 |
 |
| Korean J Intern Med > Volume 28(5); 2013 > Article |
|
Abstract
Background/Aims
Chronic arthritis of familial Mediterranean fever (FMF) involves weight-bearing joints and can occur in patients without a history of acute attack. Our aim was to investigate a possible causal relationship between FMF and osteoarthritis in a population in which FMF is quite common.
Methods
Patients with late stage primary osteoarthritis were enrolled, and five MEFV gene mutations were investigated. The frequency of MEFV gene mutations was compared among patients with osteoarthritis and a previous healthy group from our center.
Results
One hundred patients with primary osteoarthritis and 100 healthy controls were studied. The frequency of MEFV gene mutations was significantly lower in the osteoarthritis group (9% vs. 19%). M694V was the most frequent mutation (5%) in the osteoarthritis group, whereas in the control group, E148Q was the most common (16%). In subgroup analyses, the mutation frequency of patients with hip osteoarthritis was not different from that of patients with knee osteoarthritis and controls (7.1%, 9.7%, and 19%, respectively). There were no differences among the three groups with respect to MEFV gene mutations other than E148Q (8.1% vs. 3.6%). E148Q was significantly lower in the osteoarthritis group than in the controls (16% vs. 1%), although the mutations did not differ between patients with knee osteoarthritis and controls.
Conclusions
In a population with a high prevalence of MEFV gene mutations, we did not find an increased mutation rate in patients with primary osteoarthritis. Furthermore, we found that some mutations were significantly less frequent in patients with osteoarthritis. Although the number of patients studied was insufficient to claim that E148Q gene mutation protects against osteoarthritis, the potential of this gene merits further investigation.
Osteoarthritis (OA) is the most common condition affecting synovial joints and a major cause of disability, especially among the aged population [1]. Several predisposing factors, such as genetic inheritance, bone density, age, ethnicity, nutritional factors, hormonal status, and gender, have been found to be associated with OA. The disease is characterized by focal and progressive hyaline articular cartilage loss with concurrent changes in the adjacent bone, such as marginal overgrowth, osteophytes, and increased thickness of the bony envelope. Although the disease is considered to be representative of degenerative arthritis, an at least low-grade inflammation is thought to accompany the process. This phenomenon was first emphasized by Ehrlich [2] almost 35 years ago. Actually, examination of synovial samples of patients with OA exhibits evidence of inflammation, although it is not as aggressive as that seen in inflammatory arthritis.
The systemic autoinf lammatory disorder familial Mediterranean fever (FMF) is characterized by recurrent episodes of fever and serosal, synovial, or cutaneous inf lammation. Together with intermittent fever and abdominal attacks, articular attacks are one of the most common manifestations of the disease. Although the arthritis in FMF had been thought to recover spontaneously, joint destruction and persistent joint deformities have been reported since the 1960s [3]. Acute arthritis is typical for FMF, but subacute and chronic arthritis can occur in 5% of patients [4]. Unlike acute arthritis, the chronic destructive form usually involves weight-bearing joints such as the hips and knees [5]. Chronic involvement of the hip is usually seen as repeated articular attacks or protracted attacks; however, chronic inflammatory arthritis of the hip joint can occur in patients without a history of attack at the affected joint [6].
