Follicular lymphoma: contemporary clinical management with a focus on recent therapeutic advances
Article information
Abstract
Follicular lymphoma (FL) is the most common type of indolent lymphoma, and the prognosis is favorable for most patients. However, FL remains generally incurable, and relapse is common. Patients are at risk of developing treatment-resistant lymphoma, particularly when early disease progression occurs or transformation to aggressive lymphoma takes place. Furthermore, lymphoma is the leading cause of death among patients with FL, emphasizing the need for more effective treatment strategies. This review summarizes therapeutic approaches for FL, with a focus on therapies currently in development. Recent biological insights have driven the emergence of highly effective treatments, including novel immune and targeted therapies. Clinical trials are assessing the efficacy of these novel approaches, which are increasingly used in earlier line settings. In the future, FL therapy is expected to rely less on chemotherapeutic methods, extend remission, and potentially enable cures for a growing number of patients.
INTRODUCTION
Follicular lymphoma (FL) is a common type of B-cell non-Hodgkin lymphoma, with an annual incidence of 2.2 per 100,000 individuals in the United States [1]. The median age at diagnosis is 64 years [1]. The incidence varies according to geography and ethnicity for largely unknown reasons [2], implying that FL incidence is influenced by multiple factors, including population demographics, genetic predis-position, early detection, and potentially lifestyle. FL is an indolent disease with typically slow progression. Although 50–60% of patients present with advanced-stage disease, outcomes are generally favorable; the 5-year survival rate is 90% [1]. Despite high response rates and often durable responses to frontline therapy, relapse is frequent, and FL is considered incurable; lymphoma is the leading cause of death in patients with FL [3]. Early progression after systemic therapy is associated with poor survival and often results from transformation to aggressive lymphoma, which carries an increased risk of mortality [4–8]. This review examines the impacts of recent therapeutic advances on patient care.
PATHOLOGY
Histologically, FL consists of smaller centrocyte-like and larger centroblast-like cells organized in a microanatomical structure, forming follicles that, unlike normal germinal centers, lack polarization into dark and light zones. Malignant cells are also found outside the follicular areas. The relative proportions of these cell types are reflected in grading; grades 1, 2, and 3A represent indolent disease. In contrast, grade 3B is typically associated with poorer outcomes and has been classified as an aggressive form of lymphoma. Since the most recent update of the World Health Organization Classification of Haematolymphoid Tumours [9], grading has become optional, and most FL cases are classified as classic FL. Rarer cases with a predominantly diffuse pattern are classified as diffuse FL; even rarer cases with unusual cytological features are designated FL with unusual cytological features. Grade 3B FL has been renamed follicular large B-cell lymphoma to reflect its distinction from indolent disease. Malignant cells express B-cell-associated antigens, including CD20, CD22, and CD79a; they typically exhibit germinal center markers such as CD10 and BCL6. A translocation between chromosomes 14 and 18 is observed in 85% of cases, leading to aberrant overexpression of the anti-apoptotic factor BCL2 [10]. Although the t(14;18) translocation is a hallmark of FL, it is not a defining feature because it can also occur in other lymphoid malignancies and is absent in a small subset of FL cases, particularly in early-stage cases (~50%) [11]. Certain immunohistochemical markers, such as high expression of Ki-67, IRF4, and FOXP1, are associated with worse outcomes but are not used in clinical practice for treatment decision-making [12,13]. Several FL variants are recognized, including in situ follicular neoplasms, pediatric-type FL, duodenal-type FL, and primary cutaneous follicle center lymphoma [14–17]; these variants are associated with favorable outcomes.
PATHOGENESIS
Advances in genomic methods have substantially improved the overall understanding of the molecular basis of FL, enabling studies of FL at both bulk and single-cell levels [18,19]. Furthermore, the development of sophisticated animal models has illuminated the effects of genetic alterations. FL frequently harbors mutations in genes encoding histone modifiers or chromatin remodelers (e.g., KMT2D, CREBBP, EZH2, ARID1A, EP300) and histone linker genes [20–22]. Epigenetic reprogramming of normal transcriptional profiles is a distinguishing feature of FL and other B-cell malignancies. Other genes, including TNFRSF14, FOXO1, STAT6, IRF8, MEF2B, and genes related to the mTOR pathway (RRAGC, ATP6V1B2, and ATP6AP1), are also mutated in FL [23–25]. The most common gene mutations are not currently actionable, with the exception of mutant EZH2, which can be targeted by small-molecule inhibitors. Patterns of gene mutations may clarify molecular subtypes that influence therapeutic responses and outcomes [26,27]. Similar to other lymphoid malignancies, TP53 mutations have been consistently associated with a worse prognosis, although they have not been adopted as biomarkers [28–30] even though treatment principles, including chemotherapy resistance due to mutant TP53, do not substantially differ from those in other indolent lymphoid malignancies. Clonal heterogeneity exists in FL, which may cause a tissue-based biomarker to yield different results depending on the anatomical site of biopsy [31,32].
