Characteristics and outcomes of portal vein thrombosis in patients with inflammatory bowel disease in Korea
Article information
Abstract
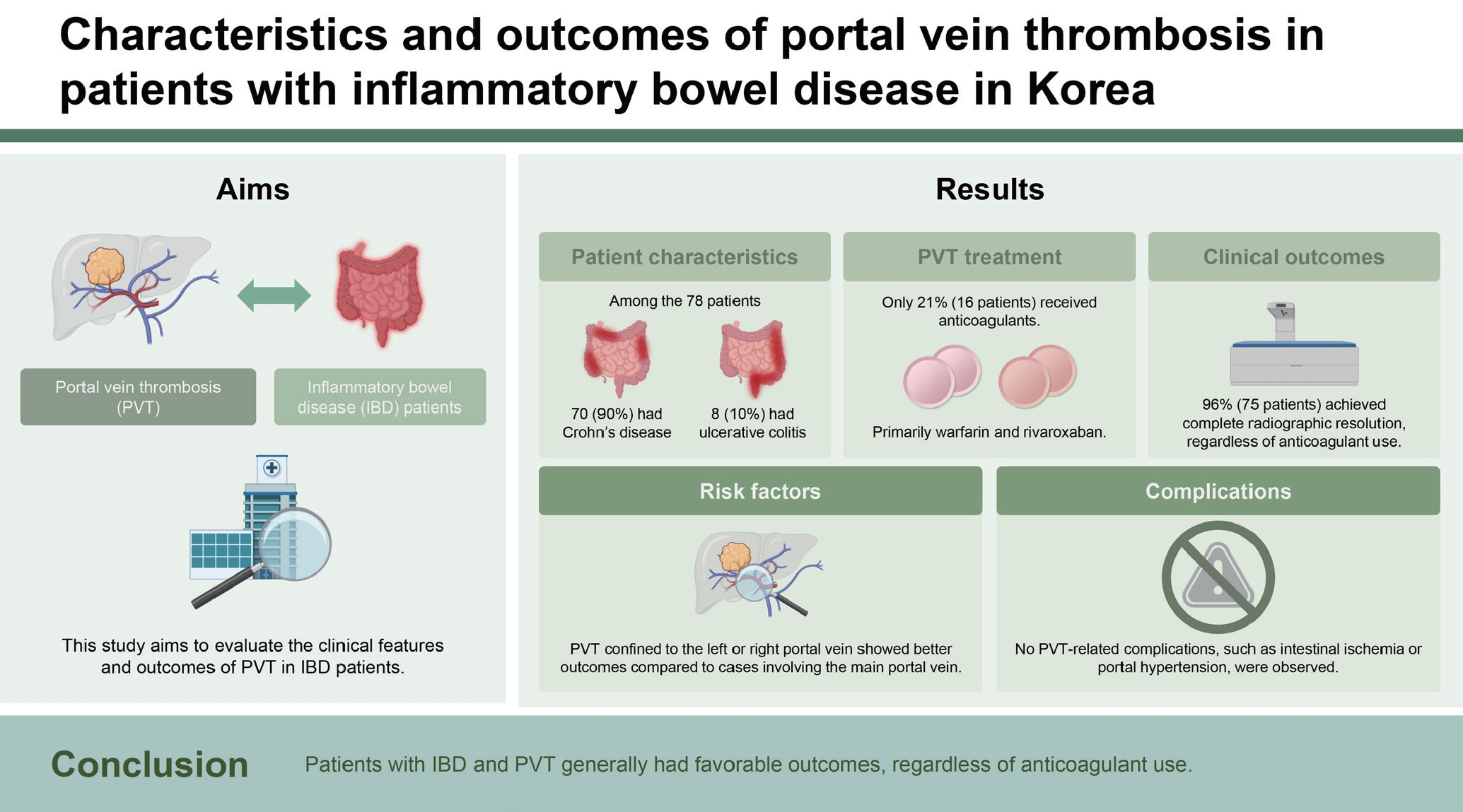
Background/Aims
Portal vein thrombosis (PVT) frequently occurs in patients with inflammatory bowel disease (IBD), particularly when influenced by factors such as abdominal infections, IBD flare-ups, or surgical procedures. The implications of PVT range from immediate issues such as intestinal ischemia to long-term concerns including portal hypertension and its complications. However, there is a notable gap in comprehensive studies on PVT in IBD, especially with the increasing incidence of IBD in Asia. This research aimed to evaluate the clinical features and outcomes of PVT in patients with IBD at a leading hospital in South Korea.
