 |
 |
| Korean J Intern Med > Volume 22(1); 2007 > Article |
|
Abstract
Pulmonary arterial hypertension (PAH) secondary to chronic obstructive pulmonary disease (COPD) is incurable and it has an unpredictable survival rate. Two men who suffered from COPD presented with progressive dyspnea and edema, respectively. PAH, as estimated by the peak velocity of tricuspidal regurgitation, and the depressed myocardial performance index (MPI) of the right ventricle (RV) were noted on echocardiography. In addition to the baseline therapy for their depressed ventilatory function, we prescribed tadalafil 10 mg orally every other day for 2 weeks and then we doubled the dosage. They well tolerated the medication without any notable side effects. After 4 weeks of tadalafil treatment, the patients' pulmonary arterial pressure was decreased and the MPI of the RV was improved in both. The exercise capacity, as measured by the respiratory oxygen uptake, also improved from 10.9 mL/kg/min to 13.8 mL/kg/min in one patient.
We report here on 2 patients with PAH secondary to COPD, and they showed notable improvement of their pulmonary hemodynamics and exercise capacity with the administration of tadalafil.
Pulmonary arterial hypertension secondary to chronic obstructive pulmonary disease (COPD) is incurable with an unpredictable survival rate. An oral administration of phosphodiesterase-5 (PED-5) inhibitor, sildenafil, has been regarded as a safe and effective treatment for patients suffering with pulmonary arterial hypertension (PAH)1, 2). However, its effects have been transient in nature due to its short half life1-3). Tadalafil is a new, long-acting PED-5 inhibitor3, 4), and it seems to be effective for lowering the pulmonary vascular resistance3). In this report two patients with pulmonary arterial hypertension secondary to COPD showed notable improvement in their pulmonary hemodynamics and exercise capacity with the administration of tadalafil.
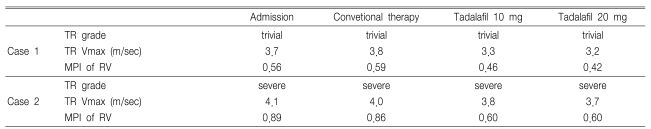
A 55-year-old male, who was diagnosed with emphysema 5 years earlier, had complaints of progressive dyspnea (New York Heart Association Class III) and cough during his regular visits to an outpatient clinic. In addition to the inhalant anticholinergics, he had taken a long acting beta-agonist and theophylline for his depressed ventilatory function (GOLD stage III). Despite a gradual exacerbation of dyspnea and an increase in the amount of sputum, there were no signs of other illnesses, including fever, myalgia or sore throat. His blood pressure was 135/80 mmHg, the pulse was 80 beats/min, the respiratory rate was 20 breaths/min and his temperature was 36.5℃. Electrocardiography showed right ventricular hypertrophy, and the chest X-rays showed no signs of pneumonia. The forced expiratory volume in 1 second (FEV1) was 30% of the predicted value, and this had progressively worsened over the preceding year. Pulmonary arterial hypertension was noted on Doppler echocardiography with trivial tricuspidal regurgitation and a peak velocity (TR Vmax) of 3.6 m/s. The myocardial performance index (MPI) of the right ventricle (RV) was 0.56, which was not changed after 2 weeks of treatment. In addition to the baseline therapy, we administered tadalafil 10 mg orally every other day with the patient's informed consent. He well tolerated a 2 weeks course of this therapy, and he only complained of mild myalgia. Therefore, the tadalafil was increased up to 20 mg/every other day. After 4 weeks of tadalafil treatment, the TR Vmax was decreased to 3.2 m/sec and the MPI of the RV was improved to 0.42 (Table 1). His exercise capacity, as measured by the respiratory oxygen uptake, also improved from 10.9 mL/kg/min to 13.8 mL/kg/min.
A 62-year-old male presented with edema in his legs. He had been suffering from cor pulmonale associated with emphysema for 2 years. The latest data collected from the patient's visit to the clinic showed his ventilatory function being in GOLD stage IV. He was tachypneic (26 breaths/min) and had 3 + pitting edema of the legs. The patient's blood pressure was 120/75 mm Hg and his pulse was 105 beats/min. There were no notable exacerbating factors such as pneumonia, arrhythmia, pulmonary arterial embolism, etc. His arterial blood gas values were a PO2 of 53 mmHg and a PCO2 of 68 mmHg. Echocardiography showed dilated right chambers with severe tricuspidal regurgitation. The estimated TR Vmax was 4.1 m/sec and the MPI of the RV was 0.89. Although the patient's edema substantially improved after therapy with digitalis, diuretics, vasodilator and bronchodilator, the degree of pulmonary arterial hypertension did not change. Therefore, tadalafil therapy was attempted with the patient's written informed consent. We prescribed 10 mg of tadalafil orally every other day for 2 weeks and then we doubled the dosage. During 4 weeks of therapy, he complained of headache and mild orthostatic dizziness. Physical examination showed a blood pressure of 110/70 mmHg and the rest of the examination was unremarkable. Subjective improvement in his functional status was also noted (New York Heart Association Class II). The arterial PO2 was 65 mmHg without inspired oxygen. His TR Vmax was also decreased to 3.7 m/sec and the MPI of the RV was improved to 0.6 (Table 1).
Our attempt of using tadalafil showed promising results for treating pulmonary arterial hypertension secondary to COPD. It was safe and efficacious in improving the functional capacity and pulmonary hemodynamics. These results were consistent with an earlier report; in that report, tadalafil was administered to a patient with end-stage primary pulmonary arterial hypertension5).
Hypoxia-induced pulmonary hypertension complicates the course of COPD. Although continuous oxygen administration is the most reasonable treatment for this condition, and particularly when exercise tolerance is present, it has little effect on the pulmonary artery pressure. A growing number of studies in recent years have demonstrated the promising efficacy of sildenafil for the treatment of pulmonary arterial hypertension1-3). However, one limitation is that it requires frequent daily administrations due to its short half-life of about 4 hours1-3). Tadalafil is a long-acting PDE-5 inhibitor that has an extended half-life of 17.5 hours. It appears to be generally safe and well tolerated by patients, and it has a similar side-effect profile to that of sildenafil3, 4).
In summary, the present report provides a valuable boost for extending the use of tadalafil to the treatment of pulmonary arterial hypertension secondary to COPD, and the results of this treatment should be quite favorable.
References
1. Michelakis ED, Tymchak W, Noga M, Webster L, Wu XC, Lien D, Wang S, Modry D, Archer SL. Long-term treatment with oral sildenafil is safe and improves functional capacity and hemodynamics in patients with pulmonary arterial hypertension. Circulation 2003. 108:2066–2069PMID : 14568893.


2. Ghofrani HA, Wiedemann R, Rose F, Schermuly RT, Olschewski H, Weissmann N, Gunther A, Walmrath D, Seeger W, Grimminger F. Sildenafil for treatment of lung fibrosis and pulmonary hypertension: a randomised controlled trial. Lancet 2002. 360:895–900PMID : 12354470.


3. Ghofrani HA, Voswinckel R, Reichenberger F, Olschewski H, Haredza P, Karadas B, Schermuly RT, Weissmann N, Seeger W, Grimminger F. Differences in hemodynamic and oxygenation responses to three different phosphodiesterase-5 inhibitors in patients with pulmonary arterial hypertension: a randomized prospective study. J Am Coll Cardiol 2004. 44:1488–1496PMID : 15464333.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



