 |
 |
| Korean J Intern Med > Volume 28(4); 2013 > Article |
|
Abstract
Takayasu arteritis (TA) is a chronic vasculitis that affects the aortic arch and its primary branches. Ulcerative colitis (UC) is an inflammatory bowel disease of unknown etiology. Patients diagnosed with both TA and UC have rarely been reported. The pathogenesis of TA and UC is uncertain, but cell-mediated mechanisms play an important role in both diseases, and a genetic factor is thought to have an effect on the coincidence of these two diseases. We herein report a 38-year-old female with TA who had a history of UC with optic neuritis. We believe that this is the first case of the coexistence of TA and UC in Korea.
Takayasu arteritis (TA) is a chronic vasculitis that causes inflammation and stenosis of medium- and large-sized arteries. It involves mainly the aortic arch and its branches. Its incidence is low, estimated to be 1.2 to 2.6 cases per 1,000,000 annually; however, it is more common in Asian populations. Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by diarrhea, rectal bleeding, and abdominal pain. Its incidence varies geographically; the highest is in the northern hemisphere and in Caucasians. In North America, the annual incidence ranges from 2.2 to 14.3 cases per 100,000. Coexistence of TA and UC is reported in Japan occasionally, but this is the first case reported in Korea.
A 38-year-old female was admitted with a 14-day history of dizziness, headache, and neck pain. She had a history of visual disturbance and was diagnosed with optic neuritis 4 years prior to admission. After 3 months, her symptoms fully resolved spontaneously. Five months later, she developed diarrhea, intermittent hematochezia, and iron deficiency anemia. Colonoscopy with biopsy led to the diagnosis of UC. Mesalazine resulted in clinical improvement.
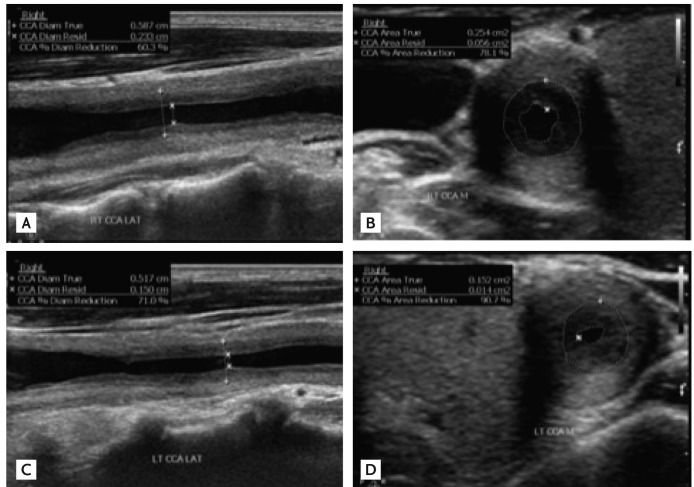
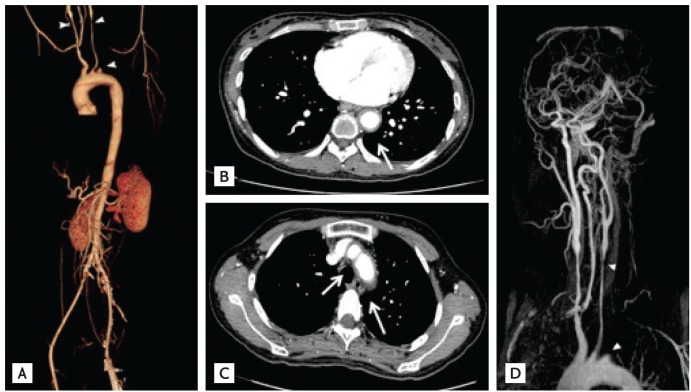
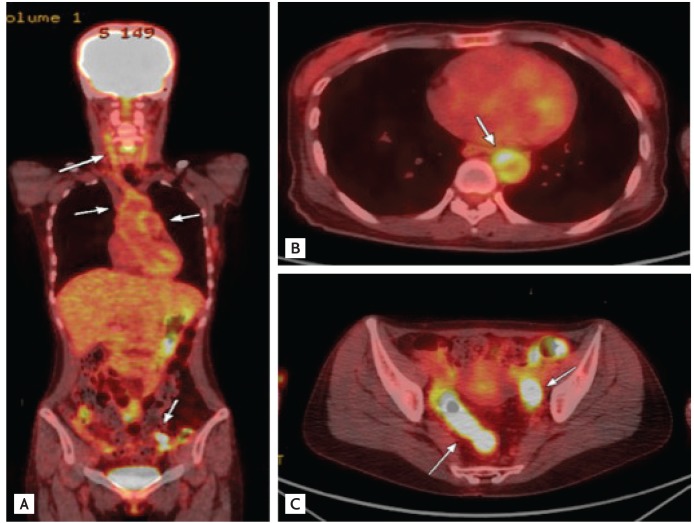
On examination, she showed alert consciousness. Her body temperature was 36.7Ōäā, and her pulse was regular at a rate of 80 per minute. However, her radial and brachial pulses were not detectable on either arm, and bruits were heard over the cervical region on the medial side of the sternocleidomastoid muscle. Her femoral artery, popliteal artery, and dorsalis pedis pulses were easily palpable. Laboratory findings were as follows: white blood cell count, 6,170/mm3; hemoglobin, 8.0 g/dL; and platelet count, 532,000/mm3. Her erythrocyte sedimentation rate (ESR) was 120 mm/hr, and her C-reactive protein (CRP) level was 45.93 mg/L. Other laboratory findings were within normal limits, including liver function, renal function, and urine analysis. Antineutrophil antibodies, anticardiolipin immunoglobulin M (IgM), anticardiolipin IgG, anti-╬▓-2-glycoprotein1 IgG, anti-╬▓-2-glycoprotein1 IgM, and antimyeloperoxidase (anti-MPO) antibodies were all negative; however, antiproteinase-3 antibodies were positive. Chest X-ray showed no cardiomegaly or lung lesions. Ultrasonography of the neck showed severe stenosis of both common carotid arteries and total occlusion of the left subclavian artery (Fig. 1). The left common carotid artery showed 90% luminal narrowing by dimension, whereas the right common carotid artery showed 78% luminal narrowing by dimension. The results of computed tomography scans and brain-neck magnetic resonance imaging showed diffuse wall thickening of the mid-descending thoracic aorta and aortic arch branches, diffuse stenosis of both common carotid arteries and the proximal right subclavian artery, and complete occlusion of the proximal left subclavian artery (Fig. 2). Positron emission tomography scans also showed FDG uptake along the thoracic aorta and arch branches, which was consistent with TA (Fig. 3). An echocardiogram showed GI-II/IV mitral valve regurgitation due to aortic root effacement.
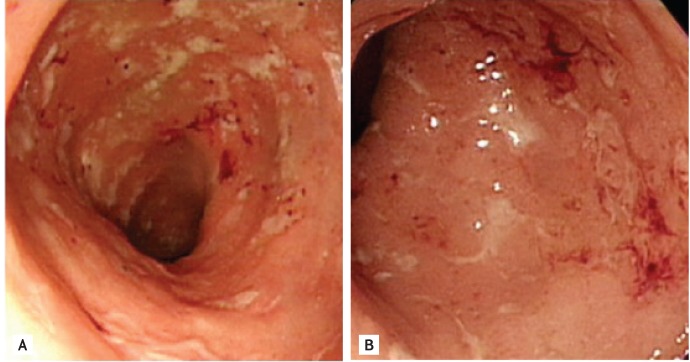
For UC assessment, we performed sigmoidoscopy, which showed erythema, edema, exudates, and spontaneous bleeding of the bowel, which were consistent with UC (Fig. 4).
For treatment, we started high-dose prednisolone (1 mg/kg, 50 mg) and added 50 mg of azathioprine. After this treatment, the patient's dizziness improved, her neck pain subsided from a visual analogue scale score of 7 to 1, and her ESR decreased from 120 to 38 mm/hr. In addition, the bruits in the cervical region became weaker, which implied that the inflammation had improved with the medication.