Single-cell studies have provided insights into the transcriptional footprints of FL tumor cells, challenging the simplistic view that FL cells are universally germinal center-like [33–36]. The transcriptional profiles in FL are desynchronized, possibly reflecting the loss of polarization in FL nodules [33]. FL transcriptional phenotypes are complex, representing a continuum of gene expression states where some cells express programs similar to normal germinal-center cells and others resemble normal memory B cells [34]. Importantly, memory-like FLs are associated with a higher risk of transformation and shorter progression-free survival (PFS), indicating that molecular-level interpatient heterogeneity translates into distinct clinical trajectories [34,37].
The tumor microenvironment (TME) plays a key role in FL, comprising a significant portion of the tumor mass, and its composition is associated with patient outcomes [38]. The TME consists of interacting immune cells, including CD4+ and CD8+ T cells and macrophages, as well as stromal cells and non-cellular components such as the extracellular matrix. Collectively, these elements support tumor growth and immune evasion [39]. Distinct FL subtypes have been identified based on TME composition, and reduced T-cell counts have been linked to unfavorable outcomes [40,41]. Moreover, the pathogenetic effects of certain gene mutations extend beyond cell-intrinsic changes and contribute to TME remodeling. For example, CREBBP and EZH2 mutations downregulate antigen-presentation genes, such as major histocompatibility complex class I or II [42,43], emphasizing the complexity of interactions between tumor cells and the TME.
RISK PREDICTION
Several clinical factors are associated with an increased likelihood of disease progression after treatment. These factors have been incorporated into clinical-risk assessment tools such as the Follicular Lymphoma International Prognostic Index (FLIPI) [44], FLIPI-2 [45], PRIMA-PI [46], and Follicular Lymphoma Evaluation Index (FLEX) [47]. These prognostic scores, which are calculated using routinely available clinical and laboratory data, enable risk stratification and evaluation of the likelihood of disease progression. However, their discriminative accuracy remains insufficient for risk-adjusted treatment strategies and does not provide insight into potential therapeutic targets in high-risk patients. In addition to clinical indices, functional imaging with positron emission tomography-computed tomography (PET-CT) offers valuable prognostic information. For example, baseline tumor metabolic volume is associated with shorter PFS [48]. Similarly, positive PET-CT findings (i.e., a Deauville score of 4 or 5) upon completion of immunochemotherapy are associated with inferior PFS [49,50]. Efforts have been made to incorporate molecular characteristics into prognostic scores. For example, the m7-FLIPI combines the mutation statuses of seven genes with the FLIPI and performance status [29], whereas the 23-gene predictor assesses risk based on expression levels of 23 genes [51–53]. Additionally, TME-derived signatures show potential for identifying high-risk patients [40,41,54,55]. Notably, the prognostic values of certain biomarkers depend on the treatment received. For instance, EZH2 mutations are favorable prognostic indicators in patients treated with rituximab-cyclophosphamide-vincristine-prednisone (R-CVP) or rituximab-cyclophosphamidedoxorubicin-vincristine-prednisone (R-CHOP) [27,29,56,57]. However, no such association has been detected in patients treated with bendamustine-based immunochemotherapy [53,58]. Despite ongoing efforts to enhance prognostic methods, predictions of early progression and transformation remain challenging [59], posing an obstacle to personalized treatment for at-risk patients.
TREATMENT APPROACH FOR NEWLY DIAGNOSED FL
The fundamental aspects of treatment are determined by disease stage, tumor burden, presence or absence of symptoms, and potential occurrence of laboratory abnormalities (e.g., cytopenias). In addition to clinical examination, cross-sectional imaging is required for staging and is ideally performed with PET-CT [60], which is more sensitive than conventional CT [61,62]. PET-CT can also guide additional biopsies when transformation is clinically suspected. The treatment approach for FL is shown in Figure 1.

Treatment algorithm for follicular lymphoma in the frontline and first- and later-relapse settings. This is intended as a general guide. Interpretations of evidence from published studies may vary among physicians, and treatment choices can be influenced by funding, drug access, and local guidelines. ASCT, autologous stem cell transplantation; chemo, chemotherapy; CHOP, cyclophosphamide, doxorubicin, vincristine, and prednisone; CVP, cyclophosphamide, vincristine, and prednisone; O, obinutuzumab; POD24, progression of disease within 24 months; R, rituximab; R2, rituximab and lenalidomide. Figure created using BioRender.com.
Early-stage disease
Patients with stage I or contiguous stage II disease are typically considered candidates for radiation therapy. This strategy has historically been associated with favorable outcomes; half of the patients with stage I disease do not experience relapse after extended follow-up, raising the question of whether radiation in this context is curative [63–65]. It remains unclear, however, whether these favorable outcomes are due to the intervention or possibly reflect favorable disease biology. Two retrospective series reported no survival advantage of radiation over observation or other systemic treatment modalities [66,67], whereas other studies suggested improved overall survival when radiation is used upfront for early-stage FL [61,68]. Patients with presumed early-stage disease should be fully staged with PET-CT and bone marrow biopsy. Thoroughly staged patients with stage I–II disease receiving ≥ 24 Gy had a 5-year freedom-from-progression rate of 69% (74% for stage I disease vs. 49% for stage II disease) in a multicenter retrospective study by the International Lymphoma Radiation Oncology Group (ILROG) [69]. In-field relapses were uncommon (2%), indicating excellent local disease control. A radiation dose of 24 Gy, divided into 12 fractions, is typically used because it is as effective as higher doses [70]. Doses lower than 24 Gy may result in inferior outcomes. A randomized controlled trial showed a 2-year local progression-free rate of 94% vs. 80% in patients treated with 24 Gy vs. a very low dose of 4 Gy [71]. In a retrospective series, very low-dose radiation achieved an overall response rate (ORR) and complete response (CR) rate of 90% and 66%, respectively [72].
