Effect of abatacept versus conventional synthetic disease modifying anti-rheumatic drugs on rheumatoid arthritis-associated interstitial lung disease
Article information
Abstract
Background/Aims
To compare the effects of abatacept and conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs) on the progression and development of rheumatoid arthritis-associated interstitial lung disease (RA-ILD).
Methods
This multi-center retrospective study included RA patients receiving abatacept or csDMARDs who underwent at least two pulmonary function tests and/or chest high-resolution computed tomography (HRCT). We compared the following outcomes between the groups: progression of RA-ILD, development of new ILD in RA patients without ILD at baseline, 28-joint Disease Activity Score with the erythrocyte sedimentation rate (DAS28-ESR), and safety. Longitudinal changes were compared between the groups by using a generalized estimating equation.
Results
The study included 123 patients who were treated with abatacept (n = 59) or csDMARDs (n = 64). Nineteen (32.2%) and 38 (59.4%) patients treated with abatacept and csDMARDs, respectively, presented with RA-ILD at baseline. Newly developed ILD occurred in one patient receiving triple csDMARDs for 32 months. Among patients with RA-ILD at baseline, ILD progressed in 21.1% of cases treated with abatacept and 34.2% of cases treated with csDMARDs during a median 21-month follow-up. Longitudinal changes in forced vital capacity and diffusing capacity for carbon monoxide were comparable between the two groups. However, the abatacept group showed a more significant decrease in DAS28-ESR and glucocorticoid doses than csDMARDs group during the follow-up. The safety of both regimens was comparable.
Conclusions
Abatacept and csDMARDs showed comparable effects on the development and stabilization of RA-ILD. Nevertheless, compared to csDMARDs, abatacept demonstrated a significant improvement in disease activity and led to reduced glucocorticoid use.
INTRODUCTION
Rheumatoid arthritis-associated interstitial lung disease (RAILD) is a significant cause of mortality and morbidity in patients with RA [1]. ILD occurs in around 20–30% of patients with RA [2]. Older age, male sex, smoking, the presence of rheumatoid factor (RF) or anti-cyclic citrullinated peptide (anti-CCP) antibodies, and high disease activity are associated with RA-ILD [3]. Management of RA-ILD is challenging because of the lack of an established therapy. Although conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) and biologic DMARDs are widely used for the management of joint inflammation, their potential therapeutic effects on RA-ILD are unknown. Indeed, several csDMARDs such as methotrexate (MTX), leflunomide, and tumor necrosis factor (TNF) inhibitors, have been reported to worsen RA-ILD or drug-induced pneumonitis. However, the causal relationship between the use of certain csDMARDs such as MTX and the development of RA-ILD has not been confirmed [4,5].
Accumulating evidence shows that the majority of RA-ILD patients treated with non-TNF inhibitors (abatacept [ABA], rituximab, and tocilizumab) remain stable or improve [6]. In a Spanish retrospective cohort, two-thirds of patients remained stable after a median 9-month treatment with ABA [7]. In another observational multicenter study, 263 patients with RA-ILD were treated with ABA alone, in combination with MTX or with another csDMARD. All three treatment groups experienced stabilization or improvement in lung function and chest high-resolution computed tomography (HRCT) findings, suggesting that ABA therapy with and without csDMARDs is equally effective [8]. The British Society for Rheumatology recommends ABA as a first-line biologic agent for patients with RA-ILD [9]. However, previously published studies were uncontrolled, and uncertainty remains regarding the effect of ABA on the disease course of RA-ILD compared with csDMARDs.
Therefore, in this multicenter observational retrospective study, we aimed to investigate the effect of ABA versus csDMARDs on the progression of preexisting ILD and the development of ILD in patients with RA.
METHODS
Study design and population
This multi-center, retrospective, observational study included RA patients aged 19–75 years who were treated with ABA or csDMARDs at 10 referral hospitals in South Korea between March 2006 and February 2020. All patients were diagnosed with RA according to the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria [10] or 1987 ACR classification criteria [11]. ABA was administered at a standard dose intravenously (10 mg/kg/4 wk) or subcutaneously (125 mg/wk). The ABA group received different treatment modalities including ABA monotherapy, ABA combined with MTX, and ABA combined with non-MTX csDMARDs. csDMARDs included MTX, leflunomide, sulfasalazine, hydroxychloroquine, and tacrolimus.