TA and UC are both chronic inflammatory diseases of uncertain etiology, and both diseases are thought to be mediated by an immune reaction. NK cell and T lymphocyte infiltration is found in the aortic tissue of patients with TA, and levels of various cytokines, such as tumor necrosis factor (TNF)-╬▒, interleukin (IL)-6, and IL-18, are significantly higher in patients with TA than in healthy controls [1]. The production of proinflammatory cytokines, such as IL-1, IL-6, and TNF-╬▒, is increased in patients with UC, indicating that an immune reaction is also associated with the pathogenesis of UC [2]. An extensive literature review revealed that the coexistence of these two diseases was occasionally reported in Japan, but this is the first report of such coexistence in Korea.
Our patient was diagnosed with TA based on age, diminished brachial artery pulses, bruits over the common carotid arteries, and images showing stenosis of both common carotid arteries and the left subclavian artery. UC was diagnosed based on the colonoscopic findings and biopsy results (Fig. 4). Coincidence of TA and UC is rare, but has been reported in Japan occasionally. To date, 39 Japanese patients [3] and three non-Asian patients have been reported to have both diseases [4]. Interestingly, the present report is the first case of a patient with both diseases in Korea, although Koreans and Japanese are both Asians and have similar biological traits.
Patients with TA accompanied by UC have a tendency to be positive for specific types of HLA, such as A24 or B52 [3]. Numano et al. [5] analyzed reports of 12 patients with TA with UC and discovered that 10 were positive for HLA-B52. These data are based on the Japanese population. Unfortunately, we could not conduct genetic testing in our patient. However, it is well known that the presence of HLA-B52 is closely associated with TA in both Korea and Japan [6], so more patients with both TA and UC may exist in Korea. We should keep in mind that patients with TA or UC may have other autoinflammatory diseases.
In this case, the patient was positive for anti-PR3 antibodies (PR3-antineutrophil cytoplasmic autoantibody [ANCA]). Although antiphospholipid antibodies can be detected in patients with TA, no report has suggested the presence of positive PR3-ANCA in patients with TA. In one study conducted in Mexico, none of the 39 patients with TA were ANCA-positive, even during the active phase [7]. The positive PR3-ANCA in our patient may be explained by her UC. PR3-ANCA is not common in patients with UC, but there are reports that PR3-ANCA can be detected in these patients. A study conducted in China reported that five of 58 patients with UC were PR3-ANCA-positive, while MPO-ANCA demonstrated higher positivity [8].
An interesting feature of this case of TA is that the patient had suffered from optic neuritis in addition to UC. Five months before the diagnosis of UC, she had a concentric visual disturbance of left eye and was diagnosed with optic neuritis in the US. Like most other cases of optic neuritis, her symptoms fully recovered spontaneously without recurrence. The cause of optic neuritis in our patient was unclear, but we assumed that it could have been associated with UC. Both UC and optic neuritis are immune-mediated, and specific mechanisms or target antigens of these diseases are not known. One study demonstrated that patients with UC were 75% more likely than community controls to have been diagnosed with optic neuritis, multiple sclerosis, or another demyelinating condition [9]. In addition, a few case reports have shown that optic neuritis is associated with Crohn disease [10]. Our patient's visual loss may have resulted from optic neuritis associated with UC. Our patient was diagnosed with TA, UC, and optic neuritis, which supports the emerging concept that a patient with one immune-mediated condition is likely to have another autoinflammatory disease. Therefore, when we meet a patient with an autoinflammatory disease, we must look at the patient from a systemic viewpoint and keep the possibility of other autoinflammatory diseases in mind.
In conclusion, we reported the first Korean case of a patient with both TA and UC. Because there are few cases in Japan, more might occur in Korea. Therefore, when physicians in Korea see patients with TA, they should consider the possibility of other coexisting autoimmune diseases, such as UC. The significance of this case is that there may be more patients with coexistence of TA and UC in Korea, so we patients with TA should be evaluated more thoroughly.
References
1. Park MC, Lee SW, Park YB, Lee SK. Serum cytokine profiles and their correlations with disease activity in Takayasu's arteritis. Rheumatology (Oxford) 2006;45:545ŌĆō548PMID : 16352633.