FMF is known to be caused by mutations in the MEFV gene, which encodes the pyrin protein. Pyrin belongs to a class of proteins involved in the regulation of apoptosis and inflammation likely through altered leukocyte apoptosis, secretion of interleukin (IL)-1╬▓, and the nuclear factor-╬║B pathway [7,8]. An association between MEFV mutations and inf lammatory diseases was suggested in the early 2000s, and this phenomenon was further supported by observations that MEFV mutations might influence the course and severity of many inf lammatory conditions such as ankylosing spondylitis (AS), rheumatoid arthritis (RA), Behcet disease, ulcerative colitis, and juvenile RA [9-14]. Given the fact that there are patients with FMF with destructive hip involvement but with no symptomatic arthritis and a high prevalence of FMF in Turkey, we hypothesized a causal relationship between FMF at least in a subgroup of patients with OA.
Between January 2008 and June 2009, consecutive patients with late stage primary OA who were candidates for total hip or knee replacement surgery and were seen at the orthopedics outpatient clinic of the University Hospital were included in this study. Patients with secondary causes, namely those known to have inflammatory (RA, AS, etc.) or metabolic joint diseases (hyperparathyroidism, acromegaly, etc.), and patients with an established diagnosis of FMF were excluded. In addition, risk factors for aseptic necrosis, including trauma, corticosteroid use, and alcohol abuse, were screened and excluded. To rule out the possibility of patients who were unaware of their disease, all patients were also questioned regarding the manifestations of FMF, and those who fulfilled the Tel-Hashomer criteria were also excluded. To detect other inflammatory and secondary causes, all patients underwent the following laboratory tests: whole blood count, urinalysis, erythrocyte sedimentation rate, and concentrations of serum glucose, urea and creatinine, calcium, phosphate, magnesium, parathyroid hormone, thyroid stimulating hormone, and C-reactive protein.
All participants were investigated for the presence of MEFV mutations. The frequency of MEFV mutations in patients with OA was compared with that in a historical control group previously studied at our center. The control group comprised 100 unrelated healthy volunteers (48 males and 52 females; age range, 18 to 56 years; mean age, 34.5 ┬▒ 13.8 years) who were free of symptoms, had no family history of FMF or rheumatic heart disease, and were from the same geographic area as the patients.
The study was reviewed and approved by the local ethics committee of Gulhane School of Medicine, and each patient signed an informed consent form before any study-related procedures were performed.
