 |
 |
| Korean J Intern Med > Volume 35(5); 2020 > Article |
|
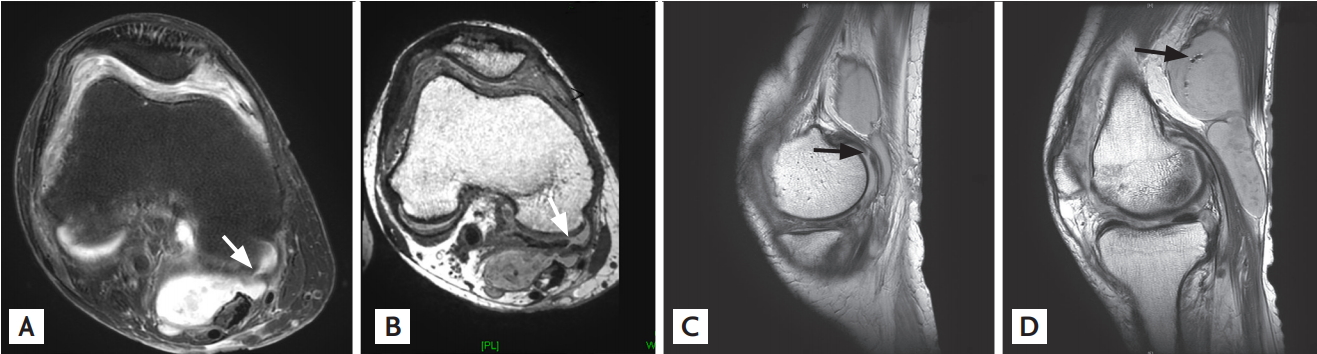
A 77-year-old man with longstanding rheumatoid arthritis was hospitalized because of gastric ulcer bleeding. He was referred to a rheumatologist due to a large BakerŌĆÖs cyst in the right knee joint, which was incidentally found in computed tomography to rule out deep vein thrombosis. Fluid from BakerŌĆÖs cyst showed increased white blood cell count (39,200 cells/╬╝L) with predominant neutrophils (88%). Erythrocyte sedimentation rate (ESR) (> 120 mm/hr) and high sensitivity C-reactive protein (hsCRP; 8.59 mg/dL) levels were significantly elevated. Magnetic resonance imaging (MRI) revealed definite communication between BakerŌĆÖs cyst and knee joint space on T2-weighted fat-suppression axial (Fig. 1A) and T1-weighted magnetization prepared rapid acquisition gradient-echo axial (Fig. 1B) images (white arrow) and on T2-weighted sagittal image (Fig. 1C; black arrow). Air bubbles (black arrow) were noted in the non-dependent area of BakerŌĆÖs cyst on T2-weighted sagittal image (Fig. 1D). Due to combined air content and elevated acute phase reactants, we could not rule out infection of BakerŌĆÖs cyst. After 7 days of intravenous antibiotic treatment, ESR and hsCRP levels did not improve; bacterial culture was negative. After systemic glucocorticoid administration, ESR/hsCRP levels decreased to 72 mm/hr and 0.56 mg/dL, respectively. Treatment decision was difficult since the etiology of co-existing air in BakerŌĆÖs cyst was confusing (infection vs. iatrogenic). After excluding infection, we concluded that the air was from previous intra-articular injection (4 months prior to admission). BakerŌĆÖs cyst is posterior synovial sac of knee joint, and located between the medial head of the gastrocnemius and semimembranosus tendons. Although autopsy and arthroscopic findings demonstrated communication between BakerŌĆÖs cyst and knee joint space, our case showing such communication on MRI is rare. Furthermore, iatrogenic air of BakerŌĆÖs cyst by joint injection has not been reported. These clinical images demonstrate excellent visualization of communication between a BakerŌĆÖs cyst and knee joint space with abnormal air content.
Informed consent was waived by the board.
Figure┬Ā1.
(A) The communication between Baker's cyst and knee joint is visualized (white arrow) in T2-weighted fat-suppression axial view, and (B) T1-weighted magnetization prepared rapid acquisition gradient-echo axial view. (C) The communication is pointed with black arrow in T2-weighted sagittal view. (D) Iatrogenic air bubbles are observed in Baker's cyst (black arrow).
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 3,600 View
- 110 Download
- Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


