improved sensitivity allows the identification of practically any amount of myocardial necrosis [10,11]. The marked evolution of these cardiac biomarker assays has reduced the time interval to the second Tn assessment. If hs-Tn is available, a rapid ŌĆśrule-outŌĆÖ protocol (3-hour hs-Tn) is recommended [12ŌĆō14]. Furthermore, Reichlin et al. [15] introduced a 1-hour ŌĆśrule-outŌĆÖ algorithm as a faster diagnostic tool than the 3-hour ŌĆśrule-outŌĆÖ protocol.
However, no studies have examined a rapid ŌĆśrule-outŌĆÖ algorithm using high-sensitivity troponin T (hs-TnT) in Korean patients with ACS. In addition, there is little information on the prediction of significant coronary artery stenosis using hs-TnT. We hypothesized that if the change in myocardial enzymes is significant, there would be a high likelihood that significant coronary artery stenosis is present in patients with chest pain and suspected non-ST-segment elevation ACS (NSTE-ACS).
From April 2014 to May 2018, 484 patients presented to our tertiary center with acute chest pain suspected of being ACS, which developed within 6 hours. The initial hs-TnT (or 0-hour hs-TnT) was tested routinely. To estimate the interval change in cardiac enzymes, hs-TnT was re-checked 3 hours after presentation and defined as the 3-hour hs-TnT. The study flowchart is shown in Fig. 1. The following patients were excluded from the study: (1) those with duration of chest pain > 6 hours; (2) those with possible ŌĆśrule-inŌĆÖ MI; (3) those with medical conditions that could affect Tn levels (e.g., systemic infection, acute cerebrovascular accident, tachyarrhythmia, renal disease, heart failure, or other acute medical conditions rather than ACS); and (4) those who previously underwent an interventional cardiac procedure. Patients with a 0-hour hs-TnT Ōēź 0.1 ng/mL or who presented with electrocardiogram findings suggesting ST-segment elevation were excluded because they were identified as a ŌĆśrule-inŌĆÖ MI. Patients with a history of coronary artery disease, previous percutaneous coronary intervention (PCI), or previous coronary artery bypass graft were also excluded. The patients who required cardiopulmonary resuscitation during admission, were in cardiogenic shock, or had chronic heart failure were excluded because these conditions may affect the initial Tn levels. Patients who did not undergo coronary angiography (CAG) were excluded. Ultimately, the study enrolled 163 patients. These were subdivided into hs-cTnT positive (n = 32) and negative (n = 131) interval change groups. This study was a prospective, non-randomized, observational study. The study protocol was approved by the Chonnam National University Hospital Institutional Review Board (IRB No. CNUH-2014-124). Informed consent was obtained from all study participants.
Blood samples were collected in serum-separating tubes. Samples were obtained from 484 patients immediately after emergency room visits. The hs-TnT level was measured by Roche e411 (Roche Diagnostics, Rotkreuz, Switzerland). An interval change in serial hs-TnT was defined as follows: (1) 3-hour hs-TnT Ōēź 0.014 ng/mL and more than 50% greater than 0-hour hs-TnT in patients with a 0-hour hs-TnT < 0.014 ng/mL; or (2) 3-hour hs-TnT Ōēź 0.014 ng/mL and more than 20% greater than 0-hour hs-TnT in patients with a 0-hour hs-TnT Ōēź 0.014 ng/mL. The current cutoff value for the hs-TnT assay is 0.014 ng/mL [9]. Although the 2015 European Society of Cardiology (ESC) guidelines recommend invasive management for patients with acute chest pain if 3-hour hs-TnT is greater than 0.014 ng/mL [5], we defined positive or negative interval change groups according to an older guideline that subdivided patients with 3-hour hs-TnT Ōēź 0.014 ng/mL into two groups [16]. The clinical manifestations of NSTE-ACS reference the 2015 ESC guidelines, as follows: (1) prolonged (over 20 minutes) angina at rest; (2) new-onset class II or III angina of the Canadian Cardiovascular Society (CCS) classification; (3) recent destabilization of previously stable angina with at least CCS class III angina (crescendo angina); and (4) post-MI angina. The term non-ST-segment elevation myocardial infarction (NSTEMI) was used when there was evidence of myocardial necrosis (defined as an elevated troponin value with at least one value above the 99th percentile upper reference limit) and the aforementioned clinical features [5]. In this study, hs-TnT was used as a cardiac biomarker to determine whether the subjects had unstable angina or MI. In this study, significant coronary artery stenosis was confirmed by CAG and defined as follows: (1) Ōēź 50% diameter stenosis identified in the left main coronary artery at CAG; or (2) Ōēź 70% diameter stenosis identified in coronary arteries other than the left main coronary artery at CAG. Multi-vessel disease was determined when there were significant coronary stenoses in two or more epicardial coronary arteries. A bifurcation lesion was defined as narrowing of a coronary artery adjacent to or involving the origin of a significant side branch [17]. Vasospasm was defined as a > 90% reduction in diameter on the ergonovine provocation test or a spontaneous, dynamic > 90% decrease in diameter observed during CAG.