Numerous out-of-field relapses and frequent circulation of the t(14;18) translocation in peripheral blood [73] suggest that systemic disease is often undetected at diagnosis, supporting the rationale for adding systemic therapy to radiation. Rituximab has been proposed as an adjunct treatment based on retrospective and prospective data [74,75]. The strongest evidence supporting systemic therapy comes from the TROG 99.03 trial, in which patients were randomized to receive involved-field radiotherapy with 30–36 Gy, with or without (R)-CVP [76]. Combined therapy significantly improved PFS but not OS. Although efforts to achieve long-term remission after radiotherapy are essential, research concerning minimally toxic strategies that avoid the genotoxicity of chemotherapy is also needed.
Advanced-stage disease, asymptomatic/low tumor burden
The question of whether asymptomatic patients with a low tumor burden and advanced-stage disease require treatment or can be safely observed has been investigated in several clinical trials. Two studies from the pre-rituximab era showed no survival advantage from upfront systemic therapy with oral chlorambucil, prednimustine, or interferon alfa [77,78]. Subsequently, a randomized phase III trial compared rituximab induction, with or without maintenance, to a watch-and-wait approach [79]. As expected, rituximab extended the time before subsequent therapy was needed. At 10 years, 49% and 65% of patients in the rituximab induction and maintenance arms, respectively, had not started a new treatment, compared to 29% in the watch-and-wait arm. Moreover, cause-specific survival exceeded 80% at 10 years, indicating that a low tumor burden is associated with a favorable prognosis. In the RESORT trial, patients received rituximab induction, followed by either maintenance or retreatment as needed [80]. The retreatment strategy, requiring fewer rituximab doses, was preferred, with only a minor difference in the 3-year freedom-from-cytotoxic-therapy rate (84% vs. 95%). Patients assigned to the maintenance arm in the RESORT trial received rituximab every 3 months until treatment failure. A different approach was adopted in the phase III FLIRT trial, where four maintenance doses were administered at 2-month intervals; maintenance was associated with a higher 4-year PFS rate (58% vs. 41%) [81]. New therapies may further improve outcomes for patients with a low tumor burden. However, these patients have a favorable prognosis, and no treatment has yet demonstrated a survival advantage. Therefore, it is essential to minimize treatment toxicity.
Advanced-stage disease with a high tumor burden
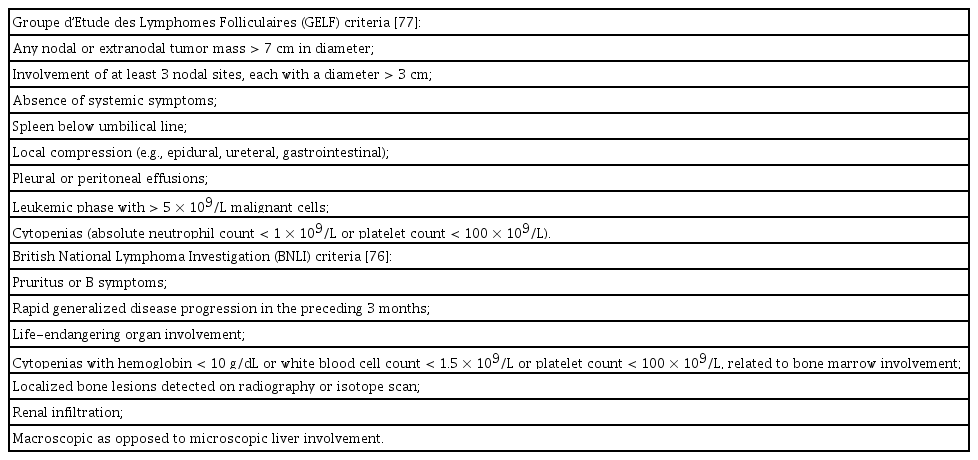
Patients requiring systemic therapy typically meet the criteria of the Groupe d’Etude des Lymphomes Folliculaires (GELF) or the British National Lymphoma Investigation (BNLI), as outlined in Table 1. These criteria are not intended as risk stratification tools; their primary purpose is to aid in identifying patients with a high tumor burden. Clinicians have some discretion in applying these criteria. Since the introduction of rituximab and the discovery that its combination with chemotherapy substantially prolongs both PFS and OS [82–84], immunochemotherapy has become the standard approach for patients with high-tumor-burden FL. Various chemotherapy backbones are available for use. The phase III StiL trial showed that bendamustine and rituximab (BR) achieved better PFS than R-CHOP, with superior tolerability [85]. The confirmatory BRIGHT phase III trial demonstrated the non-inferiority of BR compared to R-CHOP or R-CVP; BR showed higher incidences of vomiting and drug hypersensitivity but lower rates of peripheral neuropathy and alopecia [86]. Longer follow-up from the BRIGHT study revealed superior PFS with BR, but OS did not differ between groups [87]. The PRIMA study showed that rituximab maintenance, administered after R-CHOP, R-CVP, or R-FCM, significantly prolonged PFS [88]. Even with extended follow-up, an OS improvement has not been observed, although rituximab maintenance shows excellent long-term disease control, with a median PFS of 11 years compared to 4 years in the observation arm [89]. Similarly, in the FOLL05 study, the 8-year PFS rate was 48% [90]. Rituximab maintenance after BR induction has not been extensively studied. In a retrospective series of 640 patients, those with a partial response after BR had an improved duration of response when receiving rituximab maintenance, whereas those who achieved complete remission after BR did not [91]. The FOLL12 trial evaluated whether patients with a complete metabolic and minimal residual disease-negative response could forgo rituximab maintenance [92]. Despite an excellent response to induction treatment, the experimental arm showed inferior PFS. In the FOLL12 study, rituximab maintenance resulted in longer PFS in patients treated with R-CHOP and in those treated with BR [93]. To further enhance the efficacy of CD20-directed therapy, the GALLIUM trial randomized patients to receive immunochemotherapy with either rituximab or obinutuzumab. PFS was improved in the obinutuzumab arm [94]. Additionally, obinutuzumab was associated with a lower risk of early progression [95]. A subsequent analysis of the GALLIUM trial highlighted the risk of grade 5 toxicity, particularly in patients treated with bendamustine, due to substantial reductions in CD4+ and CD8+ T-cell counts [96]. The coronavirus disease 2019 pandemic has prompted a re-evaluation of the risk-benefit balance of frontline therapy in FL, with BR associated with increased risks of adverse outcomes [97–99].