For the OA group, genomic DNA was extracted from whole blood collected in tubes containing ethylenediaminetetraacetic acid. The genomic DNA was isolated using a Nucleospin Blood Kit (Macherey-Nagel, Dueren, Germany). Five common MEFV gene mutations (M694V, M680I, V726A, E148Q, and M694I) were detected by the real-time ARMS-TaqMan method (Dr. Zeydanli FMF type 1 mutation analysis system, Ankara, Turkey). DNA from the patient group (4.5 ┬ĄL) was amplified by real-time polymerase chain reaction (PCR) (iQ5 multicolor real-time PCR detection system, Bio-Rad, Hercules, CA, USA) in a 25-┬ĄL reaction volume containing 20.5-┬ĄL master mix and 0.3-┬ĄL Superhot Taq DNA polymerase (Dr. Zeydanli). PCR conditions were 95Ōäā for 5 minutes followed by 32 cycles of 95Ōäā for 15 seconds and 62Ōäā for 1 minute. The frequency of MEFV gene mutations was compared between patients with OA and a previously studied healthy group from our center. In subgroup analyses, the mutation rates of patients with knee and hip OA were compared.
Statistical analysis was performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). Data are presented as means ┬▒ SD. Comparison of the numerical data of patients with OA and controls was performed with Student t test (for parametric data) or the Mann-Whitney U test (for nonparametric data) for nominal data with the chi-square test. In the comparison of groups, p Ōēż 0.05 was accepted as significant.
We studied 100 patients with primary OA, including 72 with knee OA and 28 with hip OA (male/female, 89/11). The mean age of the patients was 66.0 ┬▒ 7.9 years. The demographic and clinical features of the patients are summarized in Table 1. The historical control group comprised 100 unrelated healthy volunteers (male/female, 48/52). Their mean age was 34.5 ┬▒ 13.8 years (range, 18 to 56).
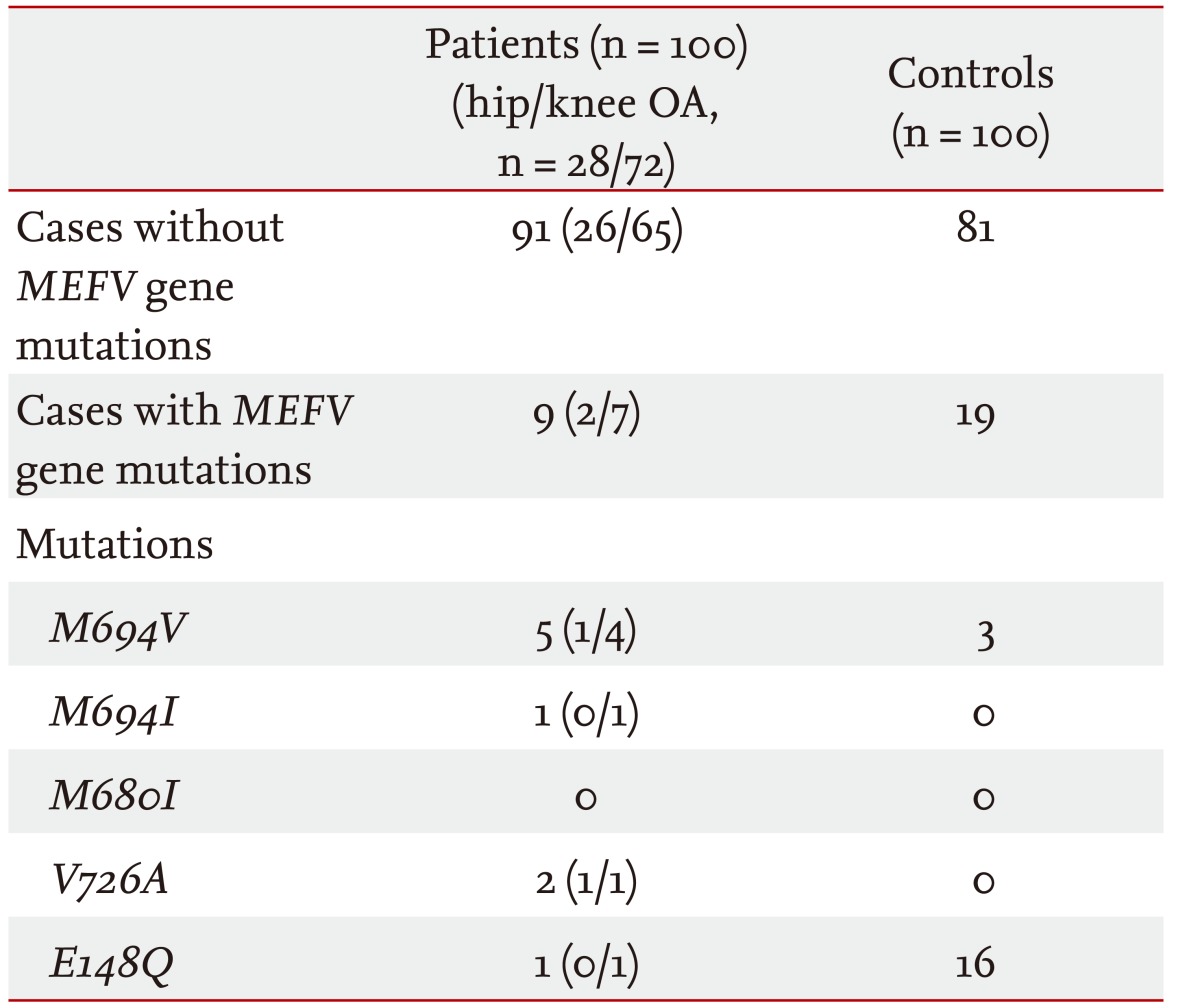
MEFV mutations were identif ied in nine of 200 (4.5%) alleles in nine (9%) of the patients with OA. All nine patients had heterozygote mutations, and none had homozygote mutations. M694V was the most frequent mutation (2.5%) in the patients with OA, and other mutations detected were V726A in two patients (1%), E148Q in one (0.5%), and M694I in one (0.5%). In the historical control group, the frequency of MEFV gene mutation was 9.5%; the most common mutation was E148Q (8%), followed by M694V (1.5%). None of the control patients had the other studied mutations (M694I, M680I, and V726A). The mutated allele frequencies and their distributions in patients with OA and healthy controls are shown in Table 2.
In the study group, the overall allelic frequency of MEFV gene mutations in patients with OA was signif icantly lower than that in the historical control group (9 [4.5%] vs. 19 [9.5%]; p = 0.042). There were no differences among the three groups with respect to MEFV gene mutations other than E148Q (8 [4.0%] vs. 3 [1.8%]; p > 0.05). E148Q was significantly less frequent in patients with OA than in controls (16% vs. 1%; p < 0.001), although there was no difference between patients with knee OA and healthy controls. In the subgroup analyses, the mutation frequency of patients with hip OA did not differ from that of knee OA patients or healthy controls (7.1%, 9.7%, and 19%, respectively; p > 0.05).
Among patients with OA, there were no significant differences between the MEFV mutation carriers and noncarriers with respect to clinical and demographic characteristics such as gender, age at diagnosis, and disease duration (data not shown).
This is the first study to evaluate the relationship between MEFV gene mutations and OA. Our hypothesis was essentially based on the observation that patients with FMF can suffer destructive hip involvement without symptomatic arthritis. Considering that both the prevalence and carrier rate of FMF in Turkey are high, it is possible that MEFV gene mutation is responsible for some cases of OA with hip involvement.