Methods
This retrospective analysis reviewed adult patients diagnosed with both IBD and PVT from 1989 to 2021 at a renowned South Korean medical center. The study focused on patient characteristics, specifics of PVT, administered treatments, and outcomes, all confirmed through enhanced CT scans.
Results
A total of 78 patients met the study’s criteria. Notably, only 20.5% (16/78) were treated with oral anticoagulants; however, a vast majority (96.2%; 75/78) achieved complete radiographic resolution (CRR). When comparing patients receiving anticoagulants to those who did not, a significant preference for anticoagulant use was observed in cases where the main portal vein was affected, as opposed to just the left or right veins (p = 0.006). However, multivariable analysis indicated that neither anticoagulant use nor previous surgeries significantly impacted CRR.
Conclusions
Patients with IBD and PVT generally had favorable outcomes, regardless of anticoagulant use.
INTRODUCTION
Portal vein thrombosis (PVT) manifests in diverse scenarios and shows a heightened incidence, notably among individuals diagnosed with liver cirrhosis. However, it is important to note that PVT can also occur in those without any signs of liver cirrhosis [1]. A myriad of factors contribute to its onset, including intra-abdominal infections, such as diverticulitis, cholecystitis, pancreatitis, abdominal malignancies, and factors such as intra-abdominal surgeries, trauma, thrombophilia, myeloproliferative neoplasms (MPN), and inflammatory bowel disease (IBD) [2].
Specifically, IBD demonstrates a pronounced propensity for venous thromboembolism (VTE) compared to other digestive disorders [3]. Despite the prevalence of this occurrence, the precise etiological mechanism triggering PVT in patients with IBD remains elusive. Prevailing theories suggest that persistent inflammation coupled with intra-abdominal thrombophilia might contribute [2,4,5]. Additionally, there is a hypothesis suggesting that the translocation of gut bacteria into the portal venous system, facilitated by bowel mucosal ulcerations, could lead to portal pyelophlebitis, ultimately resulting in thrombotic events [6].
The risk of PVT in patients with IBD escalates with additional predisposing factors such as intra-abdominal infections, active IBD episodes, or post-operative conditions [7-9]. Moreover, individuals administered steroids prior to surgical interventions or those undergoing emergency surgeries are at an increased risk of developing PVT [10,11].
Neglecting PVT can lead to severe complications. In the short term, it can cause intestinal ischemia or necrosis [12], while over a longer duration, it may lead to portal hypertension, thereby causing complications such as varices and ascites [2,13]. Notably, PVT manifestations in IBD often occur subtly and are primarily identified incidentally [14,15].
Anticoagulation is an effective therapeutic approach for PVT management, emphasizing the importance of prompt treatment initiation to prevent complications [16]. In cases where PVT coincides with liver cirrhosis, a transition from low molecular weight heparin to alternatives such as warfarin or direct oral anticoagulants (DOACs) after treatment initiation is recommended [17]. Approximately half of the affected patients experience complete recanalization [18], whereas spontaneous portal vein (PV) recanalization without anticoagulation is rare in acute PVT cases [19].
Despite the critical nature of anticoagulation in potential PVT scenarios accompanying IBD, research avenues remain relatively limited, especially in Asian contexts. Given the escalating prevalence of IBD in Asia [20,21] and the higher incidence of VTE in Asian IBD demographics compared to their Western counterparts [22], significant research addressing the nuances and prognosis of PVT in Asian IBD cohorts is necessary.
This investigation aims to examine the clinical manifestations and long-term outcomes of PVT among patients with IBD in a major tertiary healthcare facility in South Korea.
METHODS
This study was approved by the Institutional Review Board of Asan Medical Center (approval no. 2022-0062).