Due to the acute and long-term side effects of chemotherapy, there is considerable interest in developing non-chemotherapeutic approaches. After several phase II trials demonstrated promising activity of rituximab combined with lenalidomide (R2) [100–102], the RELEVANCE study compared R2 to R-chemotherapy [103]. At 6 years of follow-up, PFS was nearly identical in the two arms (59% and 60%) [104]. Although neutropenia and febrile neutropenia were more frequent in the R-chemotherapy arm, other side effects, such as cutaneous reactions, were more common in the R2 arm. Obinutuzumab was combined with lenalidomide in the phase II GALEN study, yielding an ORR of 92% and a 2-year PFS rate of 82% [105]. Overall, R2 is a therapeutic option with comparable efficacy but a distinct toxicity profile relative to immunochemotherapy.
TREATMENT APPROACH FOR RELAPSED/ REFRACTORY FL
Because FL is incurable, recurrence is common. However, outside of clinical trials, the utility of regular imaging-based monitoring is limited [106,107]. Considering the unfavorable prognosis regarding POD24, it is tempting to hypothesize that routine imaging can identify early recurrence. However, POD24 detected by incidental routine imaging was not associated with reduced survival [108]. Consequently, most patients should undergo clinical monitoring without systematic, serial imaging. Principles similar to those applied in initial treatment should guide the management of recurrent disease. In relapsed/refractory disease, biopsies are recommended (particularly to exclude transformation) because this scenario requires a different treatment approach and is associated with a worse prognosis [8].
If relapse is limited to a single site or adjacent sites, radiation (even at very low doses) can achieve reasonable disease control [72]. Patients who are asymptomatic and exhibit a low tumor burden can be managed with a watch-and-wait strategy [109]. Conversely, systemic therapy is generally indicated for patients with a high tumor burden or lymphoma-related symptoms. Second- and third-line treatment options differ to some extent because many recently approved novel therapies are based on studies conducted after two or more lines of therapy. With successive lines of treatment, the duration of response tends to diminish [110–112]. As the number of treatment options rapidly increases, it is important to balance potential toxicity, intended therapeutic goals, and patient preferences.
Choice of systemic therapy in the second-line setting
There is no universally accepted treatment approach after recurrence [113–115], and treatment practices vary among jurisdictions [113]. In the second-line setting, re-treatment with chemoimmunotherapy is often considered, particularly if the response to initial therapy was prolonged (e.g., > 5 yr). Typically, a different chemotherapy backbone is chosen to minimize the risk of treatment resistance. In a randomized non-inferiority trial, BR demonstrated superior PFS and OS compared to fludarabine and rituximab in 219 patients, half of whom had FL [116]. In the GADOLIN trial, patients with rituximab-refractory disease were randomized to receive either bendamustine alone or bendamustine combined with obinutuzumab, followed by obinutuzumab maintenance [117]. Patients in the experimental arm experienced improved PFS, and an OS improvement was later demonstrated [117,118]. Notably, the trial did not include rituximab in the control arm, precluding a definitive comparison of obinutuzumab vs. rituximab efficacy in this setting. Because BR is frequently used in the first-line setting, obinutuzumab is often combined with CHOP or CVP for rituximab-refractory FL. However, the optimal sequence of chemotherapy backbones remains unclear. Additionally, the benefit of rituximab maintenance therapy for rituximab-sensitive disease in the second-line setting is uncertain [119], considering that anti-CD20 therapy is routinely administered with upfront treatment.