The study inclusion criteria were as follows: (1) patients with RA-ILD who had undergone at least two pulmonary function tests (PFTs) and/or HRCT scans, the first within 3 months before the initiation of ABA or csDMARDs, and the second after a follow-up interval of at least six months. (2) Patients without RA-ILD at the initiation of ABA or csDMARDs who had undergone at least two HRCT scans, the first at baseline and the second after a follow-up interval of at least six months Patients with other connective tissue diseases, incomplete clinical data, or history of malignancy or radiation therapy were excluded. This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Soonchunhyang University Seoul Hospital (IRB Number: 2020-03-020). The requirements for patient approval and informed consent were waived by the IRB Board due to the retrospective nature of the study and the fact that only anonymous clinical data were used for analysis.
Data collection
At the start of treatment with ABA or csDMARDs, baseline data were collected from the medical records, including demographics, clinical data (disease duration, 28-joint Disease Activity Score with the erythrocyte sedimentation rate [DAS28-ESR], body mass index, and smoking history), presence of anti-CCP and RF, and treatment-related records. Among the enrolled patients, a diagnosis of RA-ILD was established based on HRCT findings.
In patients with RA-ILD at baseline, the forced vital capacity (FVC), diffusing capacity for carbon monoxide (DLCO) (corrected for hemoglobin), and HRCT data were obtained at the start of the study (within 3 months before the administration of ABA or csDMARDs) and the most recent follow-up to evaluate the progression of RA-ILD. In patients without RA-ILD at baseline, HRCT data were obtained at the start of the study (within 3 mo before the administration of ABA or csDMARDs) and the most recent follow-up to evaluate the development of RA-ILD.
Outcome measures
The main variables were the effects of ABA and csDMARDs according to the outcome of ILD at the end of follow-up in patients with RA-ILD with respect to the following factors: (1) progression (meeting any of the following criteria: a decline in FVC of ≥ 10%, a decline in FVC of 5–10% with a decline in DLCO of 15%, or increased extent of fibrosis on HRCT during the follow-up period) [12,13]); (2) non-progression (stabilization or improvement; a decline in FVC < 10% and in DLCO < 15% and no radiological progression); and (3) death. In patients without baseline RA-ILD, the development of RA-ILD was compared between ABA and csDMARDs. The follow-up period was from the date of baseline HRCT or PFT until the date of progression, new development of RA-ILD, discontinuation of ABA or csDMARDs, initiation of a new biologic or targeted synthetic DMARD, last follow-up HRCT or PFT, or death. Switching between different csDMARDs or between ABA monotherapy and ABA plus csDMARDs was not a censoring event. Drug discontinuation was defined as the absence of dispensing within 90 days of the expected refill date.
At each center, one or two board-certified thoracic radiologists independently assessed the chest HRCT images [8]. In addition, the presence and progression of ILD were evaluated. ILD was classified into nonspecific interstitial pneumonia (NSIP), usual interstitial pneumonia (UIP), or other (bronchiolitis obliterans, organizing pneumonia, lymphocytic interstitial pneumonitis, and mixed patterns) [14].
We also collected data on the discontinuation of ABA or csDMARDs, reasons for discontinuation, and adverse events including infection, hospitalization, reason for hospitalization, and development of malignancy. Information regarding mortality and causes of death was obtained from a review of medical records.
Statistical analysis
Statistical analyses were performed using SPSS (version 22.0; IBM Corp., Armonk, NY, USA) and R (version 3.6.2). Continuous variables were expressed as mean (standard deviation) or median (interquartile range [IQR]), and categorical variables were presented as frequencies and proportions. Intergroup comparisons were conducted using Student’s t-test or the Mann–Whitney U test for continuous variables, while categorical data were compared using the chi-square test or Fisher’s exact test. Longitudinal changes in FVC, DLCO, DAS28-ESR, and glucocorticoid dose were compared between the ABA and csDMARDs groups using a generalized estimating equation (GEE). Logistic regression analysis was used to identify the prognostic factors for the progression of RA-ILD. p values < 0.05 were considered statistically significant.