The medical and social histories were obtained using a questionnaire. The conventional cardiac risk factors included were hypertension, diabetes, dyslipidemia, stroke, and smoking status. Body data such as height (m) and weight (kg) were measured by experienced nurses and body mass index (BMI, kg/m2) was calculated. Blood was tested in all subjects on admission, including white blood cell count, hemoglobin level, platelet count, serum glucose, serum creatinine, and hs-TnT. The hs-TnT was measured at presentation and 3 hours later. All study subjects underwent echocardiography and CAG. The left ventricular ejection fraction was considered an indicator of ventricular systolic function on transthoracic echocardiography. Patients who had an interval change underwent CAG between admission and hospital discharge, while patients who were negative for an interval change underwent CAG within 1 to 2 months of admission via a hospital visit. The coronary arteries were assessed quantitatively and qualitatively using CAG. If significant coronary artery stenosis was found at CAG, PCI was performed simultaneously.
All statistical analyzes were performed using SPSS for Windows version 25.0 (IBM Co., Armonk, NY, USA). Continuous variables are expressed as the mean ┬▒ standard deviation. Discrete (categorical) variables are expressed as percentages and counts. StudentŌĆÖs t test was used to analyze the difference between two independent groups of continuous variables. In the analysis of categorical variables, the difference between the observed and expected frequencies was confirmed by PearsonŌĆÖs chi-square test. To demonstrate the impact of the interval change in hs-TnT on the presence of significant coronary artery stenosis, the odds ratio (OR) and 95% confidence interval (CI) were calculated using univariable and multivariable logistic regression analysis. The ORs were adjusted according to the variables that had statistical significance (p < 0.05) in the univariable analysis in the multivariable model.
Table 1 compares the baseline clinical characteristics. There was no significant difference between the two groups in age (60.09 ┬▒ 10.40 years vs. 57.79 ┬▒ 11.74 years, p = 0.312), proportion Ōēź 65 years old (34.4% vs. 28.2%, p = 0.495), or proportion of males (71.9% vs. 65.6%, p = 0.502). The positive interval change group had higher 0-hour hs-TnT level (0.020 ┬▒ 0.014 ng/mL vs. 0.011 ┬▒ 0.008 ng/mL, p = 0.001), proportion of 0-hour hs-TnT Ōēź 0.014 ng/mL (56.3% vs. 16.0%, p = 0.001), and 3-hour hs-TnT level (0.150 ┬▒ 0.206 ng/mL vs. 0.010 ┬▒ 0.007 ng/mL, p = 0.050) than the negative interval change group. The laboratory tests did not differ significantly, except for the serum glucose level (151.90 ┬▒ 57.92 ng/mL vs. 115.07 ┬▒ 29.68 mg/dL, p = 0.031). There was no difference in conventional cardiac risk factors such as hypertension, diabetes mellitus, and dyslipidemia in both groups.
Table 2 summarizes the angiographic findings of both groups. There was a marked difference in the presence of significant coronary artery stenosis (68.8% vs. 23.7%, p = 0.001). There was a higher proportion of reduced initial thrombolysis in myocardial infarction (TIMI) flow (i.e., initial TIMI flow 0, I, and II) in the positive interval change group (53.1% vs. 13.7%, p < 0.001). The positive interval change group had a higher rate of bifurcation lesions (12.5% vs. 2.3%, p = 0.028), but a lower proportion of vasospastic components (6.3% vs. 31.3%, p = 0.003). A higher proportion of the positive interval change group underwent PCI (65.6% vs. 22.9%, p < 0.001).
The univariable and multivariable analyses of predictors of significant coronary stenosis are described in Tables 3 and 4, respectively. In the univariable analyses, age, 0-hour hs-TnT, 3-hour hs-TnT, interval change of serial hs-TnT, serum glucose level and history of diabetes mellitus were associated with significant coronary stenosis (Table 3). Multivariable analysis was performed on these significant variables, and age (adjusted OR, 1.054; 95% CI, 1.013 to 1.097; p = 0.024), interval change of serial hs-TnT (adjusted OR, 10.196; 95% CI, 3.571 to 29.111; p = 0.001), and history of diabetes mellitus (adjusted OR, 3.390; 95% CI, 1.216 to 9.451; p = 0.013) were identified as independent predictors of the presence of significant coronary artery stenosis (Table 4).