The immunomodulator lenalidomide induces the recruitment and subsequent degradation of the Ikaros and Aiolos transcription factors via the CRL4CRBN E3 ubiquitin ligase [120–122]. Lenalidomide also enhances NK-cell function, repairs T-cell immunologic synapses, and acts synergistically with rituximab [123–126]. Accordingly, several phase II trials reported encouraging response rates of 65–77% in the relapsed setting [127–129], setting the stage for exploration of this regimen’s efficacy in larger clinical trials. The phase III AUGMENT trial randomized patients with relapsed/refractory FL or marginal zone lymphoma to R2 or rituximab alone [130]. Patients had received a median of one prior therapy and were not rituximab-refractory; the majority (82%) had FL. At the 5-year follow-up, the median PFS was 28 months with R2 vs. 14 months with rituximab alone; an improvement in OS was noted [131]. The R2 regimen showed comparable efficacy in patients with and without POD24 [130]. In the MAGNIFY trial, patients with relapsed/refractory FL, marginal zone lymphoma, or mantle cell lymphoma received induction with R2, followed by randomization to R2 vs. rituximab maintenance. Patients had received a median of two prior lines of therapy. The induction phase showed an ORR of 72% and a CR of 42% in patients with FL, with a median PFS of 41 months [132]. Lenalidomide combined with obinutuzumab was evaluated in the GALEN trial, revealing an ORR of 84% and a 2-year PFS of 65% [133]. Cereblon E3 ligase modulators (CELMoDs) other than lenalidomide are also under investigation. The combination of golcadomide (CC-99282) with rituximab demonstrated encouraging activity in a phase I/II study [134]. Considering these promising results, the combination of lenalidomide with anti-CD20 therapy is a frequently used second-line treatment, especially for patients who did not experience durable responses to immunochemotherapy in the frontline setting.
Roles of autologous and allogeneic stem cell transplantation
Hematopoietic stem cell transplantation (SCT) has long been a commonly used treatment approach in FL. In the pre-rituximab era, long-term follow-up data from the Dana-Farber Cancer Institute showed an 8-year disease-free survival rate of 42% and an OS rate of 66% in patients with relapsed FL who underwent autologous SCT (auto-SCT) [135]. Negative PCR for the t(14;18) rearrangement during follow-up was associated with sustained complete remission. Later follow-up indicated a remission plateau at 48% at 12 years, suggesting the curative potential of chemotherapy intensification and auto-SCT [136]. In a randomized controlled trial of 140 European patients, high-dose chemotherapy was associated with improved PFS and OS [137]. A retrospective re-analysis of the GLSG1996 and GLSG2000 trials showed improved PFS and OS in patients with POD24, suggesting that treatment intensification can overcome the poor prognosis in these patients [138]. In the GELA/GOELAMS FL2000 study, auto-SCT was associated with improved PFS and OS [139]. Encouraging long-term outcomes were reported in a cohort of patients with relapsed FL, 64% of whom had received prior anti-CD20 therapy, with a plateau of 59% in after 9 years [140]. In a retrospective analysis by the LymphoCare Study and the Center for International Blood and Marrow Transplant Research (CIBMTR), auto-SCT was associated with improved OS in patients receiving auto-SCT within 1 year of treatment failure [141]. However, in the follow-up of patients from the PRIMA trial, only those with biopsy-proven transformation benefited from auto-SCT; patients with persistent FL on biopsy did not [8].
Other findings favor allogeneic SCT (allo-SCT). For patients with early treatment failure, matched sibling and matched unrelated donor allo-SCT were associated with better disease control but higher non-relapse mortality relative to auto-SCT [142]. A combined analysis by the European Society for Blood and Marrow Transplantation and CIBMTR reported 5-year OS and PFS rates of 61% and 52%, with worse outcomes in patients who had received multiple lines of therapy and those undergoing myeloablative conditioning [143]. The use of SCT is expected to decrease, particularly where novel treatment options are available. If auto-SCT is considered, the available data suggest it is most effective during the first or second remission, especially for POD24.
Immune therapies
In FL, tumor cells reside within a complex cellular ecosystem, interacting closely with the TME. FL cells depend on signals from the tumor microenvironment and evade immune recognition. Disrupting the interaction between FL cells and the TME is intuitively thought to have therapeutic value. Amplification of programmed death ligands is uncommon in FL tumor cells [144]. The PD-1 checkpoint is expressed in subsets of tumor-infiltrating T cells [145]. CD4+ PD-1high expressing cells are found in the follicles and exhibit a follicular T helper phenotype, whereas PD-1low CD4+ T cells reside outside of follicles, show reduced cytokine production, and transduce fewer signals [146]. Although immune checkpoint inhibitors have significantly impacted multiple cancers, trials of single-agent immune checkpoint inhibitors in FL have yielded disappointing results, with minimal response rates [147–149] (Table 2). However, combining checkpoint inhibitors with anti-CD20-directed therapy has shown promise. For example, in a single-center phase II trial, 30 patients with rituximab-sensitive relapse after one or more lines of treatment received pembrolizumab and rituximab, achieving an ORR of 67%, a CR rate of 50%, and a median PFS of 13 months [150]. In a phase Ib study of 26 patients with FL who had a median of two prior lines of therapy, the combination of atezolizumab and obinutuzumab produced an ORR of 54%, a CR rate of 23%, and a median PFS of 9 months [151]. Triplet therapies have been tested to enhance therapeutic efficacy. In a phase Ib/II trial of patients treated with atezolizumab, obinutuzumab, and lenalidomide, the CR rate was 72%, and the 3-year PFS rate was 68% [152]. The combination of atezolizumab, obinutuzumab, and polatuzumab vedotin was less effective and more toxic [153]. Further studies are warranted to identify the most effective combination strategies and to understand the effects of checkpoint inhibitors when combined with other targeted agents.