RESULTS
Baseline characteristics
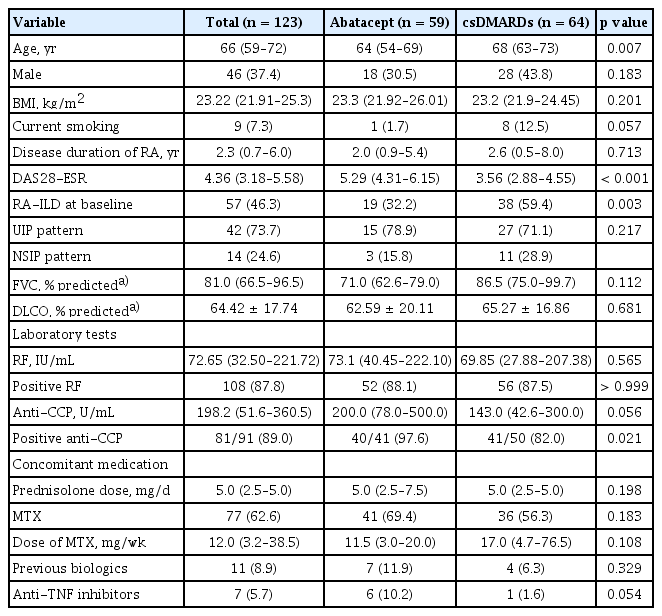
A total of 123 patients with RA were included in a retrospective multi-center cohort, with 59 receiving ABA and 64 receiving csDMARDs. The baseline characteristics of the patients are shown in Table 1. The median (IQR) follow-up periods with ABA (24.0 mo [14.5–40.5 mo]) were longer than those with csDMARDs (20.5 mo [12.0–33.8 mo]) (p = 0.039). The ABA group had a younger average age (64 vs. 68 yr) (p = 0.007), higher DAS28-ESR at baseline (5.29 vs. 3.56) (p < 0.001), and higher positivity for anti-CCP (97.6% vs. 82.0%) (p = 0.021) than the csDMARDs group. Nineteen (32.2%) patients treated with ABA and 38 (59.4%) patients treated with csDMARDs had RA-ILD at baseline. The most common HRCT pattern observed was UIP (73.7%), followed by NSIP (24.6%).
In the ABA group, 41 patients (69.5%) received ABA plus MTX, 11 (18.6%) received ABA plus non-MTX csDMARDs (hydroxychloroquine [n=7], leflunomide [n=1], and sulfasalazine [n=3]), and 7 (11.9%) received ABA monotherapy. Among patients with baseline RA-ILD treated with ABA, 5 (26.3%) were treated with ABA monotherapy and 9 (47.4%) received ABA plus MTX. ABA was the first biologic prescribed in 52 patients (88.1%), while 7 had prior experience with biologics (6 with TNF inhibitors and one with tocilizumab).
In the csDMARDs group, MTX was the most prescribed drug (MTX monotherapy: 8 patients, MTX in combination with other csDMARDs: 32 patients). Monotherapy with leflunomide, hydroxychloroquine, and tacrolimus was administered to 4 (6.3%), 10 (15.6%), and 6 (9.4%) patients, respectively. The detailed use of csDMARDs is shown in Supplementary Table 1.
Almost all patients (98.3% treated with ABA and 95.3% treated with csDMARDs) were taking glucocorticoids at a median prednisolone equivalent dose (IQR) of 5.0 mg/d (2.5–5.0 mg/d). No patients in either group received antifibrotic medication.
