INTRODUCTION
Primary angioplasty is widely used as standard therapy for acute myocardial infarction (AMI), but a significant proportion of these patients does not benefit from this procedure1-3). Diagnostic criteria to identify these patients could lead to the design of more effective therapeutic regimens. Terminal QRS complex distortion on the admission electrocardiogram has been reported to reflect profound myocardial ischemia, larger infarcts and generally worse prognoses compared to those without terminal QRS complex distortion in AMI patients who are given thrombolytic therapy4-8). Patients with terminal QRS complex distortion who have larger infarcts would therefore benefit less from primary angioplasty9, 10). Residual flow to the infarct zone attenuates the severity of myocardial ischemia during AMI11, 12) and may reduce distortion of the terminal portion of the QRS complex. It is not yet known, however, whether terminal QRS complex distortion reflects reduced myocardial perfusion of the infarct area and larger risk to the myocardium prior to primary angioplasty13). We, therefore, have tested the hypothesis that terminal QRS complex distortion on the admission electrocardiogram is related to reduced residual flow to the infarct zone, a larger risk area and greater infarct size in anterior AMI patients undergoing primary angioplasty.
MATERIALS AND METHODS
Study patients
The study population consisted of 46 consecutive patients with anterior AMI who were treated with primary angioplasty at our institution. The inclusion criteria were typically chest pain lasting more than 30 min, presentation within 12 h of the onset of symptoms, and ST-segment elevation ≥ 0.1 mV in ≥ 2 limb leads or ≥ 0.2 mV in ≥ 2 consecutive precordial leads. Patients previously administered thrombolytic agents for index infarction, and those with a prior myocardial infarction or bypass surgery, cardiogenic shock, chronic left bundle branch block, ventricular rhythm or negative T waves in the leads with ST elevation, were excluded from the study. Written informed consent was obtained from each patient, in accordance with the rules of the Institutional Ethics Committee, which approved the study.
Primary angioplasty
Right and left coronary angiograms were obtained in all patients, and primary angioplasty was performed with the goal of ≤30% residual diameter stenosis Stents were deployed using the standard technique. Heparin was administered as an initial bolus of 10,000 U during the procedure, followed by continuous infusion for 3 days. All patients were treated with aspirin, and all patients treated with stents were administered ticlopidine.
Radionuclide studies
Immediately prior to coronary angiography, each patient was intravenously injected with 740 MBq of 99mTc-sestamibi. Imaging acquisition occurred within 6 hours of tracer injection. A follow-up 99mTc-sestamibi study was performed 5~9 days after primary angioplasty. For tomographic imaging studies, we obtained 64 projections of 20 sec each over 180°, using a dual head rotating gamma camera. Images were reconstructed using standard back projection algorithms.
Definitions and analysis
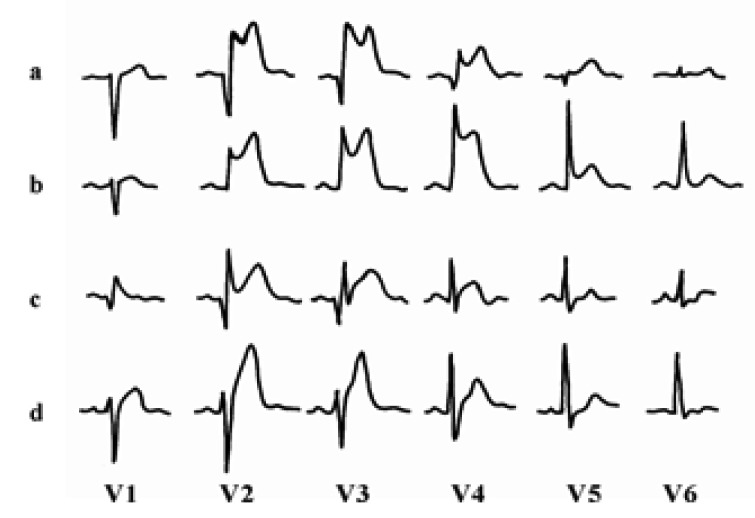
Scintigraphic results were analyzed by an experienced physician (D.H.M.) who was blinded to the clinical data. Short axis slices of the left ventricle were normalized to the peak counts in the heart. Circumferential count profiles were generated for 5 short axis slices from apex to base. Risk area (perfusion defect size on the acute study) and final infarct size (perfusion defect size on the follow-up study) were determined with a threshold of 60% of maximal counts and expressed as a percentage of the left ventricle12, 14). Nadir (residual flow) was estimated from the initial image by the lowest ratio of minimal to maximal counts. The myocardial salvage index was quantified as the change in defect size adjusted for the risk area and calculated as (risk area - final infarct size)/risk area. Distortion of the terminal portion of the QRS complex was defined as the presence of the following in ≥ 2 adjacent leads (Figure 1)4-8) 1) emergence of the J point at ≥ 50% of the R-wave amplitude in leads with initial QR configuration; or 2) absence of S waves in leads without Q waves (Rs configuration).