The adoptive transfer of autologous T cells engineered to recognize CD19 can result in high response rates and durable responses [154–157]. Three phase II studies have confirmed these promising early results. The ZUMA-5 study evaluated 86 patients with FL who had received two or more prior lines of therapy and were infused with axicabtagene ciloleucel; the ORR and CR rates were 94% and 79%, respectively [158]. The rates of grade 3 or higher cytokine release syndrome (CRS) and neurotoxicity were 6% and 15%. The 3-year follow-up of 127 FL patients from ZUMA-5 showed a median PFS of 40 months [159]. Similar efficacy was observed in the phase II ELARA trial of tisagenlecleucel, where the OR and CR rates were 86% and 69%, respectively, in patients with relapsed/refractory FL after two or more lines of therapy or relapse following auto-SCT [160]. The rates of grade 3 or higher CRS and immune effector cell-associated neurotoxicity syndrome (ICANS) were 0% and 1%, respectively. The most recent update from the ELARA trial showed a 24-month PFS of 57% [161]. The phase II TRANSCEND FL study evaluated lisocabtagene maraleucel in patients with relapsed/refractory FL, 18% of whom had received only one prior line of therapy [162]. Remarkably, in second-line patients, the ORR and CR rates were 96%, with similar results in third- or later-line patients (ORR 97% and CR rate 94%). Grade 3 or higher CRS occurred in 1% of patients, whereas grade 3 or higher neurological toxicity was noted in 2%. Without direct comparative data, it is not possible to conclude that one CAR T-cell product is superior to another. However, the real-world efficacy of CAR T-cell therapy aligns with clinical trial results [163,164], and indirect comparisons suggest that CAR T-cell therapy has greater efficacy than other standard-of-care therapies [165,166].
Another promising advance is the development of CD20 × CD3 bispecific antibodies, which target a B-cell epitope while simultaneously activating T cells near neoplastic cells. In a phase I dose-escalation study, mosunetuzumab achieved OR and CR rates of 66% and 49%, respectively, with a median duration of response of 17 months in patients with relapsed/ refractory indolent lymphomas after two or more prior lines of therapy [167]. The corresponding phase II study reported OR and CR rates of 80% and 60%, respectively [168]. Grade 3 or higher CRS occurred in only two patients (2%), and no grade 3 or 4 neurological toxicity was noted. Extended follow-up confirmed the previous findings, with a high response rate of 88% in eight patients exhibiting indolent lymphomas who relapsed after achieving a CR and were re-treated [169]. A phase I study examined the safety of glofitamab, a bispecific antibody with a 2:1 configuration for bivalent binding to CD20, showing that 4% of patients experienced grade 3 or higher CRS and 1% experienced grade 3 ICANS [170]. Among patients with FL treated with the recommended phase II dose, the OR and CR rates were 62% and 52%, respectively. In a dose-escalation study of subcutaneously administered epcoritamab, the OR and CR rates were 90% and 50% in patients with FL treated at full doses, with no grade 3 or higher CRS events [171]. Similar results were observed in the phase II EPCORE NHL-1 study, where OR and CR rates were 82% and 63%, respectively, with grade 3 CRS in only 2% of patients and no high-grade ICANS [172]. Finally, odronextamab was evaluated in the phase I ELM-1 study, where the OR and CR rates were 78% and 63%, respectively, in patients with relapsed/refractory FL; grade 3 or higher CRS was noted in 7% and grade 3 or higher ICANS was observed in 3% of the overall cohort [173]. The phase II ELM-2 study reported OR and CR rates of 80% and 73%, respectively, in relapsed/refractory FL; only one patient experienced grade 3 CRS and no patients exhibited grade 3 or higher ICANS, after optimized stepup dosing [174]. Across these studies, observed toxicity was generally mild, with frequent pyrexia, mainly during stepup dosing in the first treatment cycle, and cases of neutropenia. However, the risk of infection may be underestimated, as a recent meta-analysis of patients treated with bispecific antibodies showed high frequencies of all-grade (44%), grade 3 or higher (20%), and fatal (3%) infections [175]. Viral infections were overrepresented in fatal cases, indicating a need for preventative measures. Despite these risks, bispecific antibodies are expected to play an increasing role in managing FL, as they achieve high response rates with a comparatively low risk of high-grade toxicity. Bispecific antibodies have not been directly compared with CAR T-cell therapy or other approved therapies, representing an unmet need. A matching-adjusted indirect comparison by the LEO consortium suggested that mosunetuzumab had a higher response rate than real-world data but similar PFS at 12 months [176], with similar results reported by others [177]. The treatment schedules and routes of administration vary among bispecific antibodies, which may influence decision-making in real-world settings.