This study examined the association between significant coronary stenosis and the interval change of serial cardiac biomarkers. A higher proportion of significant stenosis was observed in the positive interval change group. In the positive group, the 0 and 3-hour hs-TnT were higher than in the negative group. As there was a higher rate of significant coronary stenosis in the positive group, the proportion undergoing PCI was also higher in that group. Multivariable analysis of the risk factors for significant coronary stenosis demonstrated that the interval change in serial cardiac biomarkers was the most important predictor of severe artery coronary stenosis angiographically.
The advent of the hs-TnT assay has led to the development of a method for the rapid assessment of ŌĆśrule-outŌĆÖ and ŌĆśrule-inŌĆÖ AMI [9,12,18,19]. Many studies have examined hs-TnT worldwide. Recent guidelines mention the early ŌĆśrule-outŌĆÖ method for AMI. This method is based on the hs-TnT assay and sampling at 0 and 1 hour. This algorithm includes two conditions to rule out MI: (1) hs-Tn is a continuous variable and the probability of MI increases with hs-Tn; and (2) early absolute changes in the level within 1 hour can be interpreted as surrogates of absolute changes over 3 or 6 hours and add incremental diagnostic value to the assessment of cardiac troponin at admission. This ŌĆśrule-outŌĆÖ algorithm should always be integrated with a detailed clinical assessment. It is also mandatory to evaluate the 12-lead electrocardiogram and repeat blood sampling including Tn for all cases of ongoing or recurrent angina.
We hypothesized that cardiac troponin, especially hs-TnT, can predict the presence of angiographic significant coronary stenosis. In many cases of MI, actual significant coronary stenosis may not be present [20ŌĆō23]. CAG is needed to determine whether stenosis exists. All NSTE-ACS cases that have a rise or fall in Tn compatible with MI are classified as high-risk patients, and should undergo CAG within 24 hours, according to the 2015 ESC guidelines [5]. All STEMI cases should undergo primary PCI within 12 hours, according to the 2017 ESC guidelines [24]. Indeed, the greater the likelihood of having significant coronary stenosis is, the greater the need for early revascularization.
A few studies describe the relationship between cardiac biomarkers and significant coronary stenosis. von Jeinsen et al. [25] noted that cardiac troponin-I is useful for diagnosing significant obstructive coronary artery disease in the hemodynamically stable setting of suspected AMI with special electrocardiographic findings, such as bundle branch block or a wide QRS complex. Sanchis et al. [26] measured hs-TnT at the time of presentation and after 6 hours in patients presenting with non-STE acute chest pain and elevated hs-TnT, estimated the maximum hs-cTnT and interval change in hs-TnT, and optimized the cut-off values. They noted that low maximum and low interval changes in hs-TnT were associated with angiographically proven no-stenosis.
In this study, we selected 3-hour hs-TnT as the reference value for a change in cardiac biomarkers. The 2015 ESC guidelines recommend applying the 0/3-hour ŌĆśrule-outŌĆÖ algorithm of NSTE-ACS using the hs-TnT assay [5]. In accordance with prior studies regarding the hs-TnT assay, we set the upper normal limit of 3-hour hs-cTnT as 0.014 ng/mL [9,27]. We included NSTEMI with hs-TnT of at least 0.14 ng/mL and at most 0.1 ng/mL. In such patients, it may be difficult to predict the presence of significant coronary stenosis, so these may be considered ŌĆśgray zoneŌĆÖ patients clinically. In these ŌĆśgray zoneŌĆÖ cases, we found that the interval change in hs-TnT predicts some coronary stenotic lesions before CAG. This supports the evidence for performing CAG. As expected, both 0 and 3-hour hs-TnT were significantly higher in the positive interval change group. Interestingly, the proportion of patients with a significant vasospasm was statistically higher in the negative group. In other words, if ACS is suspected, but the serial changes in cardiac markers are not significant, vasospastic angina may contribute to the clinical situation. Vasospastic angina was diagnosed when spontaneous spasm or ergonovine-induced spasm occurred. If no spontaneous spasm occurred, the ergonovine provocation test was only performed in patients with clinical suspicion of vasospastic angina. However, the prevalence of vasospasm in the negative hs-TnT group was relatively high (6.3% vs. 31.3%, p = 0.003). Therefore, routine vasospasm provocation test can be considered in patients with moderately elevated hs-TnT. The 1-hour ŌĆśrule-inŌĆÖ algorithm was introduced in the 2015 ESC guidelines. However, it was not available in our institution at the time of this study.
