INTRODUCTION
Idiopathic granulomatous mastitis (IGM), which was first described as a clinical entity by Kessler and Wolloch [1] in 1972, is a benign, chronic, and rare breast disease that histologically presents with non-caseated granulomas. It may be confused with breast cancer both clinically and radiologically. Although its etiology has not been explained definitively, various factors including autoimmunity are probably involved [2]. No consensus exists on the best treatment modality for the disease [2-5]. We present an IGM case that was successfully treated with low dose oral and topical steroids and provide information on the use of topical steroids, which has not been reported yet.
CASE REPORT
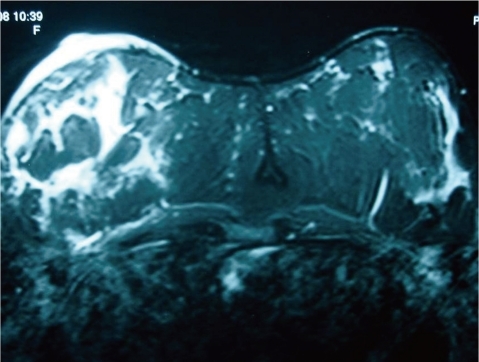
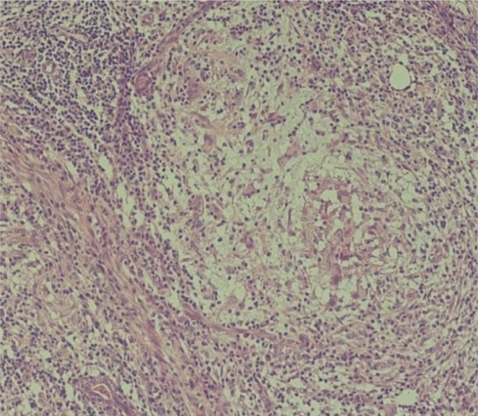
A 32-year-old, married, female patient (para 1) presented with pain, redness, enlargement, and hardening of the right breast (Fig. 1). A physical examination revealed a hyperemic right breast that was larger than the contralateral one. The entire breast was edematous, firm, and painful on palpation. An axillary examination showed no lymphadenopathy. Mammography revealed an asymmetric density increase with indistinct margins in the retroareolar region and upper outer quadrant of the right breast. No microcalcification was evident. Breast ultrasonography showed no distinct loculated fluid; however, all of the mammary tissue was edematous. A breast magnetic resonance image (MRI) revealed thickening of the mammary skin of the right breast alongside nodular lesions in different locations and of various sizes, which exhibited low signal intensity on T1-T2A sequences but displayed no distinct contrast enhancement (Fig. 2). A Tru-cut biopsy was performed, and the histopathological analysis of the material showed giant granulomas without necrosis. No caseating necrosis or vasculitis signs were present (Fig. 3).
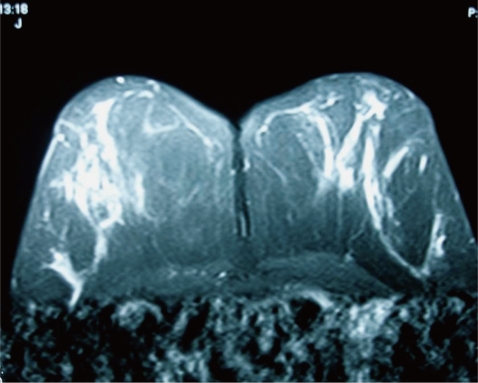
Because of a history of peptic ulcer disease, the oral steroid dose was kept at low levels, and a topical steroid was applied additionally due to the presence of serious cutaneous symptoms. The patient was administered 30 mg/day oral prednisolone and bid topical prednacinolone four times per week (prednol pomade). At the fifth week of treatment, the firmness in the mammary tissue disappeared, the fistulas closed, and the size of the breast was equal to the contralateral one. During the course of the oral and topical steroid therapies, the patient received peptic ulcer treatment (lansoprazole and sucralfate) and antibiotic therapy (ampicillin-sulbactam) against secondary infections that might arise from the skin. Eight weeks after the discontinuing treatment, recurrence was detected in the form of hyperemic areas localized in the mammary skin, and the patient was administered additional topical steroid. The clinical symptoms resolved in 4 weeks after repeated four times per week bid topical steroid therapy. Controls performed during the fifth follow-up month included a breast examination and MRI, both of which showed a normal breast (Fig. 4). The patient demonstrated no recurrence at the 14th month of follow-up.
DISCUSSION
Since its first description in 1972, IGM had challenged clinicians regarding diagnosis, differential diagnosis, and treatment options. It is a difficult disease in terms of diagnosis because the incidence is rare, and the disease may not be recognized by clinicians who have no special training or interest in breast diseases. Because the presenting clinical and radiological signs and symptoms mimic those seen in cancer cases, the disease might be evaluated as breast cancer, and treatment may be planned based on this conclusion.
IGM has no specific radiological appearance, and symptoms often mimic breast cancer. Lee et al. [6] reported a thickening (64%) of mammary skin on mammography. In our case, no calcification or thickening of the mammary skin was observed, but the edema and thickening of the mammary skin were remarkable on MRI.
No consensus exists on the most appropriate treatment modality for IGM. Many treatment options have been presented in the literature, varying from conservative therapy to mastectomy [2-5]. Today, the most commonly applied treatment options are surgical excision and steroid therapy. Systemic corticosteroid therapy was first proposed by DeHertogh et al. [7] who reported successful results. Recently, successful results have been reported with lower doses of steroids. Su et al. [3] reported successful treatment by applying 40 mg/day prednisolone to patients with a history of gestational diabetes, whereas Maffini et al. [8] reported successful outcomes by administering systemic antibiotic therapy and 25 mg/day prednisone. No data are available on the sole or combined use of topical steroids for treating IGM. Topical corticosteroids are used to treat many skin diseases, particularly atopic dermatitis, due to their anti-inf lammator y, vasoconstrictive, antiproliferative, and immunosuppressive effects. While steroids can be easily absorbed through normal skin, their absorption increases during skin inflammation. Because of their local and systemic side effects and the potential to develop tolerance, steroid use at a frequency of more than twice per day is not recommended [9]. Although the duration of topical steroid use should be short, studies have reported the absence of side effects such as skin thinning, atrophy, or hypothalamic-hypophyseal-adrenal axis suppression as a result of 16-24 week long therapies [10]. In our case, topical steroid therapy was applied four days per week bid along with oral steroid treatment. Eight weeks after the end of treatment, only the topical steroid was used at the recurrence. No local or systemic side effects were observed during the use of oral and topical steroids.
In conclusion, we believe that non-invasive treatments should be preferred initially because of the self-limiting nature of IGM, and topical steroid therapy may prove useful, as it affects mammary parenchyma as well as mammary skin. Further studies with a greater number of patients are needed to determine the oral steroid therapy dose and to better understand the efficacy of topical steroids for treating IGM.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