In addition to immune therapies that rely on T cells for anti-tumor effects, the inhibition of “do-not-eat-me” signals emitted by tumor cells can enhance macrophage phagocytic function and may synergize with rituximab, as demonstrated in a preclinical study [178]. In a phase Ib study of seven patients with relapsed/refractory FL treated with the CD47-blocking antibody Hu5F9-G4 (magrolimab) and rituximab, 71% and 43% of patients achieved an objective and complete response, respectively [179]. In a subsequent extended phase Ib and preliminary phase II report, the OR and CR rates were 66% and 24%, respectively, in patients with indolent lymphomas [180]. Anemia, an on-target toxicity, and infusion reactions were common. TTI-622 (maplirpacept), a fusion protein that blocks the signal-regulatory protein α (SIRPα)–CD47 axis, was evaluated in a phase Ia/Ib dose-escalation and expansion trial involving four patients with FL [181]. Combination therapy studies are underway to better define the role of CD47-directed therapies.
Epigenetic therapies
Epigenetic disruption plays a key role in the development of FL. EZH2 gain-of-function mutations increase trimethylation of lysine 27 on histone 3, suppressing gene expression programs that typically drive terminal differentiation [182]. Accordingly, specific inhibitors of EZH2 have been developed. Proof-of-concept was demonstrated in a phase I study of tazemetostat involving 21 patients with B-cell non-Hodgkin lymphoma, including 7 who had FL [183]. Considering its favorable safety profile, a phase II study was conducted in which tazemetostat was administered orally twice daily [184]. The ORR was 69% in EZH2-mutant cases and 35% in wild-type cases. However, the median PFS was similar between the two cohorts (14 and 11 mo), suggesting that the therapeutic efficacy of EZH2 inhibition is not restricted to EZH2-mutant FL. Intriguingly, an EZH2 gene expression signature is present in certain wild-type cases [185], possibly due to alternative causes of EZH2 hyperactivity, such as chromosomal gains [57]. Importantly, EZH2 mutations are frequently subclonal [31,186], indicating that tissue-based tumor sampling could miss this targetable alteration. The favorable safety profile of tazemetostat supports ongoing efforts to evaluate combination therapies that may yield more durable responses. For instance, the SYMPHONY-1 study is assigning patients to R2 with or without tazemetostat, after a phase Ib lead-in that showed good tolerability and promising responses [187]. In preclinical studies, tazemetostat increased the efficacy of CAR T-cell therapy [188,189]. Other epigenetic therapies, including histone deacetylase inhibitors, have been investigated in FL, with variable response rates and less favorable toxicity profiles relative to other emerging therapies [190–195]. Mutations of the KMT2D histone methyltransferase are among the most common genetic alterations in FL. In a preclinical study, inhibition of the histone demethylase KDM5 reversed the activation of both KMT2D-dependent and independent genes, with efficacy demonstrated in an animal model [196].
Inhibition of B-cell receptor signaling
The preservation of surface immunoglobulin expression and selection against mutations causing structural changes [197] suggest that a functional B-cell receptor is positively selected during FL development. Altered B-cell receptor signaling patterns have been reported in FL [198–200] and may be critical in transmitting tumor-promoting signals from the TME [201,202]. Spleen tyrosine kinase (Syk) docks to the B-cell receptor upon engagement and activates Bruton’s tyrosine kinase (BTK), which then triggers intracellular signaling pathways, such as the phosphatidylinositol 3-kinase (PI3K) pathway [203]. The therapeutic potential of Syk inhibition has been explored in several clinical studies, yielding mixed results. Fostamatinib, the first clinical-grade, orally available Syk inhibitor, showed limited activity in FL (ORR 10%) [204]. Response rates were also low with entospletinib (17% in FL) [205] and the dual Syk/JAK inhibitor cerdulatinib (31%) [206]. In contrast, response rates were higher with the dual Syk/FLT3 inhibitor TAK-659 [207] and sovleplenib (61%) [208].
BTK inhibition, which has led to high response rates in chronic lymphocytic leukemia and mantle cell lymphoma, has also been evaluated in FL. Ibrutinib alone demonstrated a low ORR of 21% in the phase II DAWN study [209]. In a separate phase II study, ibrutinib also showed a modest ORR of 38%; rates were higher in patients with rituximab-sensitive disease than in those with rituximab-refractory disease [210]. The phase III SELENE study randomized patients with relapsed/refractory FL or marginal zone lymphoma after one or more prior therapies to receive immunochemotherapy (BR or R-CHOP) with or without ibrutinib [211]. The experimental group showed a non-significant trend toward improved PFS. Acalabrutinib has been evaluated in combination with rituximab in patients with relapsed/refractory FL and one or more prior lines of therapy, achieving an ORR of 33–39% [212,213]. Acalabrutinib combined with R2 demonstrated an ORR of 76% [213]. In a phase I study, zanubrutinib combined with obinutuzumab achieved an ORR of 72% in relapsed/refractory FL [214]. The phase II ROSEWOOD study randomized patients to receive zanubrutinib with obinutuzumab or obinutuzumab alone [215], revealing improvements in ORR (69% vs. 46%), CR rate (39% vs. 19%), and median PFS (28 vs. 10 mo). Grade 3 or higher toxicities were primarily cytopenias and pneumonia. Therefore, BTK inhibitors combined with other targeted agents may be effective against relapsed/refractory FL. Intriguingly, BTK mutations have been detected in samples from patients with FL who had not been previously exposed to BTK inhibitors; these mutations differ from mutations that confer resistance in chronic lymphocytic leukemia [216,217]. Several BTK mutations identified in FL also induce resistance to BTK inhibition [216]. Therefore, further research is required to develop precision medicine strategies related to BTK inhibition.