Our study had several limitations. First, there is no expert consensus on how to determine the interval change in cardiac biomarkers. Many studies define the interval change as the arithmetic difference between the 0-hour cardiac 0 and subsequent estimated Tn level [12ŌĆō14]. However, we determined the interval change using a slightly different method. Second, the symptom duration might have affected study outcomes. Patients with long symptom duration likely had pre-conditioned myocardium and rich collateral flows in coronary artery circulation, and these aspects might have influenced the study results. Although patients in the current study had symptom durations of less than 6 hours, there was no exact information regarding symptom duration in the case report form. Third, there was some diversity among the underlying clinical characteristics. Fourth, the study was conducted in a single medical center with a small sample size. Therefore, caution is needed when interpreting the results. Finally, this study did not include follow-up information on the clinical prognosis of the subjects. Therefore, large randomized trials should examine the clinical outcomes in both groups.
In conclusion, the change in serial hs-TnT was associated with real angiographic severe stenosis in patients with ACS. A multicenter study with a large number of patient samples is needed.
1. A higher proportion of significant stenosis was observed in the positive interval change group, according to the 3-hour algorithm (68.8% vs. 23.7%).
2. Coronary vasospasm was more common in the negative interval change group (6.3% vs. 31.3%).
3. Serial high-sensitivity troponin T change was associated with real angiographic stenosis in patients with acute coronary syndrome.
Conflict of Interest
Conflict of interest
No potential conflict of interest relevant to this article was reported
Acknowledgments
This study was supported by a grant of the Bio & Medical Technology Development Program of the NRF funded by the Korean government, MSIP (2017M3A9E8023020), and National Research Foundation of Korea (2019R1A2C3003547).
Figure┬Ā1
Study flowchart. ACS, acute coronary syndrome; CABG, coronary artery bypass graft; CAG, coronary angiography; hs-TnT, high-sensitivity troponin T; PCI, percutaneous coronary intervention.
Table┬Ā1
Baseline characteristics
Table┬Ā2
Angiographic and procedural characteristics
Table┬Ā3
Univariable logistic regression analysis for significant coronary stenosis
| Characteristic | Unadjusted OR | 95% CI | p value |
|---|---|---|---|
| Age | 1.052 | 1.019ŌĆō1.086 | 0.002 |
| Male sex | 1.592 | 0.772ŌĆō3.283 | 0.208 |
| BMI Ōēź 25 kg/m2 | 1.260 | 0.628ŌĆō2.525 | 0.515 |
| 0 hr hs-TnT Ōēź 0.014 ng/mL | 3.015 | 1.403ŌĆō6.477 | 0.005 |
| 3 hr hs-TnT Ōēź 0.014 ng/mL | 4.550 | 2.184ŌĆō9.478 | < 0.001 |
| Interval change of serial hs-TnTa | 7.097 | 3.036ŌĆō16.590 | < 0.001 |
| Serum glucose, mg/dL | 1.011 | 1.002ŌĆō1.020 | 0.017 |
| Serum creatinine, mg/dL | 4.697 | 0.709ŌĆō31.116 | 0.109 |
| Hypertension | 1.820 | 0.915ŌĆō3.621 | 0.088 |
| Diabetes mellitus | 4.029 | 1.656ŌĆō9.803 | 0.002 |
| Dyslipidemia | 1.537 | 0.704ŌĆō3.357 | 0.281 |
| Previous history of stroke | 1.041 | 0.092ŌĆō11.758 | 0.974 |
| Current or ex-smoking | 0.987 | 0.499ŌĆō1.955 | 0.971 |
| Left ventricular ejection fraction, % | 0.947 | 0.897ŌĆō1.001 | 0.053 |
Table┬Ā4
Independent predictors of significant coronary stenosis
| Variable | Adjusted OR | 95% CI | p value |
|---|---|---|---|
| Age | 1.054 | 1.013ŌĆō1.097 | 0.024 |
| Interval change of serial hs-TnTa | 10.196 | 3.571ŌĆō29.111 | 0.001 |
| Diabetes mellitus | 3.390 | 1.216ŌĆō9.451 | 0.013 |
REFERENCES
1. Statistics Korea. Deaths and death rates by cause (236 item), sex, and age (by five-year age group) [Internet] Daejeon (KR): Statistics Korea, 2019. [cited 2020 Nov 5]. Available from: http://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board
.
2. Kavsak PA, Worster A. For a rapid diagnosis of acute myocardial infarction, a sensitive troponin assay is needed in the near-patient testing setting. Expert Rev Cardiovasc Ther 2012;10:309ŌĆō312.