Statistics
All data are expressed as mean ± SD for continuous variables, and as frequencies for categorical variables. Continuous variables were compared by an unpaired Student's t-test and categoricalvariables by a chi-square test. A probability of p<0.05 was considered to be statistically significant.
RESULTS
The study population was divided into patients with (Group I, n=16) and without (Group II, n=30) terminal QRS complex distortion. We observed few significant differences in baseline characteristics between the two groups (Table 1). However, preinfarct angina, defined as antecedent angina within 24 h prior to the onset of AMI, was present in 4/16 patients (25%) in Group I and 18/30 patients (60%) in Group II (p<0.05). In addition, patients in Group I had significantly higher mean peak levels of serum creatine kinase (4,500±1,430 U/L) than patients in Group II (2,900±1,840 U/L, p<0.01).
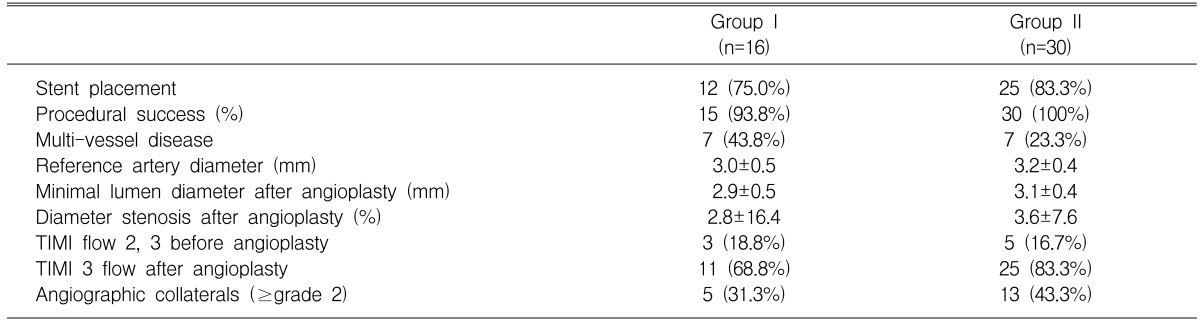
The procedural success rate (≤30% diameter stenosis and final TIMI flow ≥ grade 2) was 93.8% in Group I and 100% in Group II. Angiographic characteristics did not differ significantly between the two groups (Table 2). Final TIMI 3 flow tended to be less common in Group I than in Group II, but this difference did not achieve statistical significance (p=0.253). No patients experienced re-infarction during the study period.