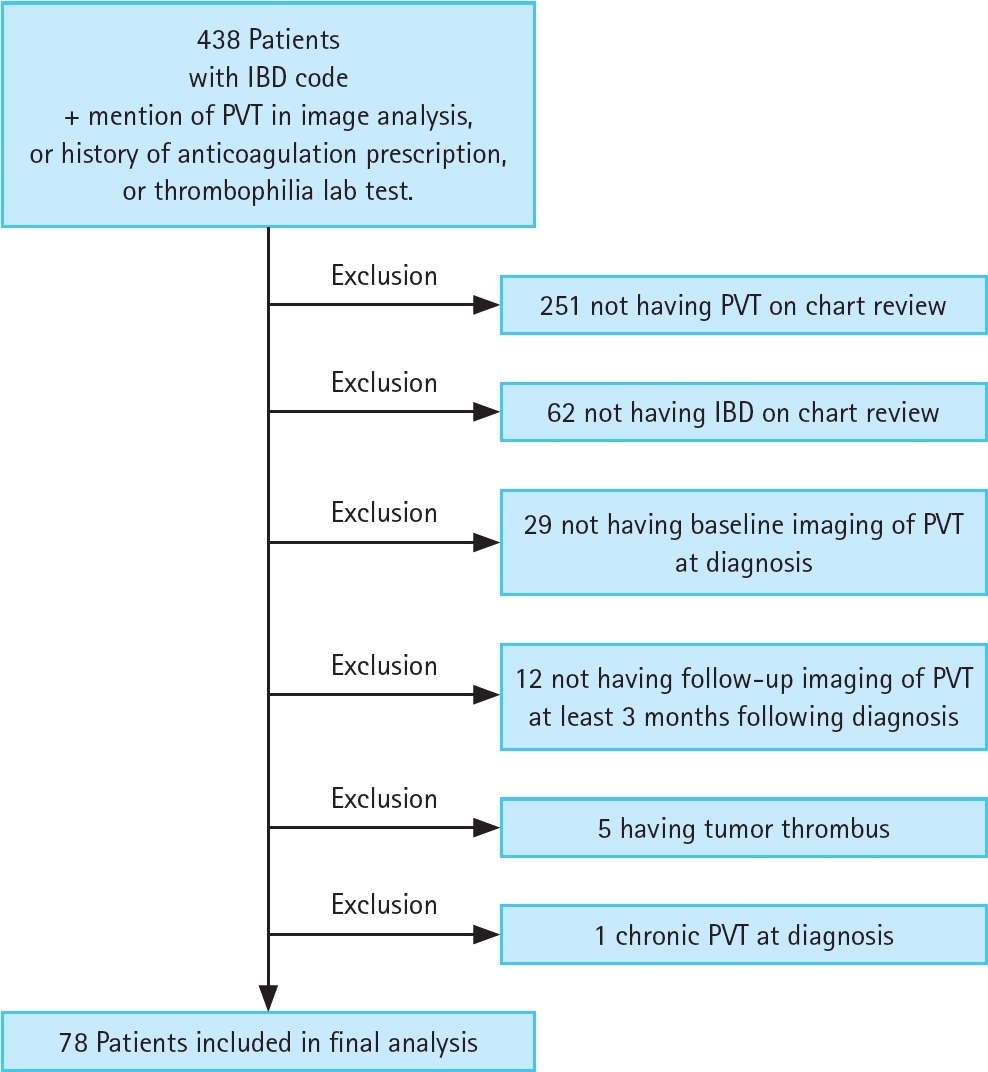
Between June 1, 1989 and December 15, 2021, we retrospectively reviewed patient records at Asan Medical Center in South Korea. We identified individuals aged 18 years and older diagnosed with IBD. Inclusion criteria were based on mentions of PVT in imaging reports, prescription of anticoagulants, or evidence from thrombophilia tests. Patient eligibility was verified via electronic health records.
Exclusion criteria involved patients with a history of tumor thrombosis, thrombolysis, or thrombectomy. Additionally, we excluded patients without baseline imaging at the time of PVT diagnosis, those lacking a minimum of 3-month follow-up imaging post-diagnosis, or those showing signs of chronic PVT. Chronic PVT diagnoses were based on radiological evidence, such as portal cavernomas or portal collaterals, and relevant clinical annotations. The research schematic diagram can be found in Figure 1.
Data collection included parameters such as age at PVT diagnosis, gender, IBD subtype, dates relevant to complete radiographic resolution (CRR), time frames for resolution achievement, last follow-up dates, and duration of follow-up from diagnosis. We also recorded metrics including specifics of anticoagulant therapy, durations of intravenous or subcutaneous bridging, postoperative VTE prophylaxis, comorbidities at diagnosis (e.g., intra-abdominal infections, liver cirrhosis, pancreatitis), symptomatic manifestations, previous VTE events, occurrences of MPN, resultant complications, medication regimens for IBD, relevant laboratory findings, surgical interventions, and imaging details.