Despite its high prevalence and potential for morbidity, little is known about the pathogenesis of OA. Several studies have shown that OA has a major genetic component that functions in conjunction with environmental factors [15,16]. It has been demonstrated that when compared with the population prevalence, the risk ratio for a relative of a patient with OA ranges from 2 to 8 [17]. However, no studies have reported a significant association between any gene and a specific OA phenotype in Caucasians [18].
Whether MEFV mutations are associated with "subclinical inflammation" has also been studied. Tunca et al. [19] showed that patients who were heterozygous for MEFV mutations had increased levels of inflammatory markers. Furthermore, in their longitudinal follow-up study, Lachmann et al. [20] demonstrated that asymptomatic relatives of patients with FMF and even healthy controls who were heterozygous for a single MEFV mutation had higher levels of acute-phase reactants compared with subjects with no MEFV mutation. Given the inf lammatory aspect of OA and the detrimental effects of MEFV mutations in other inflammatory diseases, a relatively earlier or more severe course can be expected in "carriers." However, when compared with noncarriers, we did not detect such an association with respect to the age at onset or disease severity.
In our study, we found a lower frequency of MEFV gene mutations in patients with primary OA. Furthermore, we found that one of those mutations, E148Q, was significantly lower in patients with OA than in healthy controls. This may have been the result of the high frequency of E148Q mutation in our healthy population; however, the prevalence we relied on was consistent with that in previous studies performed in Turkey that showed almost identical E148Q mutation carriage rates [21]. In contrast, there is an ongoing controversy concerning E148Q, regarding whether it is a true FMF mutation. Its frequency in healthy controls has been found to be relatively high [22,23]. Furthermore, some investigators have used MEFV gene mutations other than E148Q when comparing the carrier rates of these mutations in different diseases [24]. However, we could not satisfactorily explain the lower frequency of this mutation in patients with OA.
Our study had some limitations. The mean age of patients with OA was significantly higher than that of the healthy volunteers. Because OA is an age-related disease, some of the young volunteers may develop OA in the future. This should be taken into consideration and the results should be interpreted with this bias in mind.
In conclusion, in a population with a high prevalence of either FMF or MEFV gene mutations, we did not find an increased rate of these mutations in patients with primary OA. Furthermore, we found that the frequencies of some of these mutations were significantly lower in patients with OA than in healthy controls. Although the number of patients studied is not sufficient to claim that the E148Q gene mutation protects against OA development, the potential of this gene merits further investigation.
1. This is the first study to evaluate the association between development of osteoarthritis (OA) and MEFV gene mutations.
2. We did not detect an increased risk for OA with respect to the presence of mutations in the MEFV gene.
3. The incidence of E148Q mutation was lower in patients with OA, which merits further evaluation.
References
1. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum 1998;41:778ŌĆō799PMID : 9588729.