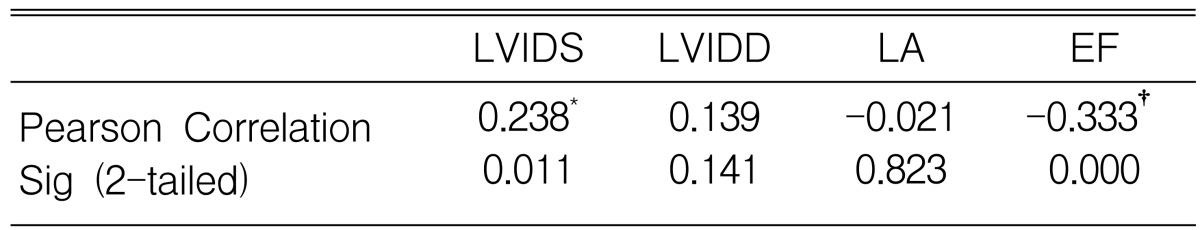
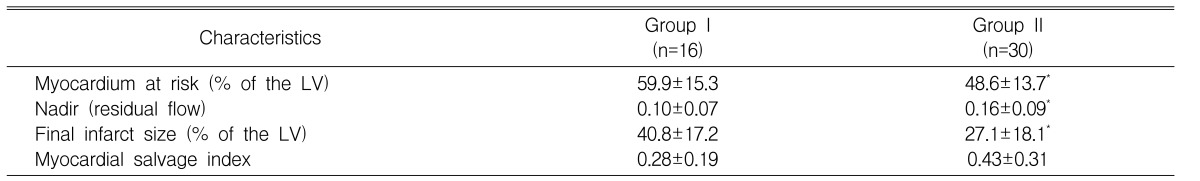
Radionuclide assays showed that the myocardium risk area for patients in Group I (59.9±15.3%) was significantly greater than in Group II (48.6±13.7%, p<0.05), and the nadir measurement of residual flow was significantly lower in Group I (0.10±0.07) than in Group II (0.16±0.09, p<0.05). We also found that the final infarct size was significantly larger in Group I (40.8±17.2%) than in Group II (27.1±18.1%, p<0.05), but the myocardial salvage index did not differ significantly between the two groups (0.28±0.19 for Group I, 0.43±0.31 for Group II, p=0.087)(Table 3).
DISCUSSION
We have shown here that distortion of the terminal portion of the QRS complex on the admission electrocardiogram is associated with reduced residual flow to the infarct zone, a larger risk area and a greater infarct size in patients with anterior AMI treated with primary angioplasty. These findings suggest that residual flow to the infarct area may play a crucial role in preventing terminal QRS complex distortion.
Clinical outcome after AMI is largely determined by infarct size, thus the primary goal of treating patients with AMI should be to reduce infarct size. Final infarct size depends on the duration of ischemia, residual flow to the infarct zone and the size of myocardial area at risk. It is difficult, however, to estimate myocardial risk areas and to predict final infarct size in AMI patients undergoing primary angioplasty. It has been shown that, in AMI patients on thrombolytic therapy, the terminal QRS complex distortion on the admission electrocardiogram is associated with greater mortality rates, larger infarct sizes and greater prevalence of left ventricular dysfunction4-8), thus suggesting that an admission electrocardiogram may provide information about infarct size and clinical outcome in AMI patients undergoing reperfusion therapy. Factors that determine terminal QRS complex distortion in these patients, however, are still poorly understood.
During myocardial ischemia, the terminal QRS complex reflects the activation wave in the local Purkinje fibers, which is less sensitive to ischemia than the contracting myocytes15-17). Thus, profound myocardial ischemia would have to occur to alter the terminal QRS complex sufficiently to affect the Purkinje fibers. Residual flow to the infarct zone, either through collateral vessels or by antegrade flow, has been shown to be a powerful predictor of infarct size11, 12). Therefore, it seems likely that patients with terminal QRS complex distortion have less residual flow to the infarct zone and greater myocardium at risk during AMI. Preinfarction angina seems to limit the size of the infarct resulting from a subsequent coronary occlusion. Interestingly, we found that terminal QRS complex distortion was less common, and final infarct size (26.6±19.7 vs. 38.3±16.5%, p<0.05) was smaller, in patients with preinfarct angina. These results are in agreement with those in previous reports, showing that the presence of preinfarct angina is associated with a better in-hospital outcome, a reduced incidence of heart failure and smaller infarct size in AMI patients treated with reperfusion therapy18, 19).
There are several limitations to this study. First, it represents the experience of a single medical center with a relatively small number of patients, and thus may not be entirely representative of the general population. In addition, this was a selected group of patients, those with hemodynamic stability, because initial 99mTc-sestamibi imaging could be obtained only from these patients.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