3. Horai Y, Miyamura T, Shimada K, et al. A case of Takayasu's arteritis associated with human leukocyte antigen A24 and B52 following resolution of ulcerative colitis and subacute thyroiditis. Intern Med 2011;50:151ŌĆō154PMID : 21245641.


4. Katsinelos P, Tsolkas P, Beltsis A, et al. Takayasu's arteritis and ulcerative colitis in a young non-Asian woman: a rare association. Vasa 2005;34:272ŌĆō274PMID : 16363285.


5. Numano F, Miyata T, Nakajima T. Ulcerative colitis, Takayasu arteritis and HLA. Intern Med 1996;35:521ŌĆō522PMID : 8842753.


6. Yajima M, Numano F, Park YB, Sagar S. Comparative studies of patients with Takayasu arteritis in Japan, Korea and India: comparison of clinical manifestations, angiography and HLA-B antigen. Jpn Circ J 1994;58:9ŌĆō14PMID : 7908064.


7. Garcia-Torres R, Noel LH, Reyes PA, et al. Absence of ANCA in Mexican patients with Takayasu's arteritis. Scand J Rheumatol 1997;26:55ŌĆō57PMID : 9057803.


8. Liu X, Yu T, Zhao M, Tang X, Gu Q, Liu N. The diagnostic significance of antineutrophil cytoplasmic antibodies in ulcerative colitis. Zhonghua Nei Ke Za Zhi 1999;38:451ŌĆō454PMID : 11798679.

Figure┬Ā1
Neck sonography shows significant (A, B) right common carotid artery stenosis (78% reduction by dimension) and (C, D) left common carotid artery stenosis (90.7% reduction by dimension), consistent with Takayasu arteritis.
Figure┬Ā2
(A, B, C) Computed tomography shows diffuse wall thickening of the aorta to the mid-descending thoracic artery and arch branches, diffuse stenosis of both common carotid arteries, and complete occlusion of the left subclavian artery. (D) Brain magnetic resonance image and angiography also show diffuse narrowing of both common carotid arteries and the right proximal subclavian artery and complete occlusion of the left proximal subclavian artery. These are all consistent with Takayasu arteritis.
Figure┬Ā3
(A,B) Positron emission tomography shows increased fluorodeoxyglucose (FDG) uptake along the walls of the thoracic aorta and arch branches and (C) intense FDG uptake in the rectosigmoid colon and distal descending colon due to ulcerative colitis.
Figure┬Ā4
Endoscopic findings of sigmoid colon mucosa showed that the mucosa was erythematous, edematous, and friable. Multiple shallow ulcers and spontaneous bleeding, which are consistent with ulcerative colitis, were seen. (A) Endoscopy was performed 2008, before the diagnosis of Takayasu arteritis (TA). (B) Another endoscopy was performed in 2011 at the time of TA diagnosis.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