2. Ehrlich GE. Osteoarthritis beginning with inflammation. Definitions and correlations. JAMA 1975;232:157ŌĆō159PMID : 1172989.


3. Heller H, Gafni J, Michaeli D, et al. The arthritis of familial Mediterranean fever (FMF). Arthritis Rheum 1966;9:1ŌĆō17PMID : 4143706.


4. Garcia-Gonzalez A, Weisman MH. The arthritis of familial Mediterranean fever. Semin Arthritis Rheum 1992;22:139ŌĆō150PMID : 1295087.


5. Sneh E, Pras M, Michaeli D, Shanin N, Gafni J. Protracted arthritis in familial Mediterranean fever. Rheumatol Rehabil 1977;16:102ŌĆō106PMID : 866903.


6. Younes M, Kahn MF, Meyer O. Hip involvement in patients with familial Mediterranean fever: a review of ten cases. Joint Bone Spine 2002;69:560ŌĆō565PMID : 12537263.


7. Bhat A, Naguwa SM, Gershwin ME. Genetics and new treatment modalities for familial Mediterranean fever. Ann N Y Acad Sci 2007;1110:201ŌĆō208PMID : 17911435.


8. Stehlik C, Fiorentino L, Dorfleutner A, et al. The PAAD/PYRIN-family protein ASC is a dual regulator of a conserved step in nuclear factor kappaB activation pathways. J Exp Med 2002;196:1605ŌĆō1615PMID : 12486103.



9. Booth DR, Lachmann HJ, Gillmore JD, Booth SE, Hawkins PN. Prevalence and significance of the familial Mediterranean fever gene mutation encoding pyrin Q148. QJM 2001;94:527ŌĆō531PMID : 11588211.


10. Cosan F, Tozkir JD, Ustek D, Ocal L, Aral O, Gul A. Association of familial Mediterranean fever-related MEFV gene M694V mutation with ankylosing spondylitis. Arthritis Rheum 2006;54:S465ŌĆōS466.
11. Rabinovich E, Livneh A, Langevitz P, et al. Severe disease in patients with rheumatoid arthritis carrying a mutation in the Mediterranean fever gene. Ann Rheum Dis 2005;64:1009ŌĆō1014PMID : 15958759.



12. Rabinovich E, Shinar Y, Leiba M, Ehrenfeld M, Langevitz P, Livneh A. Common FMF alleles may predispose to development of Behcet's disease with increased risk for venous thrombosis. Scand J Rheumatol 2007;36:48ŌĆō52PMID : 17454935.


13. Giaglis S, Mimidis K, Papadopoulos V, et al. Increased frequency of mutations in the gene responsible for familial Mediterranean fever (MEFV) in a cohort of patients with ulcerative colitis: evidence for a potential disease-modifying effect? Dig Dis Sci 2006;51:687ŌĆō692PMID : 16614989.


14. Ozen S, Bakkaloglu A, Yilmaz E, et al. Mutations in the gene for familial Mediterranean fever: do they predispose to inflammation? J Rheumatol 2003;30:2014ŌĆō2018PMID : 12966608.

15. Neame RL, Muir K, Doherty S, Doherty M. Genetic risk of knee osteoarthritis: a sibling study. Ann Rheum Dis 2004;63:1022ŌĆō1027PMID : 15308512.



16. Lanyon P, Muir K, Doherty S, Doherty M. Assessment of a genetic contribution to osteoarthritis of the hip: sibling study. BMJ 2000;321:1179ŌĆō1183PMID : 11073507.



17. Valdes AM, Spector TD. The contribution of genes to osteoarthritis. Med Clin North Am 2009;93:45ŌĆō66PMID : 19059021.


18. Valdes AM, Spector TD. The genetic epidemiology of osteoarthritis. Curr Opin Rheumatol 2010;22:139ŌĆō143PMID : 20090528.


19. Tunca M, Kirkali G, Soyturk M, Akar S, Pepys MB, Hawkins PN. Acute phase response and evolution of familial Mediterranean fever. Lancet 1999;353:1415. PMID : 10227232.

20. Lachmann HJ, Sengul B, Yavuzsen TU, et al. Clinical and subclinical inflammation in patients with familial Mediterranean fever and in heterozygous carriers of MEFV mutations. Rheumatology (Oxford) 2006;45:746ŌĆō750PMID : 16403826.


21. Yilmaz E, Ozen S, Balci B, et al. Mutation frequency of familial Mediterranean fever and evidence for a high carrier rate in the Turkish population. Eur J Hum Genet 2001;9:553ŌĆō555PMID : 11464248.


22. Ben-Chetrit E, Lerer I, Malamud E, Domingo C, Abeliovich D. The E148Q mutation in the MEFV gene: is it a disease-causing mutation or a sequence variant? Hum Mutat 2000;15:385ŌĆō386PMID : 10737995.

-
METRICS

- Related articles
-
Novel
LMNA Gene Mutation in a Patient With Atypical Werner's Syndrome2009 March;24(1)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