PI3K inhibition
PI3K is involved in transducing several signaling pathways, including those from the B-cell receptor, and its inhibition has been evaluated for efficacy in relapsed/refractory indolent lymphomas. In a phase II study, inhibition of the delta isoform (PI3Kδ) with idelalisib led to a response rate of 57% [218]. The ORR was 59% for copanlisib, a pan-class I PI3K inhibitor [219], and 47% (42% in patients with FL) for duvelisib, an oral dual inhibitor of PI3Kδ and γ [220]. In the phase III CHRONOS-3 trial, copanlisib combined with rituximab improved PFS compared to rituximab alone (22 vs. 14 mo). Additional PI3K inhibitors include umbralisib [119], buparlisib [120], KA2237 [121], zandelisib [221], and TQB3525 [222]. Although effective, PI3K inhibitors can cause severe side effects, such as pneumonitis, colitis, transaminitis, and rash. Inhibitors targeting the δ isoform, as well as the ubiquitously expressed α isoform, are associated with hyperglycemia and hypertension [223]. Due to increased toxicity and fatalities in several phase III trials, the development of PI3K inhibitors has largely ceased, and previously approved agents have been withdrawn from the market [224]. The future of this therapeutic class remains uncertain.
Other therapies
BCL2 is typically overexpressed in FL due to the t(14;18) translocation and plays a key role in its development. Despite the strong rationale for investigating BCL2 inhibitors in FL, venetoclax alone showed a response rate of only 38% in a phase I trial involving 29 patients with relapsed/refractory FL [225]. In the phase II CONTRALTO study, venetoclax and rituximab, with or without bendamustine, were evaluated in 163 patients with relapsed/refractory FL [226]. The ORR for venetoclax and rituximab was 35%, increasing to 84% when bendamustine was added, although with increased toxicity. This finding suggests that while t(14;18) is necessary in the early stages of FL pathogenesis, BCL2 overexpression may not be essential in later stages.
Regarding mTOR inhibitors, temsirolimus achieved OR and CR rates of 54% and 26%, respectively [227]. In a subsequent study, the mTORC1 inhibitor everolimus demonstrated an ORR of 61% in relapsed/refractory FL [228]. It remains unclear whether mTOR inhibitors are more effective in patients with FL harboring mTORC1-activating mutations [24,25,229]. A small study of 21 patients revealed that CREBBP mutations, specifically those affecting the histone acetyltransferase domain, were associated with responses to everolimus or temsirolimus [230]. No correlation between response and mTORC1 pathway mutations was observed, but the number of samples with such mutations was small. Further studies in this subset of patients are warranted, particularly given recent findings suggesting that mTOR pathway mutations define a subset of FLs with distinct pathobiological characteristics [26,230].
Naked antibodies and antibody-drug conjugates are under investigation. Among 34 patients with relapsed/refractory FL, tafasitamab (MOR208) demonstrated an ORR of 29% [231]. The ROMULUS trial included 20 FL patients and evaluated the CD79b-targeting antibody-drug conjugate polatuzumab vedotin, with or without rituximab; the OR and CR rates were 70% and 45%, respectively [232]. In 56 patients with relapsed/refractory FL, polatuzumab vedotin combined with obinutuzumab and lenalidomide showed OR and CR rates of 76% and 63%, respectively [233]. However, in a randomized phase II trial, the addition of polatuzumab vedotin to BR did not improve the response rate [234]. In a phase I trial, the antibody-drug conjugate loncastuximab tesirine achieved an ORR of 79% among 14 evaluable patients with FL [235]. Further research is needed to define the roles of these therapies in FL treatment.
PERSPECTIVES
Treatment options for patients with FL have substantially advanced due to the emergence of immune therapies, improved understanding of immunomodulatory treatments, and introduction of targeted therapies. Several novel therapies are currently in phase III evaluation (Table 3). Therefore, the treatment landscape for FL is expected to evolve to include therapies that are more effective and less toxic than those available at present.
In addition to clinical efficacy, there is increasing recognition of the importance of assessing patient-reported outcomes (PROs) and quality of life (QoL) in patients with FL. Given the favorable outcomes for most patients with FL, balancing disease control with QoL is essential. In a population- based registry, patients with FL receiving immunochemotherapy reported worse QoL scores than a normative population [236]. Declines in QoL measures have also been observed with later lines of therapy [237,238]. Additionally, although PROs are typically collected during clinical trials, they are often underreported, highlighting the need to prioritize patient-centered care [239].
Looking ahead, we expect that the biological basis of treatment response will continue to be investigated, and novel therapies will be developed. These efforts will likely lead to the discovery of predictive biomarkers that enable personalized therapeutic approaches. If novel therapies can reduce early progression and prevent the development of aggressive lymphoma, outcomes for FL are expected to improve.
Notes
Acknowledgments
Dr. Kridel is a Lymphoma Research Foundation Grantee (Jaime Peykoff Follicular Lymphoma Research Initiative).
Conflicts of interest
Research funding (paid to the institution) from Abbvie, Acerta, AstraZeneca, Bristol Myers Squibb and Roche. The author discloses no conflicts.
Funding
None