Notably, while fecal calprotectin is a marker for assessing IBD activity [23], its omission from routine measurements in our subjects necessitated its exclusion from the analysis. PVT localization was categorized into ‘main PV group’ and ‘left or right PV only group,’ based on the pattern of involvement. Degrees of PVT were classified as either ‘occlusive’ or ‘non-occlusive.’ IBD treatments were segmented into 5-aminosalicylic acid (5-ASA), immunomodulatory agents, steroids, and a category labeled ‘biologics,’ which acknowledged the diverse biologic agents employed in South Korea’s therapeutic landscape [24,25].
For postoperative diagnoses, surgery timelines were classified as ‘recent’ (within 3 months post-diagnosis) or ‘remote’ (beyond 3 months post-diagnosis). In our statistical analysis, patients with ‘remote’ surgery timelines were combined with those without recent surgeries for comparative purposes. Given the variance in anticoagulant use, we compared characteristics of anticoagulant users against non-users, with the primary analytical focus on CRR of PVT.
Statistical evaluations were as follows: Continuous data were presented using medians and interquartile ranges, while categorical variables were expressed as number (%). Comparative evaluations between anticoagulant user groups and non-users utilized the Mann–Whitney test for continuous data and Pearson’s/Fisher’s exact tests for categorical data. To determine odds ratios, multivariable analyses for CRR of PVT employed the Cox proportional-hazards model. Initially planned subgroup analyses based on anticoagulant specifics were omitted due to the limited cohort size.
RESULTS
Patient selection and baseline characteristics
Out of 438 adult patients diagnosed with IBD, 78 met the inclusion criteria based on radiological reports of PVT, anticoagulant prescriptions, or thrombophilia tests. Specifically, 70 patients had Crohn’s disease (CD), and 8 had ulcerative colitis (UC). The average follow-up duration for these patients was 109 months. Table 1 provides a comprehensive overview of their baseline characteristics.
Clinical presentation at PVT diagnosis
The manifestations at the time of PVT diagnosis are detailed in Table 1. A significant number of patients reported concomitant abdominal infections (37.2%) and IBD flares (28.2%). Common symptoms included abdominal pain (70.5%) and diarrhea (44.9%). Less frequently reported symptoms were fever (12.8%) and rectal bleeding (9.0%). The associated symptoms are considered to be related to the underlying IBD or post-surgical conditions. Intriguingly, a subset (9.0%) did not receive any IBD therapy within three months post-diagnosis. Additionally, a substantial 80.8% underwent various surgeries related to IBD within this period.
Diagnostic evaluations and findings
PVT diagnoses were confirmed exclusively through CT imaging, which helped in excluding chronic PVT cases characterized by specific radiographic features such as cavernous transformation. The predominant occurrence of PVT was in the left or right PV, accounting for 94.9% of cases. Notably, all diagnoses were incidental. Thrombophilia evaluations were conducted in 17.9% of patients, revealing no cases of primary thrombophilia. The results of thrombophilia testing can be found in Table 2.
Treatment strategies and management
Regarding therapeutic interventions, 20.5% (16/78) of the patients received oral anticoagulants, mainly warfarin or rivaroxaban. Among these, a significant portion (14 out of 16) underwent bridging therapy with intravenous heparin or subcutaneous enoxaparin before initiating oral anticoagulants. A detailed comparison between anticoagulant users and non-users is presented in Table 3.
Clinical outcomes and prognosis
Throughout the observational period, there were no reported fatalities. However, 2.6% (2 patients) required significant transfusions due to major bleeding episodes. Impressively, the vast majority (96.2%; 75 out of 78) achieved CRR. Figure 2, the Kaplan–Meier curve, illustrates CRR across patient subsets. Furthermore, a multivariable analysis, the results of which can be found in Table 4, aimed at identifying predictors of CRR but did not yield statistically significant results. Notably, no PVT-related complications, such as gut ischemia or portal hypertension, were documented in any patients, including those diagnosed with chronic PVT.