Development and progression of RA-ILD
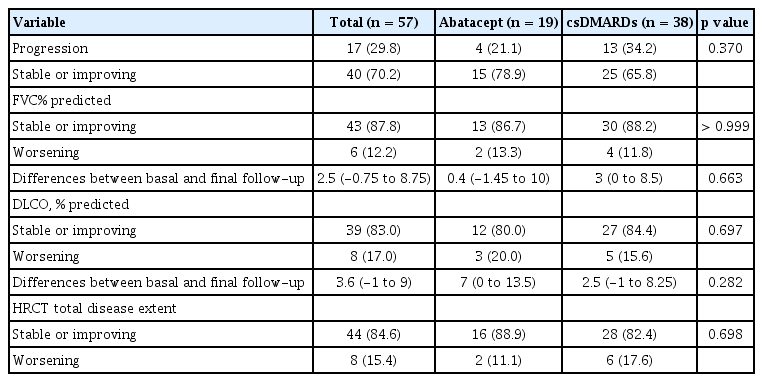
Among patients with RA without ILD at baseline, new RA-ILD developed in one patient who received triple csDMARDs (MTX, sulfasalazine, and hydroxychloroquine) for 32 months without any change in medication. In patients with RA-ILD at baseline, the median (IQR) follow-up duration was 21 months (13–37 mo). At the end of follow-up, over 80% of patients with RA-ILD had stabilized or improved lung function and HRCT extent of fibrosis in both the ABA and csDMARDs groups (Table 2). Overall, 4/19 (21.1%) patients in the ABA group and 13/38 (34.2%) in csDMARDs group showed progression of RA-ILD.
In patients with RA-ILD at baseline, longitudinal changes in FVC and DLCO were evaluated using GEE analysis, which considered repeated measurements throughout the follow-up period (Fig. 1). Although the ABA group had a lower baseline FVC than the csDMARDs group (71.0% vs. 86.5%, p = 0.112), both groups demonstrated a trend towards stabilized FVC over time (Fig. 1A). Moreover, both groups also showed a stabilized DLCO over time (Fig. 1B). In GEE analysis, no difference in longitudinal changes in lung function was found between the ABA and csDMARDs groups.
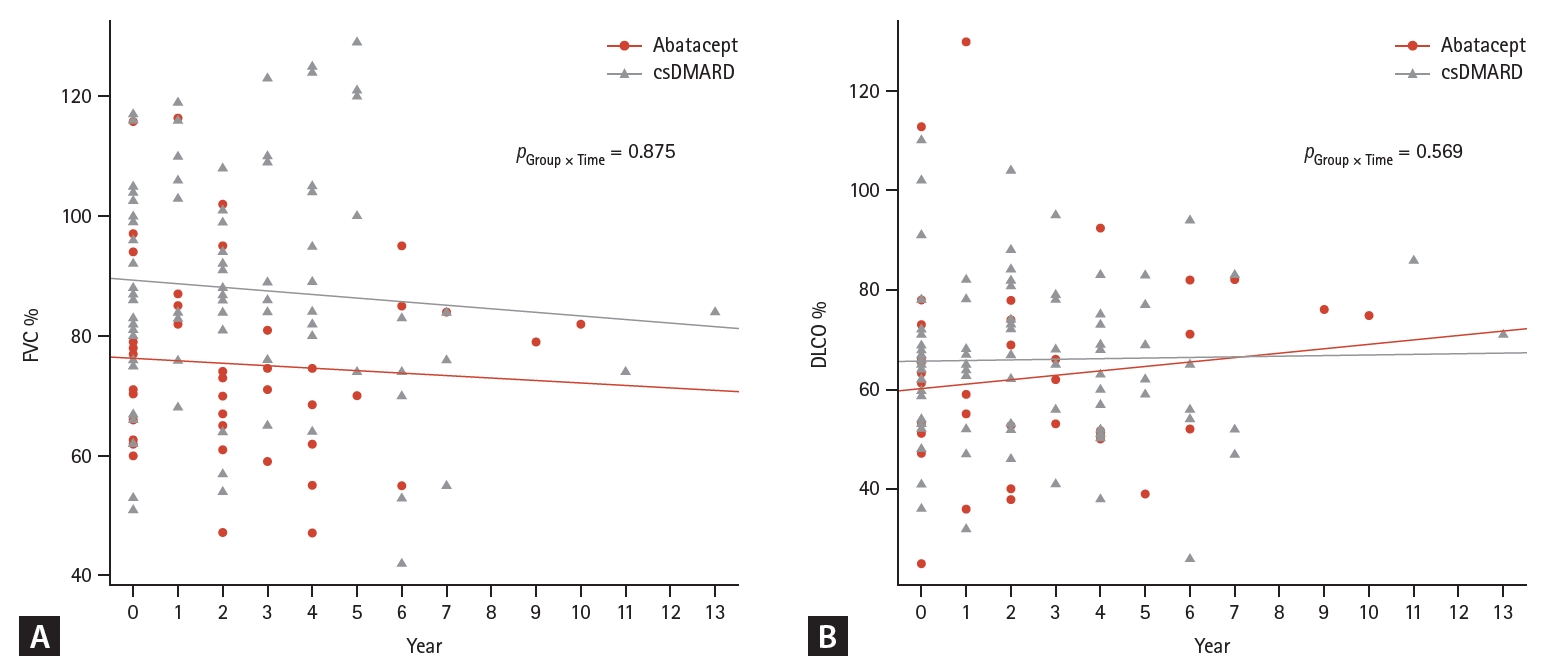
Changes in lung function during the follow-up period. FVC (A) and DLCO (B) were measured during the follow-up. csDMARD, conventional synthetic disease-modifying anti-rheumatic drug; DLCO, diffusing capacity for carbon monoxide; FVC, forced vital capacity; pgroup X time, p value for generalized estimating equation analysis.