3. Zhelev Z, Hyde C, Youngman E, et al. Diagnostic accuracy of single baseline measurement of elecsys troponin T high-sensitive assay for diagnosis of acute myocardial infarction in emergency department: systematic review and meta-analysis. BMJ 2015;350:h15.



4. Rubini Gimenez M, Twerenbold R, Jaeger C, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am J Med 2015;128:861ŌĆō870.


5. Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267ŌĆō315.


6. Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol 2011;58:1332ŌĆō1339.


7. Bandstein N, Ljung R, Johansson M, Holzmann MJ. Undetectable high-sensitivity cardiac troponin T level in the emergency department and risk of myocardial infarction. J Am Coll Cardiol 2014;63:2569ŌĆō2578.


8. Thygesen K, Mair J, Katus H, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010;31:2197ŌĆō2204.


9. Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J 2012;33:2252ŌĆō2257.


10. Sanchis J, Bardaji A, Bosch X, et al. Usefulness of high-sensitivity troponin T for the evaluation of patients with acute chest pain and no or minimal myocardial damage. Am Heart J 2012;164:194ŌĆō200.


11. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551ŌĆō2567.


12. Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 2011;306:2684ŌĆō2693.


13. Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009;361:858ŌĆō867.


14. Biener M, Mueller M, Vafaie M, et al. Comparison of a 3-hour versus a 6-hour sampling-protocol using high-sensitivity cardiac troponin T for rule-out and rule-in of non-STEMI in an unselected emergency department population. Int J Cardiol 2013;167:1134ŌĆō1140.


15. Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012;172:1211ŌĆō1218.


16. Hamm CW, Bassand JP, Agewall S, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999ŌĆō3054.

17. Louvard Y, Thomas M, Dzavik V, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv 2008;71:175ŌĆō183.


18. Reichlin T, Twerenbold R, Reiter M, et al. Introduction of high-sensitivity troponin assays: impact on myocardial infarction incidence and prognosis. Am J Med 2012;125:1205ŌĆō1213.


19. Haaf P, Drexler B, Reichlin T, et al. High-sensitivity cardiac troponin in the distinction of acute myocardial infarction from acute cardiac noncoronary artery disease. Circulation 2012;126:31ŌĆō40.


20. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000;20:1262ŌĆō1275.


21. Mann JM, Davies MJ. Vulnerable plaque: relation of characteristics to degree of stenosis in human coronary arteries. Circulation 1996;94:928ŌĆō931.


22. Frycz-Kurek AM, Gierlotka M, Gasior M, et al. Patients with no significant lesions in coronary arteries and ST-segment elevation myocardial infarction have worse outcome than patients with non-ST-segment elevation myocardial infarction: analysis from PL-ACS Registry. Kardiol Pol 2010;68:1211ŌĆō1217.

23. Aldrovandi A, Cademartiri F, Arduini D, et al. Computed tomography coronary angiography in patients with acute myocardial infarction without significant coronary stenosis. Circulation 2012;126:3000ŌĆō3007.


24. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119ŌĆō177.

25. von Jeinsen B, Tzikas S, Pioro G, et al. Troponin I assay for identification of a significant coronary stenosis in patients with suspected acute myocardial infarction and wide QRS complex. PLoS One 2016;11:e0154724.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