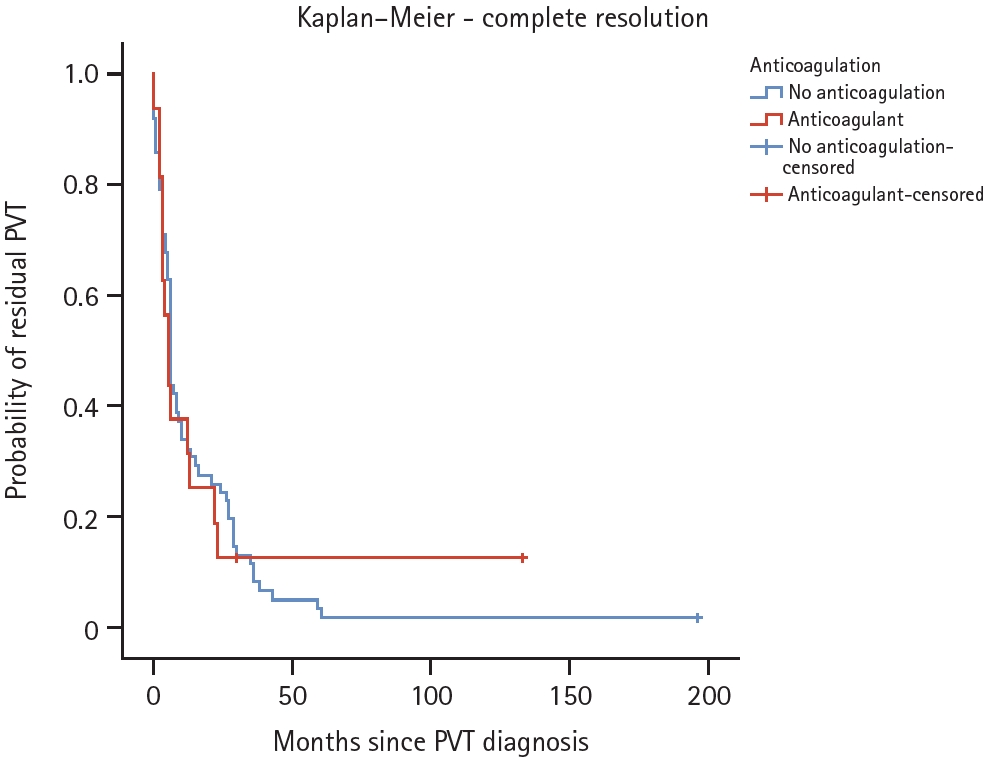
Kaplan–Meier curve for the primary outcome of CRR of PVT by anticoagulation. PVT, portal vein thrombosis; CRR, complete radiographic resolution.
DISCUSSION
PVT is recognized as a common complication in patients diagnosed with IBD [2,4]. This correlation becomes more pronounced when considering factors such as intra-abdominal surgeries, infections, or active IBD flares [7]. The clinical presentation of acute PVT often remains elusive due to its nonspecific symptoms and is frequently identified incidentally [14,15]. While acute PVT poses immediate risks such as intestinal ischemia [12], the chronic form can escalate to severe conditions, including portal hypertension, varices, and ascites [2,13]. A timely initiation of anticoagulation emerges as a cornerstone in managing PVT, and with appropriate therapy, the prognosis remains favorable [16].
Recent studies, including notable research from 2021 conducted at Mount Sinai Hospital in the United States, shed light on the clinical nuances of PVT in patients with IBD. This study evaluated 63 patients with IBD and PVT (26 with CD and 37 with UC). It was found that 92% of these patients received anticoagulation therapy, with 71% achieving CRR. Among the anticoagulants used, DOACs demonstrated higher CRR rates compared to warfarin (96% vs. 55%) and shorter treatment durations (median 3.9 mo vs. 8.5 mo). Conversely, the CRR rate was significantly lower (20%) in patients who did not receive anticoagulation. Additionally, 63% of the patients were on steroids within 3 months of diagnosis, 60% had undergone intra-abdominal surgery within 3 months prior to the diagnosis of PVT, and 68% had involvement of the main PV [26].
Conversely, our investigation, conducted within a prominent tertiary hospital in South Korea, presented a distinct patient profile and outcomes. The predominant IBD subtype was CD in 89.7% of cases, and main PV involvement was notably lower (5.1%). Surprisingly, despite a modest 20.5% of patients receiving anticoagulation, an overwhelming 96.2% achieved CRR.
These discrepancies might be elucidated by patient-specific factors, particularly the distribution of PVT primarily within the right or left PVs (94.9%). This trend could be attributed to the majority (80.8%) of cases being postoperative, where PVT was incidentally detected during routine postoperative imaging, allowing for early detection and management. Given this context, one might speculate that PVT confined to the right or left PVs, especially when discovered incidentally postoperatively, could potentially achieve full remission without anticoagulation. Additionally, regular imaging follow-ups for patients with IBD post-surgery may render shorter anticoagulation durations feasible [27].