Univariate logistic regression analysis showed that age was associated with progression of RA-ILD (OR, 1.147; 95% CI, 1.028–1.279; p = 0.014). However, other variables, including smoking, male sex, FVC and DLCO at baseline, DAS28-ESR at baseline and last follow-up, UIP HRCT pattern, levels of RF and anti-CCP, and use of ABA and MTX, were not associated with the progression of RA-ILD.
Disease activity and glucocorticoid sparing effect
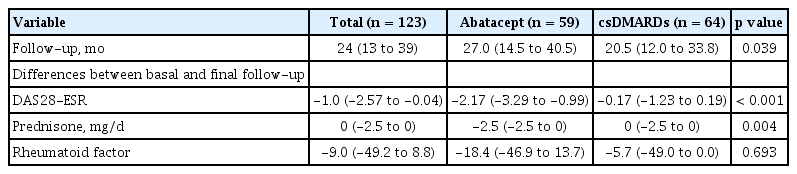
Among all patients with and without RA-ILD, the ABA group had a significantly higher DAS28-ESR than the csDMARDs group (5.4 vs. 3.8) (p < 0.001). The median follow-up duration was significantly longer in the ABA group compared with the csDMARDs group (27.0 vs. 20.5 mo) (p = 0.039) (Table 3). At the end of follow-up, ABA group showed a significant decrease in DAS28-ESR (-2.17 vs. -0.17) (p < 0.001) and higher reduction of glucocorticoid dose than the csDMARDs group (-2.5 mg/d vs. 0 mg/d) (p = 0.004). Longitudinal analysis also showed a significant improvement in disease activity (p < 0.001) and the glucocorticoid-sparing effect of ABA compared to csDMARDs (p < 0.001) (Fig. 2).
Differences in DAS28-ESR, dose of prednisolone, and rheumatoid factor between the two treatment groups
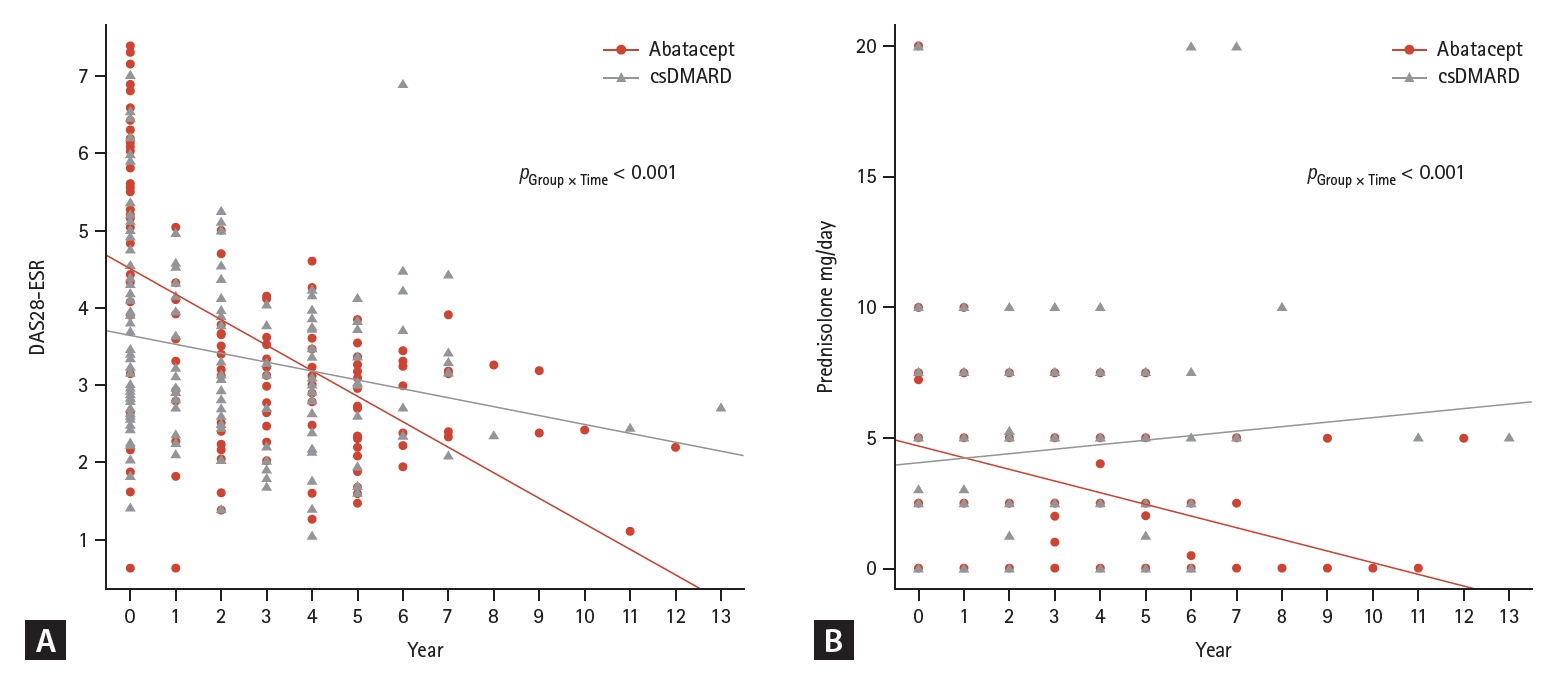
Changes in disease activity and glucocorticoid dose during the follow-up. The DAS28-ESR (A) and daily prednisone dose (B) are shown during the follow-up. csDMARD, conventional synthetic disease-modifying anti-rheumatic drug; DAS28-ESR, 28-joint Disease Activity Score with the erythrocyte sedimentation rate; pgroup X time, p value for generalized estimating equation analysis.
