An unusual cause of a bronchopleural fistula
Article information
A 70-year-old woman was admitted to the hospital with left pleuritic chest pain for 3 days. She complained of a cough, sputum, and chilling sensation but no dyspnea. She had no history of smoking or trauma. Pneumonia with a parapneumonic effusion and endobronchial nodule were evident on the chest computed tomography and flexible bronchoscopy (Fig. 1A, B). Despite receiving intravenous antibiotics and undergoing toilet bronchoscopy, the patient’s fever persisted. A pneumothorax was also detected, which recurred despite a closed thoracostomy (Fig. 1C). To address the obstruction of the left main bronchus, which was causing prolonged obstructive pneumonia and barotrauma, the patient underwent surgery. Thoracoscopically, the left lower lung was totally consolidated and purulent pus with a thickened pleura was noted (Fig. 2A). An endobronchial mass was removed through the bronchus (Fig. 2B). We performed a lobectomy of the left lower lung and the final histological diagnosis was endobronchial lipoma (Fig. 2C, D).

(A) Chest computed tomography (CT) revealed an endobronchial nodule with fat in the left main bronchus (arrow) and parapneumonic effusion on the left side. (B) Bronchoscopy revealed a well-circumscribed, firm, rounded endobronchial nodule in the left main bronchus. (C) Hydropneumothorax was evident on the left in the chest CT scan.
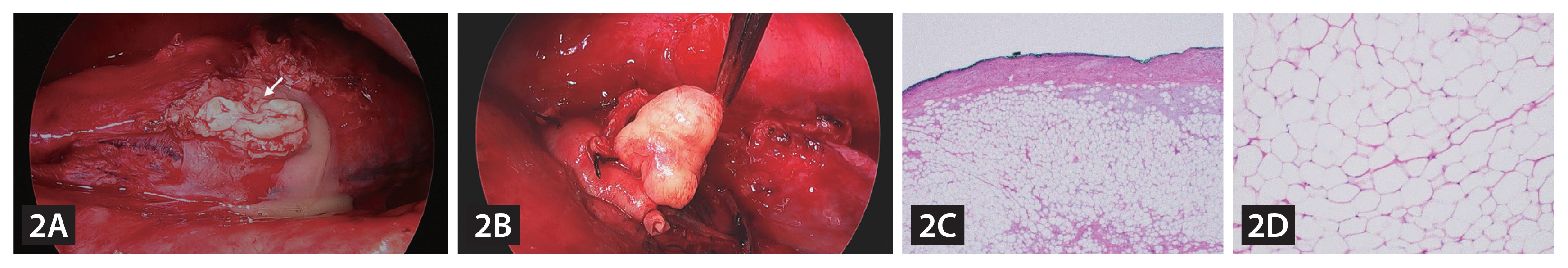
(A) Intraoperatively, an 1.0-cm-long bronchopleural fistula with pus discharge (arrow) was evident in the superior segment of the lower lobe. (B) A homogeneous and narrow-based yellowish mass was deeply embedded into the wall of the left main bronchus. (C) Adipose tissue was observed under the bronchial epithelium (Hematoxylin and Eosin [H&E], ×40). (D) Mature adipose tissue without any cellular atypia was noted (H&E, ×200).
Endobronchial lipomas are extremely rare and benign (0.1–0.5% of all lung tumors). Bronchoscopic intervention can be effective in preserving the lung function. However, despite the lipoma being benign, our patient required a lobectomy due to post-obstructive pneumonia intractable to medical treatment and irreversible lung damage. It is important to tailor the treatment according to the patient’s clinical condition.
Notes
Conflicts of interest
The authors disclose no conflicts.
CRedit authorship contributions
Dongyoon Keum: visualization, writing - original draft, writing - review & editing; Mincheol Chae: writing - review & editing; Ilseon Hwang: formal analysis, visualization, writing - original draft; Hyun Jung Kim: conceptualization, funding acquisition, writing - original draft, writing - review & editing
Funding
This research was supported by the Bisa Research Grant of Keimyung University in 2021.