Additionally, although steroid use is recognized as a risk factor for the development of PVT [7], the proportion of steroid use in our study was relatively low at 23%. As previously mentioned, our study had a high proportion of patients diagnosed postoperatively, and it is likely that many patients in our hospital discontinued steroid use before surgery based on research suggesting that stopping steroids before surgery can reduce postoperative complications [28].
Moreover, our study results indicated that anticoagulation was used more aggressively in UC patients compared to CD patients. This may be attributed to the recent guidelines recommending anticoagulation for the management of thromboembolism risk in patients with acute severe UC [29], leading to more aggressive anticoagulation therapy in UC patients in clinical practice.
However, some limitations of our study, primarily stemming from its retrospective nature, warrant acknowledgment. Potential biases, especially concerning the non-anticoagulated cohort, could skew interpretations due to the myriad variables at play. The sample size might not have provided adequate power to discern significant differences conclusively. Additionally, the study’s focus did not permit a comparative analysis between warfarin and DOACs, which previous research suggests could be pivotal [26]. Being a single-center study in a tertiary setting, the findings may not universally represent South Korea’s entire IBD patient demographic.
Furthermore, in this study, the number of PVT cases was higher in CD patients compared to UC patients. However, since we do not have data on the overall incidence of PVT in the entire IBD patient pool, we cannot ascertain the exact probability of PVT occurrence in CD versus UC. This limitation should also be considered.
Additionally, in our study, PVT was incidentally discovered in patients, rather than being associated with symptoms related to PVT. A significant proportion of patients (80.8%) were diagnosed within 3 months postoperatively, with a median diagnosis period of only 6 days post-surgery. This suggests that many patients were diagnosed through CT imaging performed shortly after surgery. However, there is currently no established consensus on whether routine CT imaging should be performed postoperatively, indicating a need for further research on this issue.
Despite these constraints, our study significantly contributes to the existing literature by providing insights into the clinical trajectory of patients with IBD and PVT. Given the escalating prevalence of IBD in Asia, our findings underscore the need for further research. The high incidence of partial thrombosis limited to the right or left PVs, even in non-anticoagulated patients, challenges existing guidelines. This observation has profound implications for postoperative patients with IBD, emphasizing the need for heightened awareness of bleeding risk and potentially reshaping current anticoagulation recommendations.
In conclusion, our investigation delved into the attributes and outcomes associated with PVT among patients with IBD in South Korea. The study’s findings highlight promising results where patients demonstrated positive outcomes irrespective of anticoagulation therapy. Given the prevailing guidelines advocating for immediate anticoagulation post-PVT diagnosis, our data prompts a reevaluation. Tailoring treatment strategies based on individual patient-specific variables and the unique characteristics of PVT could potentially enhance therapeutic efficacy and patient outcomes. As such, future studies are imperative to refine and potentially reshape existing clinical recommendations.
KEY MESSAGE
1. This study analyzed the characteristics and prognosis of concurrent PVT in South Korean IBD patients and is of significance due to the favorable outcomes observed regardless of anticoagulation use.
Notes
CRedit authorship contributions
Ki Jin Kim: investigation, data curation, formal analysis, writing - original draft, writing - review & editing; Su Bin Song: investigation, data curation; Jung Bin Park: investigation; June Hwa Bae: investigation; Ji Eun Baek: investigation; Ga Hee Kim: investigation; Min Jun Kim: investigation; Seung Wook Hong: investigation; Sung Wook Hwang: investigation; Dong-Hoon Yang: investigation; Buong Duk Ye: investigation; Jeong-Sik Byeon: investigation; Seung Jae Myung: investigation; Suk-Kyun Yang: investigation; Chang Sik Yu: investigation; Yong-Sik Yoon: investigation; Jong-Lyul Lee: investigation; Min Hyun Kim: investigation; Ho-Su Lee: investigation, Sang Hyoung Park: conceptualization, methodology, resources, investigation, data curation, formal analysis, validation, software, writing - original draft, writing - review & editing, visualization, supervision, project administration, funding acquisition
Conflicts of interest
The authors disclose no conflicts.
Funding
This study was supported by a grant (2023IT0006; 20230269) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea. This study was supported by a grant of the Korean Association for the Study of Intestinal Diseases for 2023 (2023-02).