Adverse events
Thirty-one of the 123 patients (25.2%) were admitted to the hospital at least once. A total of 12/123 (9.8%) patients required hospitalization due to infection (10 for bacterial pneumonia, one for Pneumocystis jirovecii pneumonia, and one for influenza). One patient in the csDMARDs group and one patient in the ABA group were diagnosed with non-small cell lung cancer during the follow-up period. One patient was treated with MTX for 58 months and was admitted to the hospital because of acute exacerbation of RA-ILD. No significant differences were observed in the frequency of adverse events.
The csDMARDs group had a higher discontinuity rate than the ABA group (17.2% vs. 6.8%), with marginal statistical significance (p = 0.078). In the ABA group, four of 59 patients discontinued treatment during the follow-up: 2 due to RA flares, one due to pneumonia, and one owing to the occurrence of lung cancer. Two patients treated with ABA plus csDMARDs switched to ABA monotherapy because of their improved disease activity. In the csDMARDs group, 11 of 64 patients discontinued treatment during the follow-up: 5 due to RA flare, one due to acute exacerbation of RA-ILD, one owing to pneumonia, one owing to the occurrence of lung cancer, 2 owing to gastrointestinal discomfort, and one owing to MTX-induced cytopenia. Four patients treated with two or three csDMARDs discontinued one agent owing to an improvement in disease activity. Details of csDMARD use at the final follow-up is presented in Supplementary Table 2.
