Growing chronic consolidative lesion with an air bronchogram
Article information
A 60-year-old woman was referred to our hospital for the evaluation of a 2.2 cm-sized focal consolidation with an air bronchogram sign incidentally detected by non-enhanced chest computed tomography (CT) (Fig. 1A). The patient’s medical history, physical findings, and laboratory test results were unremarkable. Contrast-enhanced CT showed a well-enhanced vascular structure (Fig. 1B). Pulmonary arteriography revealed a cut-off sign in the left pulmonary artery (Fig. 1C). Aortography revealed a dilated vascular structure from the left inferior phrenic artery (IPA), and selective angiography confirmed a fistula between the left IPA and left pulmonary vessels (Fig. 1D). Because there were no apparent symptoms, the patient was discharged and scheduled for outpatient follow-up. However, she did not visit for 49 months until she was referred for persistent lesions. Contrast-enhanced CT revealed engorgement of the left IPA with a fistula (Fig. 1E), and selective angiography revealed dilatation of the feeding artery with more prominent collateral vessels (Fig. 1F). Based on these findings, transcatheter embolization of the left IPA was successfully performed. Systemic artery-to-pulmonary vessel fistula (SAPVF) is a rare vascular anomaly for which the disease course is unclear. Although most patients are asymptomatic [1], they can develop life-threatening conditions, such as hemoptysis and pulmonary hypertension [2]. Our case highlights that SAPVF can manifest as a growing chronic consolidative lesion with an air bronchogram, possibly due to dilatation of the pulmonary vessels.
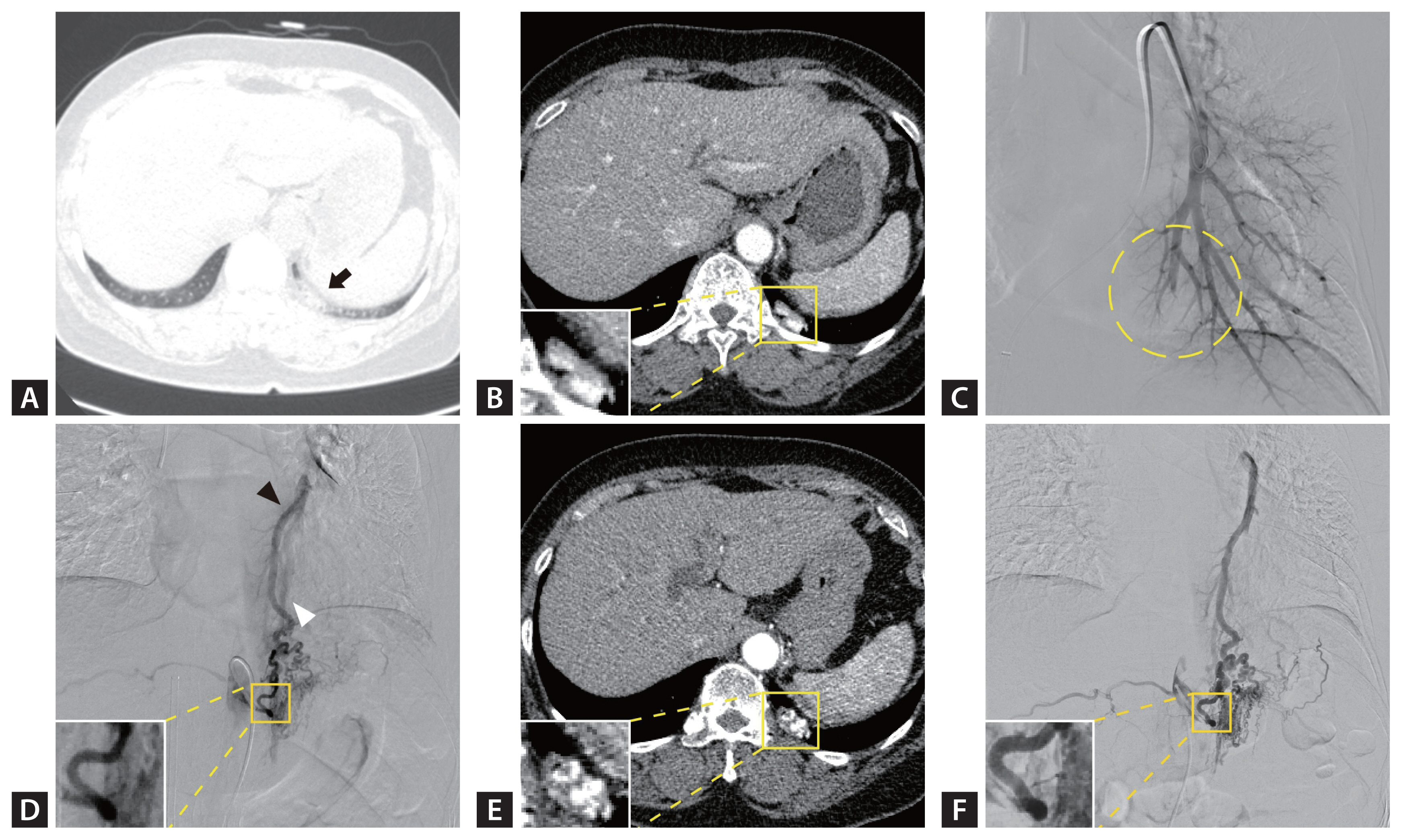
(A) Non-enhanced chest computed tomography (CT) shows a 2.2 cm-sized focal consolidation with an air bronchogram sign (black arrow). (B) Contrast-enhanced chest CT reveals a well-enhanced 24 × 9 mm vascular structure. (C) Pulmonary arteriography shows a cut-off sign distal to the left pulmonary artery (dotted circle). (D) Selective angiography of the inferior phrenic artery (IPA) confirms vascular shunt from the left IPA to the left pulmonary artery (black arrowhead) and vein (white arrowhead). (E) Contrast-enhanced chest CT shows a 25 × 13 mm vascular structure with prominent engorgement of the left IPA compared with previous images. (F) The diameter of the feeding artery has increased and collateral vessels are more prominent than the previous angiogram.
Notes
Conflicts of interest
The authors disclose no conflicts.
CRedit authorship contributions
Jae Seok Jeong: conceptualization, methodology, resources, investigation, formal analysis, validation, writing - original draft, writing - review & editing, supervision, project administration, funding acquisition; Chan Yang Cho: investigation, writing - original draft; Jun Hyung Park: investigation, writing - original draft; Kum Ju Chae: resources, investigation, validation; Yong Chul Lee: conceptualization, methodology, resources, formal analysis, validation, writing - review & editing, supervision, project administration, funding acquisition
Funding
This work was supported by the National Research Foundation of Korea (NRF), funded by the Korean government (MSIT) (No. RS-2024-00356349) and Special Operating Subsidy of Jeonbuk National University Industrial Cooperation Foundation. Funding was also received from Korea Health Technology R&D Project through Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. RS-2024-00440408). Bio&Medical Technology Development Program of the National Research Foundation (NRF) also supported this research, funded by the Korean government (MSIT) (No. RS-2023-00236157). Lastly, this paper was also supported by the Biomedical Research Institute fund at Jeonbuk National University Hospital.