DISCUSSION
The present study showed a comparable rate of ILD progression and development among RA patients treated with ABA and csDMARDs during a median follow-up period of 21 months. RA-ILD stabilized or improved in 78.9% of patients treated with ABA, which is consistent with previous studies [15]. Our study had a similar design (retrospective multicenter observational) and baseline characteristics to a recently published Italian study [16]. Regarding baseline characteristics, both studies were characterized by similar patient ages (65 yr), high seropositive rates of RF and anti-CCP (approximately 90%), and similar follow-up periods (26 mo). The baseline FVC in patients with RA-ILD treated with ABA was lower in our study than in the study by Cassone et al. [16] (71% vs. 89%). In both studies, approximately 25% of patients received ABA monotherapy, and MTX was the most prescribed combination drug with ABA (38.6% in the Cassone et al. study [16], and 47.4% in our study). The effects of ABA on ILD were similar in both studies; FVC, DLCO, and HRCT remained stable or improved in > 80% of patients.
We compared the effects of ABA on RA-ILD with those of csDMARDs. In the csDMARDs group, 65.8% of RA-ILD patients were stabilized or improved. In patients with RAILD, variations in the baseline characteristics could have affected the comparison of lung function outcomes between the ABA and csDMARD groups. ABA group had a longer follow-up duration (27.0 mo vs. 20.5 mo, p = 0.039) and lower baseline FVC than the csDMARDs group (71.0% vs. 86.5%, p = 0.112). In contrast, our analysis showed that age was associated with RA-ILD progression, and patients in the csDMARD group were older than those in the ABA group (mean age, 64 yr vs. 68 yr; p = 0.007). ABA is a fusion protein composed of the Fc region of human IgG1 fused to the extracellular portion of the cytotoxic T lymphocyte-associated antigen 4 that selectively inhibits T cell activation [17]. Autoantibody-mediated neutrophil activation is considered as one of the main pathogeneses of RA-ILD. Therefore, biological agents targeting adaptive immune responses, such as ABA, could be potential treatments for RA-ILD because ABA significantly lowers the titers of anti-citrullinated protein antibodies, and seropositivity is associated with the increased effectiveness of ABA [6,18]. In the present study, all patients were seropositive; therefore, we could not compare the effects of ABA according to seropositivity status. When comparing the effects of ABA on RA-ILD with those of TNF-inhibitors, two observational studies showed that ABA resulted in a lower rate of RA-ILD worsening than TNF inhibitors [19,20]. The present study showed a significant difference in RA disease activity and steroid-sparing effects between ABA and csDMARDs; however, ABA was not superior to csDMARDs for RA-ILD. Further comparative studies between ABA and various DMARDs are needed to confirm the effect of ABA on RA-ILD.
MTX is a cornerstone DMARD used in the management of RA. Whether MTX exposure increases the risk of RA-ILD incidence and progression of RA-ILD is controversial. A retrospective cohort study conducted in Japan showed that MTX use (OR, 12.75) was significantly associated with worsening ILD in patients with RA treated with ABA [21]. In contrast, other studies conducted in Caucasian patients with RA suggested that MTX use is not associated with an increased risk of RA-ILD [5]. Moreover, a retrospective cohort study reported that MTX use was actually a protective factor for lung function (OR, 0.27) in RA-ILD [22]. A recent meta-analysis of cohort studies revealed that MTX significantly reduces RA-ILD induced mortality [23]. In our study, approximately 70% of patients in the ABA group received ABA combined with MTX. However, we did not find an association between MTX use and ILD progression in Korean RA patients, suggesting that the discordant results in the combination of ABA with MTX cannot be explained simply by ethnic differences between Caucasians and Asians. Further studies are required to determine whether the use of MTX in combination with ABA is a beneficial strategy for RA-ILD.
Regarding the risk of inducing ILD, data from post-marketing surveillance and pooled analysis of safety data from 8 clinical trials of ABA showed a low incidence rate of ILD, ranging from 0.09% to 0.31% [24,25]. In post-marketing surveillance, the mean onset (min-max) of ABA-induced ILD was 101.5 days (22–183 d). Consistent with previous studies, we did not observe newly developed ILD in RA patients treated with ABA for a median duration of 26 months. We observed only one case of newly developed ILD that was treated with triple csDMARDs for 32 months. The course of ILD does not have an acute or subacute onset, suggesting an incidental RA-ILD and not MTX-induced pneumonitis [5]. ABA also showed a good safety profile and retention rate compared with csDMARDs. However, further prospective cohort studies are required to confirm these findings becausewe included patients with RA who underwent at least two spirometry and/or HRCT examinations, which may have led to selection bias. The reasons for undergoing follow-up chest CT in patients without RA-ILD were as follows: suspected symptoms of ILD (n = 12), monitoring of lung nodules (n = 4), screening for RA-ILD based on the clinician’s judgement (n = 39), and unknown (n = 11).
Our study has limitations due to its retrospective design, variable follow-up periods, varying ILD statuses, and relatively short follow-up time. Recently, progressive pulmonary fibrosis (PPF) was defined as the presence of at least two of the following three criteria: patients with ILD with worsening respiratory symptoms, functional decline, and radiological progression within 12 months [26]. Monitoring ILD using spirometry has limitations due to visit-to-visit variability and various factors impacting the results [27]. However, serial measurements are important for assessing disease progression in ILD. In the present study, 52.6% (30/57) of patients with RA-ILD underwent baseline and only one follow-up spirometry. However, patients with progressive RA-ILD on HRCT had significant decline in FVC (median -5% [IQR, -7.75 to 0.25] vs. 2% [IQR, 0 to 8], p < 0.05) and DLCO (median -3% [IQR, -15.5 to -1] vs. 3% [IQR, -15.5 to -1.0], p < 0.01) compared to that in those without progression, reflecting correlation between PFTs and HRCT findings. Before the recent guidelines for PPF, few studies defined progressive ILD as a decline in FVC and/or increased fibrosis on HRCT within 24 months [28,29]. A large European retrospective study demonstrated a progressive pattern in 38% of patients with RA-ILD at the 2-year follow-up [30]. Similarly, nearly 30% of patients with RA-ILD showed progression during the median follow-up of 21 months in the present study. Most patients with fibrotic ILD experience disease progression several years after the diagnosis of ILD. Therefore, further long-term cohort studies are needed to reveal the heterogeneity in the course of RA-ILD, even after satisfying the PPF criteria. Another potential limitation is the relatively small number of patients with RA-ILD. Finally, a quantitative or semi-quantitative assessment of HRCT was missing. Radiologists at each institution evaluated only the presence of ILD, and the pattern and deterioration of ILD-related fibrosis. In total, 221 HRCT scans were reviewed. Two thoracic radiologists reviewed 55 HRCT scans by consensus and were blinded to the clinical and PFT results, whereas the other HRCT scans were independently reviewed by one radiologist per centre. Although expert thoracic radiologists assessed ILD progression on HRCT, we did not evaluate the inter-reader agreement.
In conclusion, ABA and csDMARDs have comparable effects on the development and stabilization of RA-ILD. However, a substantial improvement in disease activity and glucocorticoid-sparing effect was observed with ABA compared to csDMARDs.
KEY MESSAGE
1. During the median follow-up of 21 months, RAILD progressed in 21.1% of patients with RA treated with ABA and in 34.2% of those treated with csDMARDs without significant difference.
2. ABA and csDMARDs showed comparable effects on development and stabilization of RA-ILD.
3. A significant improvement in disease activity and glucocorticoid-sparing effect was observed in the ABA group compared with the csDMARDs group.
Notes
CRedit authorship contributions
Kyung-Ann Lee: data curation, formal analysis, validation, software, writing - original draft, writing - review & editing, visualization; Bo Young Kim: investigation, data curation; Sung Soo Kim: investigation, data curation; Yun Hong Cheon: investigation, data curation; Sang-Il Lee: investigation, data curation; Sang-Hyon Kim: investigation, data curation; Jae Hyun Jung: investigation, data curation; Geun-Tae Kim: investigation, data curation; Jin-Wuk Hur: investigation, data curation; Myeung-Su Lee: investigation, data curation; Yun Sung Kim: investigation, data curation; Seung-Jae Hong: investigation, data curation; Suyeon Park: formal analysis, software; Hyun-Sook Kim: conceptualization, methodology, resources, investigation, supervision, project administration, funding acquisition
Conflicts of interest
The authors disclose no conflicts. Bristol Myers Squibb Pharmaceutical Company played no role in the study design, collection, analysis, or interpretation of the data, or writing of the manuscript.
Funding
This research was supported by a grant from the Soonchunhyang University Research Fund, Bristol Myers Squibb Pharmaceutical Company (Seoul, Korea) and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC21C0100).